INTRODUCTION: EPIDEMIOLOGY AND PATHOPHYSIOLOGY
Diverticulosis of the colon is an acquired condition that results from herniation of the mucosa through defects in the muscle layer. Epidemiological and anatomic studies have revealed that diverticular formation of the colon is primarily a disease that occurs in industrialized and westernized countries[1,2]. Approximately 60 percent of humans over age 60 living in westernized countries will develop colonic diverticula[3]. Postmortem studies reveal that it is rare prior to age 40, but increases with age so that one can estimate that by age 80 approximately 65 percent of patients have diverticula of the colon[4,5]. Of major importance is that approximately 25%-30% of these patients will develop a complication: diverticulitis, bleeding, or perforation[5,6]. It is now widely accepted that chronic diverticular formation occurs in westernized societies due to a lack of fiber in the diet[6,7]. The assumption is that decreased dietary fiber intake results in decreased intestinal contents and, hence, decreased size of the lumen, which results in the transmission of muscular contraction pressure to the wall of the colon rather than to the contents of the lumen. The result of increased force (pressure) on the wall is the formation of diverticula at the weakest point in the wall: the sites of penetration by blood vessels.
The cause of acute diverticulitis remains obscure. It has been speculated that obstruction at the mouth of the diverticulum results in diverticulitis, similar to appendicitis, but this is no longer the accepted theory, and some feel that chronic inflammation precedes clinical diverticulitis[6]. Descriptions of diverticular disease may be divided into two stages: (1) diverticular formation; and (2) diverticulitis with either pericolitis (microabcess), pericolic phlegmon, pericolic abscess, pelvic or intraabdominal abscess, and free perforation leading to bowel obstruction, fistulization, or bacteremia and septicemia[8]. In trying to assess the first stage of the disease, our preliminary evaluations identified that there is a microscopic colitis associated with mucosa of the colon adjacent to the diverticula[9]. Others have also identified asymptomatic diverticular inflammation at screening colonoscopy[10].
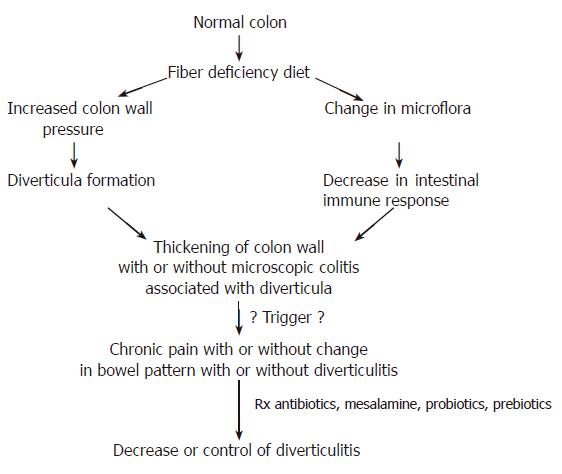
As illustrated in Figure 1, we hypothesized that diverticular disease is formed in the setting of low fiber diet. Our studies have revealed that Connecticut diets are low in fiber[11]. Furthermore, our laboratories and others have established that the indigenous bacterial flora in subjects eating a low fiber diet is decreased and altered as compared to subjects eating high fiber[12,13]. Because of this alteration, we postulate a very mild colitis may occur and may progress to a more focal, acute diverticulitis. The sigmoid colon has the smallest diameter of the colon and a different motility pattern. It is the most common site of diverticular formation in western countries. Post mortem studies[4] of 90 colons revealed that 26% had numerous diverticula limited to the sigmoid, but 15% also had an occasional diverticulum of the sigmoid, 30% had sigmoid and descending colon diverticula with 16% scattered throughout and 4% in the sigmoid, descending and transverse. The cecum and ascending colon make up less than 5%. However, right-sided diverticula are definitely more common in humans in Asia and Hawaii[6]. Spastic motility disturbances are associated with the most common forms of the disease in western society. The sigmoid may develop a corrugated appearance. Initial pathology studies suspected an increase in smooth muscle cells, but pathologic studies clearly reveal there is, in fact, an increased deposition of elastin between the myocytes[14].
Figure 1 Pathophysiologic development of diverticulitis and proposed therapy.
INFLAMMATORY BOWEL DISEASE AND DIVERTICULAR DISEASE
The simultaneous occurrence of both inflammatory bowel disease and diverticulosis was first discussed by Schmidt and colleagues in 1968[15]. The overlap of Inflammatory bowel disease (IBD) and diverticular disease is being recorded more commonly[16]. Much debate still exists as to whether there is increased prevalence when the two phenomena occur together. However, there clearly is an overlap syndrome in which clinicians must differentiate acute diverticulitis from chronic Crohn’s disease[16,17]. Makapugay and colleagues described a picture of chronic colitis associated with diverticular disease. Their work indicated that this may be more prevalent than suspected[18]. Peppercorn described eight patients who were more than 60 years of age and presented with segmental chronic colitis associated with diverticula[19]. Imperiali and associates performed a large perspective study to identify IBD-like lesions[20]. They reviewed 5457 consecutive colonoscopies and found that 733, or 13.5%, had diverticula, but only 20 of these patients (0.36%) met all of the endoscopic criteria for segmental colitis as well. They indicated that the phenomenon was less common than previously suspected.The picture is still not clear, however, since none of the studies did mucosal biopsies to indicate whether there was a low level of inflammation in mucosa adjacent to diverticula that is endoscopically normal, as indicated in some pilot studies[9,20]. Clearly, more studies are needed to fully evaluate the significance of the association of these two phenomena.
THE CLINICAL PICTURE AND DIFFERENTIAL DIAGNOSIS
When colonic diverticula are discovered during an examination such as barium enema, CT scan or colonoscopy which were done for screening or other reasons, they are assumed to be asymptomatic. Since the incidence is so high, most of these patients are not treated. However, as many as 5%-20% of patients with diverticula of the colon are symptomatic and can develop complications[21]. The clinical presentation depends on the degree and extent of the inflammation and the degree of loss of normal bowel function due to sigmoid diverticular formation. The most common presentation is that of left-lower quadrant pain associated with either mild constipation or diarrhea. When the inflammation is severe or there is a micro-abscess or abscess formation, the pain will be more severe and can present as an acute abdomen. Determining the total white blood count is helpful. It is usually elevated when the inflammation is severe. Depending on the severity, there may or may not be elevated temperature. If there is true perforation, the abdomen is much more tender with possible rebound, and a picture of peritonitis with a markedly elevated white blood count and perhaps a toxic-appearing patient.Because of the variable position of the colon and differing anatomy in different individuals, the pain might be located more on the right side or in the pelvis or even in the upper quadrants. When this occurs, a differential diagnosis between gynecologic disease or other diseases attributed to the abdomen must be considered. Radiologic findings are extremely helpful. Because of the possibility of perforation, a barium enema is no longer the preferred procedure. Computerized tomography (CT) scanning is now accepted as the most helpful diagnostic procedure. Areas of inflammation and the associated mesentery soft tissue are identifiable as well as abscesses. It must be kept in mind that it takes time for an abscess to form, and it might be missed on the initial CT examination. A study of 420 patients with left-sided diverticulitis proven at surgery compared CT to contrast enema. The CT was superior, was more sensitive, and was significantly better in grading the severity of inflammation[22]. CT has also proven most helpful in the management of complicated diverticulitis. It is shown in correlated studies that once an abscess is present, there is a high risk of failure from non-operative management. However, when management is in question, CT is of great help in defining the course of treatment. Furthermore, CT can be very helpful in guiding percutaneous drainage of abscess in order to prevent or delay surgery in selective cases[23].
Colonoscopy is used judiciously when there are any suspicions of very acute inflammation. Once that has subsided, it can be helpful in excluding a suspected malignancy or overlap inflammatory bowel disease picture.
COMPLICATIONS
Perforations and diverticular hemorrhage are the major complications of diverticulosis. Perforation has to be treated acutely. However, when there is perforation into adjacent organs such as the bladder or vagina, appropriate gynecologic and urologic evaluations are necessary. Those patients are treated medically and then surgically if necessary. Diverticular hemorrhage is the most common cause of colonic bleeding in western societies. It is estimated that 3%-5% of patients with diverticula will have severe blood loss at some point. Diagnosis of the site of ongoing diverticular bleeding is important and may be difficult. Radio-isotope studies, colonoscopy, and arteriography, diagnostic and/or therapeutic may be helpful, but barium contrast enemas are of no help[21-24].
MEDICAL THERAPY
Simple, uncomplicated diverticular disease often requires no therapy. Many clinicians advise a high fiber diet, but the evidence that this is helpful in preventing diverticulitis is not yet clear. Once mild symptoms develop, clinicians may prescribe high fiber diets, plus anticholinergic drugs to theoretically relax the bowel. Dicyclomine is used most often. Once there is any sign of infection, such as elevated white blood count or low-grade temperature, antibiotics are indicated. Depending on the institution and the location, broad spectrum antibiotics are used since the colonic flora is a combination of aerobes and anaerobes. If symptoms are severe, combinations of ciprofloxin and gentamicin or metronidazole are recommended, or amoxicillin/clavulanic acid, or sulfamethoxazole/trimethoprim. Treatment is usually anywhere from 1-2 wk with careful monitoring and reevaluation. Diet is always of concern in these patients. When there are acute symptoms, the bowel is rested and low fiber diets are recommended. However, once recovery occurs then high fiber diets are recommended.
Medical treatment is changing. Based on the theory that there is chronic inflammation in the bowel wall, even between bouts of acute diverticulitis, enough interest was created to evaluate the use of anti-inflammatory agents. There are now four groups in Italy that have reported favorable results with the use of mesalamine alone or in combination with antibiotics. Evaluation of these studies[26-31] clearly reveals that mesalamine decreases the length of the course of the diverticulitis, improves management with the use of concomitant antibiotics, has a prolonged effect and also appears to decrease the incidence of recurrent attacks. From these studies, it appears that mesalamine is safe and holds promise as a new therapy in the treatment of acute and chronic diverticulitis.
The theory that inflammation is chronic in the formation of diverticulitis also raises the hypothesis that probiotics would stimulate the immune process and possibly be effective. Only one paper has appeared on this subject[32]. The authors compared the use of an anti-microbial agent plus an absorbent to the same regimen supplemented with non-pathogenic Escherichia Coli, Nissle strain. They found that the average remission for the antibiotic regime was 2.43 mo as compared to 14.1 mo for the antibiotic plus probiotic regimen. This is only one study, but the concept is valid and these findings indicate other studies are in order.
SURGICAL TREATMENT
Once medical treatment fails or when the presentation is one of acute abdominal perforation, surgery becomes essential. Standard surgical treatment today may include a longer period of observation, or percutaneous drainage of abscess, but may finally require surgical resection. Three-stage operations are no longer the treatment of choice. The two stage procedure where there is first a colostomy and then later closure of the colostomy after a 4-12 wk period of observation are preferred[21,24,33].
Most guidelines treating elective or non-urgent cases recommend that the resection must remove all thickened diseased colon, but not necessarily all of the proximal diverticulum-bearing colon. It may be acceptable to retain proximal diverticular colon as long as the remaining bowel is not hypertrophied[24]. In almost all cases, all of the sigmoid colon should be removed. In urgent and emergent cases, the resection and diversion are required. In rare cases, it may be attempted in a one-stage procedure.
With the advent of laparoscopic procedures, sigmoid resection may benefit from the approach[34]. Laparoscopic surgery for diverticular disease can be done safely with low conversion and complication rates when performed properly in select patients[34]. When diverticular hemorrhage does not stop, surgery may be indicated. At times it may be emergent. Segmental resection is certainly preferred, but hemicolectomy is often necessary. The operative mortality rates are high, between 9%-11%, and largely depend on co-morbid conditions and the age of the patient. When it is difficult to identify the exact site, morbidity and mortality rates may increase to as high as 35%. Fortunately, most cases of bleeding stop spontaneously, but when surgery is required, the site of bleeding must be identified. On the rare occasion when it cannot, then total colectomy becomes necessary.
Finally, diverticulitis is unusual in young people, especially those under 40. However, when it does occur in this age group, it appears to be virulent and as many as 2/3 of these patients require surgical intervention[21].
S- Editor Pan BR E- Editor Liu WF