Published online May 14, 2006. doi: 10.3748/wjg.v12.i18.2919
Revised: November 30, 2005
Accepted: January 9, 2006
Published online: May 14, 2006
AIM: To evaluate magnetic resonance cholangiopancre-atography (MRCP) findings in conjunction with magnetic resonance (MR) images in autoimmune pancreatitis (AIP) patients.
METHODS: Nine patients with AIP underwent MRI, MRCP, endoscopic retrograde cholangiopancreatography (ERCP), computed tomography, and ultrasonography. The MRCP and MR images taken before and after steroid therapy were reviewed and compared with other imaging modalities. The MRCP findings of the AIP cases were compared to those of 10 cases with carcinoma of the head of the pancreas.
RESULTS: On MRCP, the narrowed portion of the main pancreatic duct noted on ERCP was not visualized, while the non-involved segments of the main pancreatic duct were visualized. The degree of upstream dilatation of the proximal main pancreatic duct was milder than that seen in cases of pancreatic carcinoma. Stenosis or obstruction of the lower bile duct was detected in 8 patients. MR images showed enlargement of the pancreas with decreased signal intensity on T1-weighted MR images, increased signal intensity on T2-weighted MR images, and, in 3 patients, a hypointense capsule-like rim. After steroid therapy, the previously not visualized portion of the main pancreatic duct was seen, along with improvement of the bile duct stenosis. Pancreatic enlargement decreased, and the abnormal signal intensity on both T1- and T2-weighted MR images became isointense.
CONCLUSION: MRCP cannot differentiate irregular narrowing of the main pancreatic duct seen with AIP from stenosis of the main pancreatic duct seen with pancreatic carcinoma. However, MRCP findings in conjunction with MR imaging of pancreatic enlargement that shows abnormal signal intensity on T1- and T2-weighted MR images are useful in supporting a diagnosis of AIP.
- Citation: Kamisawa T, Chen PY, Tu Y, Nakajima H, Egawa N, Tsuruta K, Okamoto A, Kamata N. MRCP and MRI findings in 9 patients with autoimmune pancreatitis. World J Gastroenterol 2006; 12(18): 2919-2922
- URL: https://www.wjgnet.com/1007-9327/full/v12/i18/2919.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i18.2919
Autoimmune pancreatitis (AIP) has recently been described as a peculiar type of chronic pancreatitis with underlying autoimmunity[1-5]. Patients with AIP almost always have enlargement of the pancreas[1-5], and their major presenting symptom (65%[6]-68%[7]) is obstructive jaundice due to obstruction of the bile duct. Since, pancreatic or bile duct carcinoma is suspected, pancreaticobiliary duct system is examined by endoscopic retrograde cholangiopancreatography (ERCP). The hallmark finding of AIP on direct pancreatogram is irregular narrowing of the main pancreatic duct; stenosis of the intra- or extrahepatic bile duct is frequently detected on cholangiography[1,2,5-7].
Magnetic resonance cholangiopancreatography (MRCP) has become popular as a non-invasive method for obtaining high quality images of the pancreaticobiliary tree[8]. Although the features of AIP on computed tomography (CT) and ERCP have been reported, the MRCP features of AIP have not been clarified. The aim of this study was to describe the MRCP findings in AIP patients before and after steroid therapy and to review the utility of MRCP for the diagnosis for AIP.
Nine patients (6 males and 3 females, average age 60.3 years) with AIP who had MRCP in the time period from 1997 to 2005 were enrolled in this study. All patients had ERCP, ultrasonography (US), and CT. ERCP showed irregular narrowing of the main pancreatic duct in all patients [diffuse (n = 1), segmental-head (n = 3), segmentally skipped-head and body (n = 3), segmental-tail (n = 2)]. CT and US showed enlargement of the pancreas in 8 patients [diffuse (n = 3), segmental-head (n = 3), segmental-tail (n = 2)]. Six patients had elevations of serum IgG, 7 patients had elevations of serum IgG4, and 3 patients had antinuclear autoantibody. Six patients presented with obstructive jaundice. On cholangiography, stenosis of the bile duct was detected in 8 patients [lower common bile duct (n = 5) and intrahepatic and lower common bile duct (n = 3)]. All patients were given steroid treatment and responded both morphologically and serologically. From the radiological and serological findings, in addition to effectiveness of steroid treatment, all 9 patients were diagnosed as having AIP.
MRCP was done using a 1.5 T magnetic resonance imaging (MRI) machine (INTERA, PHILIPS Co Ltd, Netherlands) by coronal heavily T2-weighted single-shot rapid acquisition with relaxation enhancement. The MRCP and MR images taken before and after steroid therapy were reviewed and compared with other imaging modalities. The MRCP findings of the AIP cases were compared to those of 10 cases with carcinoma of the head of the pancreas.
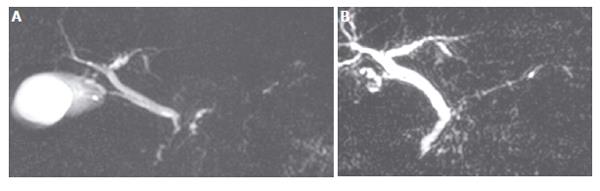
The narrowed portion of the main pancreatic duct seen on ERCP was not visualized on MRCP, while the non-involved segments of the main pancreatic duct were seen on MRCP. On MRCP, the entire main pancreatic duct was not seen in 1 patient in whom the main pancreatic duct showed diffuse narrowing on ERCP. In 3 patients in whom the main pancreatic duct was segmentally narrowed in the head region on ERCP, the MRCP visualized the main pancreatic duct only in the body and tail of the pancreas, but not in the head region. In 2 patients, MRCP showed the main pancreatic duct only in the head and body of the pancreas, but not in the tail region. On MRCP, 2 segmentally skipped lesions of the main pancreatic duct in the head and body of the pancreas were not visualized in 3 patients (Figure 1A and Table 1). Although upstream dilatation of the proximal main pancreatic duct was detected in 6 patients, the degree of dilatation was milder than that in cases of pancreatic carcinoma. Stenosis or obstruction of the lower bile duct was detected in 8 patients, of whom 3 patients also showed stenosis of the intrahepatic bile duct accompanied by dilatation of the proximal bile duct, similar to the findings on ERCP.
| ERCP | MRCP |
| Diffuse narrowing of MPD in entire pancreas (n = 1) | Non-visualized MPD in entire pancreas (n = 1) |
| Segmental narrowing of MPD in the head of pancreas (n = 3) | Non-visualized MPD in the head of pancreas (n = 3) |
| Two skipped narrowing of MPD in the head and body of pancreas (n = 3) | Two skipped non-visualized MPD lesions in the head and body of pancreas (n = 3) |
| Segmental narrowing of MPD in the tail of pancreas (n = 2) | Non-visualized MPD in the tail of pancreas (n = 2) |
All patients showed enlargement of the pancreas with abnormal signal intensity on T1- and T2-weighted images, though the degree of abnormal intensity was different among the cases. On T1-weighted MR images, the signal intensity of the affected pancreatic lesion was decreased compared to the signal intensity in the liver (Figure 2A). T2-weighted MR images showed increased signal intensity in the pancreatic parenchyma compared to that of the liver (Figure 2B). A capsule-like rim, which was hypointense on both T1- and T2-weighted images, was detected in 3 patients.
After steroid therapy, the portion of the main pancreatic duct that was previously not visualized on MRCP was seen (Figure 1B), and an improvement of the upstream dilatation of the proximal main pancreatic duct was evident. Stenosis or obstruction of the lower or hilar bile duct was found to be improved. The enlarged pancreas became normal in size (n = 6) or atrophic (n = 3) after steroid therapy. In all patients on both T1- and T2-weighted MR images, the abnormal signal intensity improved to being isointense with that of the liver, and the capsule-like rim disappeared (Figure 2C).
Since Yoshida et al[9] first proposed the existence of AIP in 1995, many cases of AIP have been reported. This unique form of chronic pancreatitis appears to be a distinct disease entity. AIP occurs predominantly in elderly males and frequently presents as obstructive jaundice[1,2,5-7]. This presentation is also typical of pancreatic carcinoma. As most patients with AIP respond to oral steroid therapy, an accurate diagnosis of AIP is necessary to avoid unnecessary laparotomy or pancreatic resection. Recently, MRCP has become a viable alternative to diagnostic ERCP as a non-invasive method for obtaining high quality images of the pancreaticobiliary tree[8]. We compared MRCP findings and MR images before and after steroid therapy in AIP patients.
The characteristic radiological images of AIP include irregular narrowing of the main pancreatic duct on ERCP and enlargement of the pancreas on CT and US[1-3,5-7]. The irregular narrowing of the main pancreatic duct on direct pancreatography, which is usually longer than the stenosis of the main pancreatic duct detected in patients with pancreatic carcinoma, is one of the useful findings that differentiate AIP from pancreatic carcinoma[1,3,10]. In the present study, the narrowing of the main pancreatic duct on ERCP was not visualized on MRCP, while the other region of the main pancreatic duct was visualized. After steroid therapy, the previously unvisualized lesions of the main pancreatic duct were seen. Thus, non-visualization of the main pancreatic duct might suggest narrowing of the main pancreatic duct. MRCP cannot differentiate irregular narrowing of the main pancreatic duct from stenosis of the main pancreatic duct in pancreatic carcinoma; thus, ERCP is necessary to diagnose AIP. However, MRCP findings of skipped, non-visualized main pancreatic duct lesions, accompanied by a lesser degree of upstream main pancreatic duct dilatation than that seen in pancreatic carcinoma, might suggest the presence of AIP. The MRCP of AIP patients frequently showed stenosis of the intra- or extrahepatic bile duct. T1-weighted MR images of AIP patients showed enlargement of the pancreas with decreased signal intensity, while T2-weighted MR images showed increased signal intensity, sometimes associated with a hypointense capsule-like rim in the involved segments. In previous reports, a decreased signal intensity on T1-weighted MR images, reflecting fibrosis in the pancreatic parenchyma, has been reported. Irie et al.[11] noted the hypointense capsule-like rim in the involved segment on T2-weighted MR images; this appears to be a characteristic finding of AIP, and is thought to be related to an inflammatory process involving peripancreatic tissue.
There have been no previous reports dealing with the change in the intensity in the pancreas of patients with AIP after steroid therapy. In the present study, on both T1- and T2-weighted MR images, abnormal signal intensity of the pancreas improved to isointensity with that of the liver. The enlargement of the pancreas and the capsule-like rim disappeared. Thus, MRCP and MR images are useful for evaluating the effectiveness of steroid therapy.
In conclusion, MRCP cannot differentiate the irregular narrowing of the main pancreatic duct seen with AIP from the stenosis of the main pancreatic duct seen with pancreatic carcinoma. However, the MRCP findings of skipped, non-visualized main pancreatic duct lesions, accompanied by a lesser degree of upstream dilatation of the main pancreatic duct, might suggest the presence of AIP. These MRCP findings, in conjunction with MR images of pancreatic enlargement showing abnormal signal intensity on T1- and T2-weighted MR images, are useful in supporting a diagnosis of AIP.
| 1. | Okazaki K, Chiba T. Autoimmune related pancreatitis. Gut. 2002;51:1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 269] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 2. | Kamisawa T, Egawa N, Nakajima H, Tsuruta K, Okamoto A. Morphological changes after steroid therapy in autoimmune pancreatitis. Scand J Gastroenterol. 2004;39:1154-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 61] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Kamisawa T, Tu Y, Egawa N, Nakajima H, Tsuruta K, Okamoto A. Involvement of pancreatic and bile ducts in autoimmune pancreatitis. World J Gastroenterol. 2006;12:612-614. [PubMed] |
| 4. | Kamisawa T, Yoshiike M, Egawa N, Nakajima H, Tsuruta K, Okamoto A. Treating patients with autoimmune pancreatitis: results from a long-term follow-up study. Pancreatology. 2005;5:234-238; discussion 234-238;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 103] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 5. | Kamisawa T, Egawa N, Nakajima H, Tsuruta K, Okamoto A, Kamata N. Clinical difficulties in the differentiation of autoimmune pancreatitis and pancreatic carcinoma. Am J Gastroenterol. 2003;98:2694-2699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 165] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 6. | Kamisawa T, Okamoto A, Funata N. Clinicopathological features of autoimmune pancreatitis in relation to elevation of serum IgG4. Pancreas. 2005;31:28-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 107] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 7. | Okazaki K. Autoimmune pancreatitis is increasing in Japan. Gastroenterology. 2003;125:1557-1558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 42] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Vaishali MD, Agarwal AK, Upadhyaya DN, Chauhan VS, Sharma OP, Shukla VK. Magnetic resonance cholangiopancreatography in obstructive jaundice. J Clin Gastroenterol. 2004;38:887-890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Yoshida K, Toki F, Takeuchi T, Watanabe S, Shiratori K, Hayashi N. Chronic pancreatitis caused by an autoimmune abnormality. Proposal of the concept of autoimmune pancreatitis. Dig Dis Sci. 1995;40:1561-1568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1044] [Cited by in RCA: 931] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 10. | Horiuchi A, Kawa S, Hamano H, Hayama M, Ota H, Kiyosawa K. ERCP features in 27 patients with autoimmune pancreatitis. Gastrointest Endosc. 2002;55:494-499. [PubMed] |
| 11. | Irie H, Honda H, Baba S, Kuroiwa T, Yoshimitsu K, Tajima T, Jimi M, Sumii T, Masuda K. Autoimmune pancreatitis: CT and MR characteristics. AJR Am J Roentgenol. 1998;170:1323-1327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 219] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
S- Editor Pan BR L- Editor Kumar M E- Editor Bai SH