Published online Jun 28, 2006. doi: 10.3748/wjg.v12.i24.3887
Revised: January 6, 2006
Accepted: January 14, 2006
Published online: June 28, 2006
AIM: To review and evaluate our experience in laparo-scopic cholecystectomy.
METHODS: A retrospective analysis was performed on data collected during a 13-year period (1992-2005) from 1220 patients who underwent laparoscopic cho-lecystectomy.
RESULTS: Mortality rate was 0%. The overall morbidity rate was 5.08% (n = 62), with the most serious complications arising from injuries to the biliary tree and the cystic artery. In 23 (1.88%) cases, cholecystectomy could not be completed laparoscopically and the operation was converted to an open procedure. Though the patients were scheduled as day-surgery cases, the average duration of hospital stay was 2.29 d, as the complicated cases with prolonged hospital stay were included in the calculation.
CONCLUSION: Laparoscopic cholecystectomy is a safe, minimally invasive technique with favorable results for the patient.
- Citation: Vagenas K, Karamanakos SN, Spyropoulos C, Panagiotopoulos S, Karanikolas M, Stavropoulos M. Laparoscopic cholecystectomy: A report from a single center. World J Gastroenterol 2006; 12(24): 3887-3890
- URL: https://www.wjgnet.com/1007-9327/full/v12/i24/3887.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i24.3887
Laparoscopic cholecystectomy was first introduced by Muhe in 1986[1], and has now evolved to the point where it has replaced the open technique in many medical centers around the world. Today, laparoscopic cholecystectomy, rather than the open technique, is considered as the treatment of choice for gallstone disease[2-5].
Perceived advantages of laparoscopic cholecystectomy, compared with the open technique, include earlier return of bowel motility, less post-operative pain, better cosmetic result and shorter hospital stay resulting in equal or lower hospital costs, as documented by various randomized control trials[6-9].
At the university hospital of Patras, we performed our first laparoscopic cholecystectomy on September 1992. Since then, a total of 1220 laparoscopic cholecystectomies have been performed. As our surgeons are increasingly familiar with it, laparoscopic cholecystectomy has become the most common operation in our daily practice.
This is a retrospective study that involves data collection from medical records of patients undergoing laparoscopic cholecystectomy. Data collection for this research project was approved by the Ethics Committee. The Department of Surgery at the University Hospital of Patras maintains medical records for all patients who have an operation in this institution since the hospital opened in 1988. Our records include paper-only charts up to 1999, and electronic records since then. The records of all patients who underwent laparoscopic cholecystectomy between September 1992 and September 2005 in our institution were retrieved. During this period, a total of 1220 patients underwent laparoscopic cholecystectomy. The female to male ratio was 3:1 (907 vs 313) and the mean patient age was 53.3 (range 16-86) years.
Data recorded included demographic information, past medical history, diagnosis and indication for the operation, name of surgeon and anesthesiologist, duration of the operation, peri-operative and post-operative complications, time to return of bowel function, oral intake and ambulation, postoperative pain and hence further need for analgesics and length of hospital stay. The recorded perioperative complications included subcutaneous emphysema, pneumothorax, bleeding, hemodynamic instability, myocardial ischemia, injury to the biliary tree or the cystic artery.
Postoperative complications included re-operation, ileus, fever, atelectasis, pneumonia, wound infection, incisional hernia, myocardial ischemia or infarction, unplanned ICU admission or death. Data were entered into a computerized database for further analysis. Most patients (86.3%) presented uncomplicated biliary colic. The remainder had symptoms of acute cholecystitis, pancreatitis and cholangitis. All patients had an ultrasound of the upper right abdominal quadrant and, in selected cases, an ERCP was performed before the operation.
All patients scheduled for elective cholecystectomy were admitted the day before, and were allowed to have food and liquids until 6 h before the operation.
The operation was performed with the standard four-port technique, using carbon dioxide for peritoneal cavity insufflation. For the first 283 cases, the Veres technique was used to obtain pneumoperitoneum. Thereafter and for the subsequent cases, we preferred the Hasson technique. Following gallbladder removal, drains were placed selectively in difficult cases where there was a risk of postoperative bleeding. All patients wore anti-embolic stockings and received low molecular heparin subcutaneously. Antibiotic prophylaxis was ensured with 3 peri-operative doses of first generation cephalosporin intravenously. The administration of heparin continued postoperatively, until the discharge of the patient from the hospital. The average time of the operation was 72 (range 50-102) min.
All procedures were performed under general endotracheal anesthesia. The anesthetic regimen was not standardized, but was tailored to the needs of each patient, as determined by the attending anesthesiologist. All patients were NPO (nil per os) after midnight, or, for cases done later in the day, for at least 6 h before the operation. All medications, except anti-platelet agents or anticoagulants, were continued until the morning of surgery. Before induction of anesthesia, patients were premedicated with intravenous ranitidine 50 mg, and midazolam 2-5 mg, depending on age, gender and preoperative anxiety. Most patients received an antiemetic (metoclopramide or ondansentron) to prevent post-operative nausea and/or vomiting. Anesthesia was induced with intravenous administration of 50-100 μg of fentanyl, followed by intravenous propofol (2 mg/kg) or thiopental (3-5 mg/kg). Muscle relaxation was accomplished with a non-depolarizing relaxant (vecuronium 0.1 mg/kg or rocuronium 0.5 mg/kg). After intubation, anesthesia was maintained, in most cases, with inhaled agents (isoflurane, sevoflurane or desflurane in an air/oxygen mixture), although TIVA with opioids and propofol infusion at 100-200 μg/kg per min was occasionally used. After its introduction to the market, remifentanil was widely used, combined with propofol or an inhaled agent, to provide intra-operative analgesia. Analgesia was accomplished with intravenous fentanyl in the early part of the procedure, followed by intravenous or intramuscular meperidine (25-50 mg) towards the end. In addition, patients who exhibited severe pain also received NSAID as an adjuvant analgesic. At the end of the procedure, all port sites were injected with 5 g/L bupivacaine (total of 10 mL). Additional meperidine or morphine was given in the recovery room if required, based on patient VAS pain score. All patients received an intravenous infusion of 1-2 L of crystalloid solution during the operation. Patients who could not tolerate pneumoperitoneum, or in cases where urine output was less than 0.5 mL/kg per hour, additional colloid (60 g/L hetastarch 500 mL) was administered, to ensure adequate patient hydration.
Post-operative analgesia was achieved with acetaminophen (po, 500 mg 4 times a day), and oral codeine/acetaminophen combinations (30-60 mg 4 times daily). Additional metoclopramide or ondansentron was administered if nausea or vomiting persisted postoperatively. All patients had oral liquids and were encouraged to proceed with food in the evening after the operation, provided there was no nausea or vomiting.
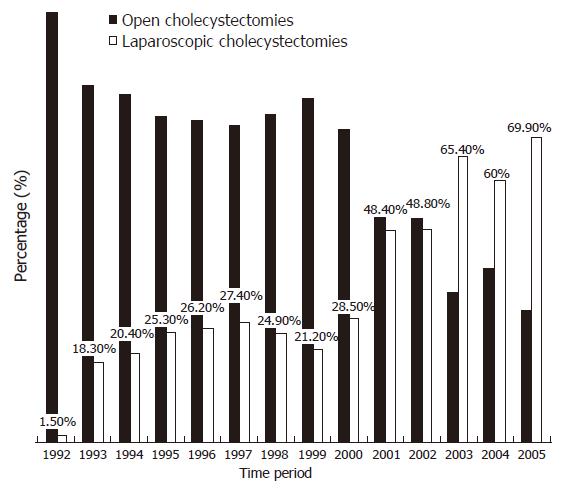
Today laparoscopic cholecystectomy has become the golden rule for the treatment of gallstone disease. In our clinic, the laparoscopic approach was initially reserved for the uncomplicated cases. However, as experience was accumulated and our surgeons became more familiar with the technique, even more complicated cases were treated laparoscopically. In 1994, 18.1% of all cholecystectomy procedures (53 cases) in our institutions were performed laparoscopically. This percentage kept increasing every year, to the point where in 2004, 60% (148 patients) of all cholecystectomies were performed laparoscopically (Figure 1). Prior to operation, 72 patients underwent preoperative ERCP due to ultrasonographic suspicion of choledocholithiasis, elevated titer of bilirubin and liver function enzymes, recent history of jaundice and/or pancreatitis. Patients with stones in the common bile duct were treated with endoscopic sphincterotomy.
Mortality rate was 0%, but complications did occur, especially early in our series, when surgical experience was still limited. Concerning major complications, bile leak from the cystic duct occurred in 3 (0.24%) patients. In two cases, the leak resulted from failure to clip the cystic duct due to unsatisfactory application of the endoscopic clips. The problem was recognized before the conclusion of the operation in both cases. However, in one of these cases, ligation was impossible, and conversion to the open procedure was necessary. In a third case, the cystic duct injury went undiagnosed intraoperatively, and was only suspected when a significant amount of bile accumulated in the drain on the 1st postoperative day. In this case ERCP confirmed the diagnosis. Endoscopic sphincterotomy was performed and a naso-biliary drainage tube was placed. The leak eventually resolved without any further therapy after 7 d. In 2 (0.16%) patients, a common bile duct injury occurred. In the first occasion, the common bile duct was clipped as it was falsely believed to be the cystic duct. Unfortunately, that mistake went unrecognized intraoperatively and it was only suspected the next postoperative day when the patient developed obstructive jaundice. Eventually, the diagnosis was confirmed with an ERCP and the patient was operated immediately for end-to-end repair of the duct and T-tube placement. In the second case the patient was released from the hospital after a 24 h stay only to return after 2 d with fever, leucocytosis and signs of peritonitis. After an abdominal CT the diagnosis of choloperitoneum was made and the patient was operated on the same afternoon. Intraoperatively, a leak was identified in the common bile duct and it was attributed to the diathermy. After proper cleaning of the peritoneal cavity, the defect was restored with a T-tube placement. In both patients the end result was favorable and no further manipulation was needed.
In 3 (0.24%) cases, bile leak from the gallbladder bed occurred after removing the gallbladder. One case, in whom the leak was identified intra-operatively, was converted to the open procedure. However, in two other cases, the diagnosis was made post-operatively and the patients required ERCP with sphincterotomy.
Thermal injury of the duodenum (2nd segment) occurred in 1 (0.08%) patient. The injury was handled with conversion to open cholecystectomy and suturing of the traumatic lesion.
Bleeding from injury of the cystic artery occurred in 5 (0.4%) patients, 3 of which were admitted and had surgery emergently for acute cholecystitis. The procedure was converted to open cholecystectomy, and bleeding was controlled successfully in all cases. In 10 (0.81%) cases, the bleeding originated from minor accessory vessels of the gallbladder fossa. In 4 of these patients (2 with history of hepatic cirrhosis and 2 with preexisting coagulation abnormalities), conversion to an open procedure was necessary to control bleeding. In 4 (0.32%) cases, bleeding occurred from the port site, and in 1 of them conversion to open procedure was necessary to achieve homeostasis.
Four (0.32%) patients developed a surgical site infection. In 3 of them, gram (+) bacteria were isolated (S. aureus in 2, Enterococcus spp in 1), whereas in 1 case E. coli was the underlying pathogen. All cases were treated successfully with intravenous antibiotics. However, in one case surgical drainage of the wound was necessary. Twenty-seven (2.21%) patients developed moderate post-operative fever. All cases of fever were considered of respiratory origin and treated as such with good outcome.
Two (0.16%) patients developed subcutaneous emphysema, but this was a transient phenomenon and did not cause any morbidity. Hernias at the trocar sites occurred as late complications in 2 (0.16%) patients.
The reported rate of conversion to open cholecys-tectomy ranges between 3 and 7%[10,11]. In our series, 23 (1.88%) of all procedures were converted to the open technique (Table 1). In most cases, uncontrollable bleeding and bile leakage, as well as previous abdominal operation associated with dense adhesions were the main reasons for conversion to the open procedure.
| Reason | n (%) |
| Bleeding | 6 (0.49) |
| Bile leakage | 3 (0.24) |
| Duodenal injury | 1 (0.08) |
| Technical Problem | 1 (0.08) |
| Anatomic Variation (gallbladder aplasia) | 1 (0.08) |
| Inadequate exposure (dense adhesions- inflammation) | 11 (0.9) |
Finally, 2 (0.16%) patients returned to the hospital 1 wk after hospital discharge with signs of choledocholithiasis. This was attributed to stones in the biliary tree that went undiagnosed at the time of the operation. Both patients were treated with ERCP and sphincterotomy, resulting in a good outcome.
Today, laparoscopic cholecystectomy is considered as the treatment of choice for gallstone disease. In our department, laparoscopic cholecystectomy was initially reserved for otherwise healthy patients with uncomplicated disease. However, as experience was gained, laparoscopic cholecystectomy was also offered for patients with more complicated biliary disease, such as acute cholecystitis, former pancreatitis and choledocholithiasis.
Laparoscopic cholecystectomy confers definite advantages compared to the open procedure, but carries its own risks. Consequently, some complications occurred in our series, especially in our early cases when surgeons were less experienced.
In our series, 8 (0.65%) patients suffered injury at various levels of the biliary tree (3 in the cystic duct, 2 in the CBD and 3 in the intrahepatic ducts). The frequency of this complication is 0%-0.8% in laparoscopic cholecystectomy[10,12-14], whereas it is very rare in the open procedure. The relatively high incidence of bile duct injury in laparoscopic cholecystectomy is perceived by many surgeons as the main drawback of the technique. However, as surgeons obtain more experience, the frequency of this complication should decrease.
Bleeding is one of the most frequent and dangerous complications of laparoscopic cholecystectomy. Clinically significant bleeding occurs in 0.5% of laparoscopic cholecystectomy[15]. In our series, bleeding was observed in 19 (1.55%) patients, but in most cases, it was minor and easily controlled. Only 6 (0.49%) patients had bleeding that necessitated conversion to the open procedure. Factors contributing to operative site bleeding may include inadequate exposure, acute inflammation, portal hypertension, adhesions, coagulopathy and rough technique[16]. This was the case in our series, as 5 of the 6 patients who needed conversion to the open procedure were acute admissions. In these patients, inflammatory reaction in the gallbladder fossa prevented adequate exposure of the cystic artery, and transection of the vessel was the end result. In another patient, bleeding occurred from the trocar port in the abdominal wall. Though not significant in amount, its origin could not be revealed and conversion to open was inevitable. Though bleeding is a potentially catastrophic complication, inherent to the laparoscopic technique, it is also the most preventable one, as it is largely related to operator technique.
Wound infection, usually involving the umbilical cannulation site through which the gallbladder is extracted, occurs in 0.3%-1% of cases[4,5,17,18]. Surgical site infection was seen in 4 (0.32%) of our patients, and were all treated successfully with intravenous antibiotics. Postoperative fever occurred in 27 patients. In all cases, the fever was of respiratory origin and resolved with antibiotics and chest physiotherapy.
The average hospital stay was 2.29 d. Recent studies have demonstrated that laparoscopic cholecystectomy can be performed as one day-surgery[19]. In our series, this was true in most uncomplicated, otherwise healthy patients. However, our mean hospital stay was longer, because, when calculating the average length of hospital stay, we included all cases with complications, which required prolonged hospitalization.
In conclusion, in the past few years, much attention has been given to the learning curve of laparoscopic cholecystectomy. Our study adds to and is consistent with the growing body of literature, demonstrating that laparoscopic cholecystectomy is a safe, minimally invasive technique, with favorable results for the patients, provided that the surgeon is meticulous, well-trained and experienced.
| 1. | Muhe E. Die erste colecystektomie durch das lparoskop. Langenbecks Arch Klin Chir. 1986;369:804. [RCA] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 109] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 2. | Asbun HJ, Rossi RL, Lowell JA, Munson JL. Bile duct injury during laparoscopic cholecystectomy: mechanism of injury, prevention, and management. World J Surg. 1993;17:547-551; 551-552. [PubMed] |
| 3. | Périssat J, Collet D, Belliard R, Desplantez J, Magne E. Laparoscopic cholecystectomy: the state of the art. A report on 700 consecutive cases. World J Surg. 1992;16:1074-1082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 69] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Soper NJ, Stockmann PT, Dunnegan DL, Ashley SW. Laparoscopic cholecystectomy. The new 'gold standard'. Arch Surg. 1992;127:917-921; discussion 921-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 308] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 5. | Williams LF Jr, Chapman WC, Bonau RA, McGee EC Jr, Boyd RW, Jacobs JK. Comparison of laparoscopic cholecystectomy with open cholecystectomy in a single center. Am J Surg. 1993;165:459-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 64] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Berggren U, Gordh T, Grama D, Haglund U, Rastad J, Arvidsson D. Laparoscopic versus open cholecystectomy: hospitalization, sick leave, analgesia and trauma responses. Br J Surg. 1994;81:1362-1365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 182] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 7. | Trondsen E, Reiertsen O, Andersen OK, Kjaersgaard P. Laparoscopic and open cholecystectomy. A prospective, randomized study. Eur J Surg. 1993;159:217-221. [PubMed] |
| 8. | Majeed AW, Troy G, Nicholl JP, Smythe A, Reed MW, Stoddard CJ, Peacock J, Johnson AG. Randomised, prospective, single-blind comparison of laparoscopic versus small-incision cholecystectomy. Lancet. 1996;347:989-994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 239] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 9. | Gallstones and laparoscopic cholecystectomy. NIH consens statement online. 1992;10:1-20. |
| 10. | Soper NJ, Dunnegan DL. Laparoscopic cholecystectomy: experience of a single surgeon. World J Surg. 1993;17:16-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Wolfe BM, Gardiner BN, Leary BF, Frey CF. Endoscopic cholecystectomy. An analysis of complications. Arch Surg. 1991;126:1192-1196; discussion 1196-1198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 111] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Deveney KE. The early experience with laparoscopic cholecystectomy in Oregon. Arch Surg. 1993;128:627-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Orlando R 3rd, Russell JC, Lynch J, Mattie A. Laparoscopic cholecystectomy. A statewide experience. The Connecticut Laparoscopic Cholecystectomy Registry. Arch Surg. 1993;128:494-498; discussion 498-499;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 142] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 14. | A prospective analysis of 1518 laparoscopic cholecystectomies. The Southern Surgeons Club. N Engl J Med. 1991;324:1073-1078. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1006] [Cited by in RCA: 921] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 15. | Deziel DJ. Complications of cholecystectomy. Incidence, clinical manifestations, and diagnosis. Surg Clin North Am. 1994;74:809-823. [PubMed] |
| 16. | Cuschieri A. The difficult cholecystectomy. In Cuschieri A, Berci G (eds): Laparoscopic biliary surgery, 2nd ed. Oxford: Blackwell Sci Pub 1992; 10. |
| 17. | Stoker ME, Vose J, O'Mara P, Maini BS. Laparoscopic cholecystectomy. A clinical and financial analysis of 280 operations. Arch Surg. 1992;127:589-594; discussion 594-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 67] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 18. | Wittgen CM, Andrus JP, Andrus CH, Kaminski DL. Cholecystectomy. Which procedure is best for the high-risk patient. Surg Endosc. 1993;7:395-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Leeder PC, Matthews T, Krzeminska K, Dehn TC. Routine day-case laparoscopic cholecystectomy. Br J Surg. 2004;91:312-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 73] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
S- Editor Pan BR L- Editor Kumar M E- Editor Liu WF