INTRODUCTION
Symptomatic gallstone disease is a very common indication for abdominal surgery. It is estimated that around 500 000 cholecystectomies are performed a year in the United States. Gallstones, alone, are rarely an indication for surgery, but 10% of the adult population are believed to carry them. Furthermore, up to one-third of the population over 70 years of age will have gallstones. Gallstone formation is a multifactorial process but is undoubtedly associated with family history, diabetes mellitus, pregnancy, obesity, significant weight loss, and hemolytic diseases. As many as 35% of patients with gallstones will ultimately become symptomatic and require cholecystectomy[1].
Common indications for surgical treatment for cholelithiasis include biliary colic, acute cholecystitis, gallstone pancreatitis, and other presentations of choledocholithiasis including bile duct obstruction and cholangitis. Other relative indications include gallstones in patients undergoing splenectomy for hemolytic anemia, high risk patients in the pretreatment phase for other conditions such as bone marrow transplant. Cholecystectomy is no longer routinely performed for asymptomatic gallstones in those undergoing bariatric surgery or aortic surgery.
Common bile duct (CBD) stones may be discovered preoperatively, intraoperatively or postoperatively. The standard preoperative workup for patients presenting with symptoms attributable to cholelithiasis includes liver function tests, and abdominal ultrasound. These tests, combined with clinical exam and history, constitute the entire workup for most patients. Abnormalities in these tests may suggest the presence of choledocholithiasis. Choledocholithiasis may occur in up to 3%-10% of all cholecystectomy patients[1], or as high as 14.7% in some series[2]. This includes some patients without classic preoperative findings suggestive of choledocholithiasis. Of these asymptomatic patients, it is believed about 15% will eventually become symptomatic[3] and require further interventional treatment.
Since the advent of routine laparoscopic cholecystectomy, the debate has continued about the utility of intraoperative bile duct assessment, primarily with cholangiography or intraoperative ultrasonography. This debate continues to some degree, with most surgeons either selectively or routinely evaluating the bile duct intraoperatively. A smaller subset relies only on preoperative assessment tools, including magnetic resonance cholangiopancreatography (MRCP) and endoscopic retrograde cholangiopancreatography (ERCP), as a complement to routine laboratory and imaging studies. The most common intervention for common bile duct (CBD) stones is ERCP. Other procedures for CBD stone extraction include percutaneous, transhepatic stone removal and intraoperative CBD exploration, whether laparoscopic or open. The availability of equipment and skilled practitioners who are facile with these techniques varies among institutions. The timing of the intervention is often dictated by the clinical situation.
PREOPERATIVE EVALUATION AND THERAPY
Diagnosis of choledocholithiasis is not always straightforward and clinical evaluation and biochemical tests are often not sufficiently accurate to establish a firm diagnosis. Imaging tests, particularly abdominal ultrasound, are used routinely to confirm the diagnosis. Liver function tests (LFT) can be used to predict CBD stones[4,5]. Elevated serum bilirubin and alkaline phosphatase typically reflect biliary obstruction but these are neither highly sensitive nor specific for CBD stones. Excepting obvious jaundice, a raised GGT level has been suggested to be the most sensitive and specific indicator of CBD stones. A value of greater than 90 U/L has been proposed to indicate a high risk of choledocholithiasis[4]. However, laboratory data may be normal in as many as a third of patients with choledocholithiasis, warranting further evaluation of the CBD by imaging studies to clarify the diagnosis.
In order to help select from the various diagnostic and therapeutic options, patients may be classified preoperatively into high, moderate or low risk groups. The high risk (> 50% risk) group includes those patients with obvious clinical jaundice or cholangitis, choledocholithiasis or a dilated CBD on ultrasonography. Patients with a history of pancreatitis or jaundice, elevated preoperative bilirubin and alkaline phosphatase levels or multiple small gallstones carry a moderate (10%-50%) risk of choledocholithiasis. Patients with large gallstones, without a history of jaundice or pancreatitis and with normal liver function tests are considered unlikely to have CBD stones and therefore at low risk (< 5%)[6-8].
The transabdominal ultrasound examination (US) is the most commonly used screening modality. In patients who present with symptoms attributable to gallstone disease, US may be the only radiologic study ordered. It has the advantages of being widely available, non-invasive, and inexpensive. Ultrasonography, however, is highly operator dependent, but it can provide useful information in experienced hands. For a diagnosis of cholecystitis, in most circumstances, gallbladder stones need to be visualized. The sonographic presence of wall thickening, pericholecystic fluid, and a Murphy’s sign, may be helpful but are not required for a diagnosis of acute cholecystitis. The ultrasonographer should routinely report indirect information suggestive of the presence or absence of CBD stones, specifically the CBD diameter or any signs of intrahepatic bile duct dilation. The sensitivity of US for detecting biliary dilatation, as reported in various studies, varies from 55 to 91 percent[9]. A CBD diameter of greater than 6 mm on US is associated with a higher prevalence of choledocholithiasis[10] .
Computed tomography (CT) may have some role in diagnosis of gallstone disease and choledocholithiasis. Many patients presenting with acute abdominal pain will undergo a diagnostic CT scan as part of the acute workup. A diagnosis of acute cholecystitis may be evident based on signs of gallbladder inflammation. Cholelithiasis may be detected on CT[11] and often the diameter of the CBD can be measured. In the clinical setting, US may not be necessary for preoperative evaluation if the CT scan provides this information. The role of helical CT cholangiography is still in evolution, particularly in the United States. Intravenously administered contrast agents, combined with high resolution helical scans and three dimensional reconstructions that can be very useful in diagnosing choledocholithiasis[12,13]. The sensitivity of this technique can be as high as 95.5%[12]. This technique is not widely utilized in the U.S. as the available contrast agents often cause significant nausea on administration. The availability of MRCP also limits the need for this modality.
MRCP has emerged as an accurate, non-invasive diagnostic modality for investigating the biliary and pancreatic ducts[14] and has been recommended in some circles as the preoperative procedure of choice for the detection of CBD stones[4,15,16]. MRCP provides excellent anatomic detail of the biliary tract and has a sensitivity of 81%-100% and a specificity of 92%-100% in detecting choledocholithiasis[14]. The accuracy of MRCP in diagnosing CBD stones is comparable with that of ERCP and IOC[14,17]. It thus avoids the need for a potentially high risk, invasive procedure in more than 50% of patients, allowing selective use of ERCP or surgical CBD exploration in those patients who require a therapeutic intervention. These results have led some practitioners to consider MRCP the new gold standard for biliary imaging[14,18]. MRCP may, however, miss stones less than 5 mm in diameter. MRCP is an expensive option that requires significant expertise for interpretation; this modality may not always be readily available.
Endoscopic techniques such as endoscopic ultrasound (EUS) and ERCP can also be useful tools in preoperative diagnosis and, in the case of ERCP, management of choledocholithiasis. Both procedures are more invasive than strictly radiologic techniques, and carry the low, but inherent risks of upper gastrointestinal tract endoscopy. ERCP also carries the risks associated with biliary instrumentation, such as pancreatitis. Endoscopic ultrasound (EUS) can been used to evaluate the CBD and identify calculi. Studies comparing the accuracy of EUS to US, CT and ERCP for detecting choledocholithiasis show a sensitivity of EUS ranging from 88%-97%, with a specificity of 96%-100%[19]. This is comparable to ERCP and avoids the risks of pancreatitis, cholangitis and radiation exposure[19]. The role of EUS, however, is not well established especially when cost and availability of less invasive modalities such as MRCP are considered. EUS may be combined with ERCP at the same endoscopy session if biliary calculi are identified, allowing it to be a bridge to therapeutic intervention.
ERCP has been the gold standard for preoperative diagnosis of CBD calculi. When compared to other tests such as ultrasonography and MRCP, ERCP has the advantage of providing a therapeutic option when a CBD stone is identified. Stone retrieval and sphincterotomy has supplanted surgical treatment of choledocholithiasis in many institutions[14,20]. Successful cholangiography by an experienced endoscopist is achieved in greater than 90% of patients. Complications associated with ERCP can be as high as 15% and include pancreatitis, cholangitis, perforation of the duodenum or bile duct, and bleeding. These individual complications can occur in 5%-8% of patients. The mortality rate from ERCP is 0.2%-0.5%[21,22]
INTRAOPERATIVE EVALUATION AND THERAPY
Since laparoscopic cholecystectomy became a routine procedure in the early 1990’s, debate has continued about the role of intraoperative bile duct assessment. The interest in intraoperative cholangiography (IOC) came from both the desire to detect CBD stones and to potentially identify any bile duct abnormalities, including iatrogenic injuries at the time of surgery. Routine cholangiography is not generally considered to be the standard of care but still has its proponents[3]. Most surgeons selectively evaluate the bile duct intraoperatively. A smaller subset relies only on preoperative assessment tools including magnetic resonance cholangiopancreatography (MRCP) and endoscopic retrograde cholangiopancreatography (ERCP) as a complement to routine laboratory and imaging studies.
Intraoperative cholangiography can be a useful tool to identify choledochal calculi but its application remains controversial. Proponents often believe that IOC enables clear definition of the biliary tree anatomy[3,23,24], thus reducing the risk of bile duct injury during cholecystectomy. Most studies on the subject show no significant difference in the rates of ductal injury between routine and selective IOC. Routine IOC has been found to yield little benefit over the selective approach in the detection of symptomatic CBD stones[3] Cholangiography is a relatively straight forward procedure to perform. It does add to the operative time, approximately an additional 15 min[25,26], but surgeon and operative team experience can minimize this. Dynamic fluoroscopic imaging is the technique of choice and can provide a specificity and sensitivity of 94% and 98%, respectively, in experienced hands[27]. This technique may be somewhat less sensitive for patients presenting with biliary pancreatitis[27]. A complete IOC should demonstrate the cannulation of the cystic duct, filling of the left and right hepatic ducts, CBD and common hepatic duct diameter, the presence or absence of filling defects in the biliary tree, and free flow of contrast into the duodenum (Figure 1).
Figure 1 Intraoperative cholangiogram via the cystic duct demonstrating proximal biliary dilation and two filling defects in the CBD (Arrows).
Obstruction or other biliary abnormality should be suspected if these findings are not clear.
The overall safety profile of IOC is very good. The incidence of pancreatitis, in contrast to ERCP, is negligible[28]. The reliability, ease to perform, and low complication rate of IOC suggest that, at least in cases where choledocholithiasis is not proven, IOC during a cholecystectomy is a better choice than preoperative ERCP assessment of the bile ducts. More recently intraoperative ultrasonography of the CBD during laparoscopic cholecystectomy has been shown to satisfactorily demonstrate stones and the biliary tree. Use of intraoperative ultrasound requires a significant learning curve, but in experienced hands takes less operative time than traditional IOC[25,26]. Laparoscopic ultrasound compares well with intraoperative cholangiography. With a sensitivity of 96% and a specificity of 100%, and the advantages of saved time and lack of radiation, intraoperative ultrasound may be a superior diagnostic modality when compared to IOC[23]. The use of intraoperative laparoscopic ultrasound is limited by the availability of equipment and surgeon training and experience. Efforts to incorporate ultrasonography training in to surgical residency curricula should aid its acceptance and use.
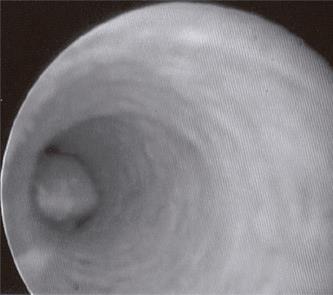
When CBD stones are detected intraoperatively, a surgeon must make a clinical decision on how to proceed. This decision is often dictated by the availability of equipment, surgeon preference and skill, and the availability of ERCP at a facility. Available options include laparoscopic CBD exploration, intraoperative ERCP, open CBD exploration, or postoperative therapy. Many surgeons are reluctant to proceed with an open procedure when other, less invasive, options are generally available. However, a decision to delay therapy to the postoperative period risks encountering procedural difficulties that preclude endoscopic therapy. Options for intraoperative CBD clearance include variations of laparoscopic exploration. Laparoscopic CBD exploration is most commonly performed with acholedochoscope. The scope, attached to a second video camera and light source, is inserted into the CBD via either the cystic duct (Figure 2) or via a choledochotomy. Placement of the choledochoscope directly into the CBD via a choledochotomy is generally reserved for patients with ducts dilated to greater than 6 mm in diameter on cholangiogram[20]. A continuous saline infusion through the choledochoscope dilates the duct and clears debris. CBD stones can be directly visualized (Figure 3) and instrumented. Between 66 and 82.5% of laparoscopic CBD explorations can be performed via the cystic duct[20,29]. In experienced hands, the CBD clearance rate is as high as 97%[2,29]. In one large series of laparoscopic CBD exploration, the overall morbidity rate of this procedure is approximately 9.5%, with a 2.7% retained stone rate[2]. These data are equivalent to the experience with ERCP.
Figure 2 Laparoscopic view of a choledochoscope (CS) entering the CBD via the cystic duct.
The gallbladder (GB) is retracted to the left of the image.
Figure 3 CBD stone as seen through the choledochoscope.
An alternate technique of laparoscopic CBD clearance involves stone extraction under fluoroscopic guidance. This technique, as described by Traverso et al, does not use a choledochoscope, but can be highly effective in CBD clearance for single stones (87%), with an overall 59% success rate[30]. In this technique, instruments, including stone extraction baskets, are passed into the CBD (usually via the cystic duct) under fluoroscopy. The fluoroscopic images facilitate stone capture and removal. This technique simplifies the operating room set up for CBD exploration because additional video equipment is not required. In this series, patients whose ducts were not cleared laparoscopically, underwent ERCP. The authors noted a significantly lower complication rate in patient who did not undergo ERCP[30]. Likewise, the overall associated costs were lower in these patients[31].
Laparoscopic techniques can be very effective at clearing CBD stones, but significant expertise and experience is required to achieve high success rates. Stones impacted at the sphincter of Oddi are often the most difficult to extract by this technique. Long term follow up does not demonstrate a significant risk of CBD stricture or other complications for these procedures[2,29,30]. This technique is also advocated in the pediatric population by some practitioners as a way of avoiding an ERCP[32]. Intraoperative ERCP, although often limited by the immediate availability of a qualified endoscopist, is a technique that can be very useful. This takes advantage of the preexisting anesthetic and does not prolong hospital stay by delaying the procedure[33,34]. In some instances, cooperation between the surgeon and the endoscopist can expedite the procedure[35]. Guidewire placement, throught the sphincter of Oddi, into the duodenum via the IOC catheter can facilitate cannulation, especially for patients with difficult duodenal anatomy[34]. In the case of an unsuccessful extraction, open CBD exploration or drainage of the duct should be considered.
POSTOPERATIVE EVALUATION AND THERAPY
Postoperative ERCP is commonly used modality for CBD clearance when a stone is detected intraoperatively. This technique is highly effective[20], but can be complicated when anatomic variables such as duodenal diverticulae or unusual biliary anatomy, are encountered[36]. On the occasion that ERCP fails, a primary option includes returning to the operating room for a laparoscopic or open exploration. However, other less invasive options may be available.
In selected patients, percutaneous transhepatic (PTH) therapies should be considered for CBD clearance. Access to the biliary system can be obtained percutaneously, under ultrasound guidance. Via this access point, stones can be extracted, a sphincterotomy can be performed, or lithotripsy can be used over a single, or multiple sessions to ensure duct clearance[37,38]. A percutaneous drain can be used to decompress the system between procedures or for temporary stenting after the duct is clear.
Novel approaches have been performed in other anatomic settings which preclude ERCP, such as prior gastric surgery. The most common gastric surgery currently performed is the Roux-Y gastric bypass. In this surgery, a small gastric pouch is created and anastomosed to a limb of jejunum. The majority of the stomach, duodenum, and proximal jejunum are bypassed, making endoscopic access technically difficult. Combined laparoscopic surgical and endoscopic procedures have been described. Endoscopic access can be achieved via a gastrostomy[39] or jejunostomy[40]. The endoscope can be passed under surgical guidance, and an ERCP can be performed in the standard fashion. These procedures are only described in short case reports, but will undoubtedly become more common place with the prevalence of gastric bypass.
In conclusion, given the various diagnostic and therapeutic options available for managing choledocholithiasis, clinical judgment is paramount. The surgeon and the patient are best served by accurate laboratory and radiologic assessment prior to cholecystectomy. In the setting of high preoperative suspicion for choledocholithiasis, preoperative imaging with MRCP may help guide subsequent treatment. If CBD stones are present on MRCP or in the setting of clinical jaundice or cholangitis, preoperative ERCP is the first line option. However, preexisting anatomic abnormalities may influence this decision. Laparoscopic IOC with a CBD exploration is a reliable approach in experienced hands and if an ERCP is unsuccessful.
Cholangiography during cholecystectomy is recommended for patients with a history of gallstone pancreatitis, LFT abnormalities, or an enlarged CBD on preoperative imaging who have not undergone MRCP or ERCP. IOC is also recommended when intraoperative findings suggest anatomic abnormalities or unsuspected CBD calculi.
Intraoperative laparoscopic CBD exploration is the first option for choledocholithiasis detected in the operating room. Intraoperative or postoperative ERCP are options for incompletely cleared ducts. Percutaneous treatment or combined laparoendoscopic options are available in some centers for patients who cannot undergo ERCP or laparoscopic choledochotomy. Open CBD exploration is a safe option, but usually limited to the setting of concomitant open surgery or as a last resort when other therapeutic modalities fail.
S- Editor Pan BR E- Editor Bi L