INTRODUCTION
Gastrointestinal stromal tumors (GISTs) are a group of mesenchymal neoplasms that arise from Cajal cells which are pacemaker cells of the gastrointestinal tract[1]. These tumors occur predominantly in middle-aged and older persons, and approximately 70% of the tumors are found in the stomach, 20%-30% are found in the small intestine, and less than 10% elsewhere in the gastrointestinal tract[1,2]. Recent studies have shown that cells GISTs express a growth factor receptor with tyrosine kinase activity termed c-kit[2]. This gene product appears to be the most specific diagnostic criterion for the diagnosis of GISTs[3]. The ligand for the c-kit receptor is the stem-cell factor, also known as the steel factor or c-kit ligand[4]. Mutations of c-kit that cause constitutive activation of the tyrosine kinase function of c-kit are detectable in most GISTs and appear to play a central part in their pathogenesis[2,5]. These mutations result in ligand-independent tyrosine kinase activity, autophosphorylation of c-kit, uncontrolled cell proliferation, and stimulation of downstream signaling pathways, including those involving phosphatidylinositol 3-kinase and mitogen-activated protein kinases. GISTs are notoriously unresponsive to conventional chemotherapy, and there is no effective therapy for the advanced, metastatic stage of this disease[6]. In this study, we used imatinib (STI571 or Glivec, Novartis, Basel, Switzerland)[7], an inhibitor of the tyrosine kinase activity of c-kit, for a patient with a GIST with multiple liver metastases.
CASE REPORT
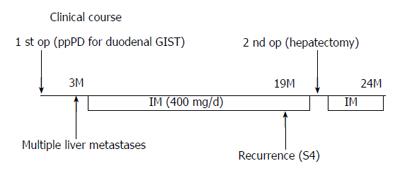
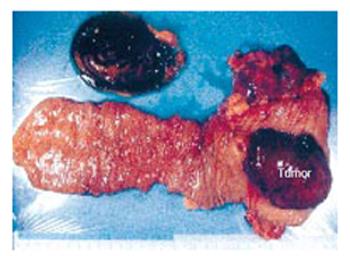
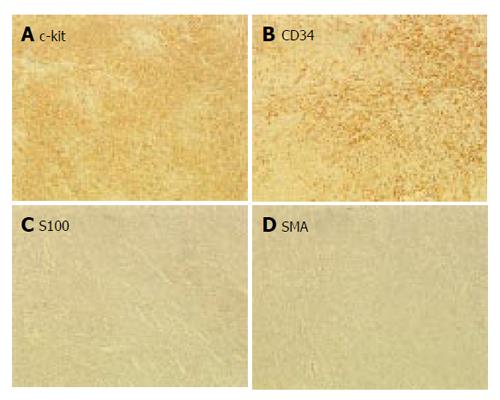
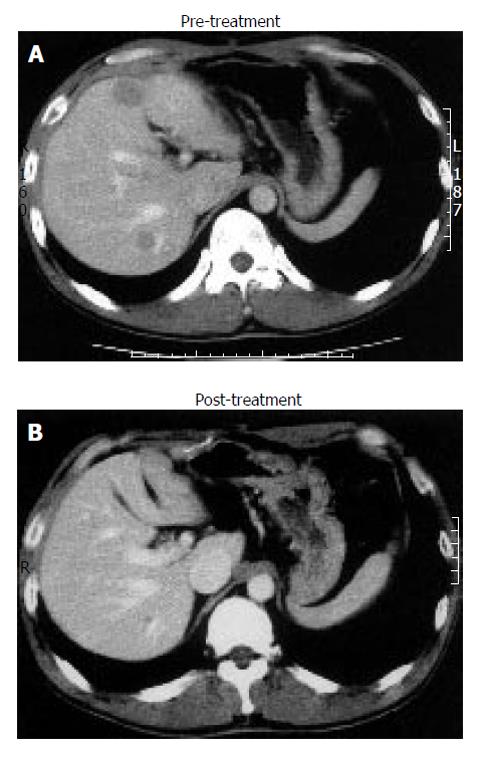
In January 2003, a 37-year-old, previously healthy man, presented with mild abdominal discomfort and a large mass in the upper abdomen. Examination with upper gastrointestinal tract led to removal of the tumor in the second portion of the duodenum by means of pancreaticoduodenectomy (PD). Clinical course of the operations (pancreaticoduodenectomy for the duodenal GIST and partial resection of recurrence tumor) and IM treatment are illustrated in Figure 1. The resected specimen is shown in Figure 2. In the second portion of the duodenum, a tumor of 5 cm in diameter was observed. Immunohistochemistry showed the tumor cells to be c-kit-positive, CD34-positive, SMA-negative, and S100-negative (Figure 3), indicating the tumor as a GIST. Histologic examination of the specimens revealed more than 20 cells per 10 high-power fields undergoing mitosis and identified the masses as a GIST. The diagnosis was confirmed by immunostaining for CD117, and c-kit mutation consisting of point mutation in exon 11 was detected in tumor DNA amplified by polymerase chain reaction[8]. Three months later, in April 2003, multiple recurrent tumors in the liver were detected by magnetic resonance imaging (MRI) and PET (Figures 4 and 5).
Figure 1 Clinical course of the patient illustrating the operations (pancreaticoduodenectomy for duodenal GIST and partial resection of recurrence tumor) and IM treatment.
Figure 2 Surgical specimen obtained by pancreaticoduodenectomy of the duodenal GIST.
Figure 3 Immunohistochemical analysis of the duodenal GIST.
A: c-kit; B: CD34; C: S100; D: SMA.
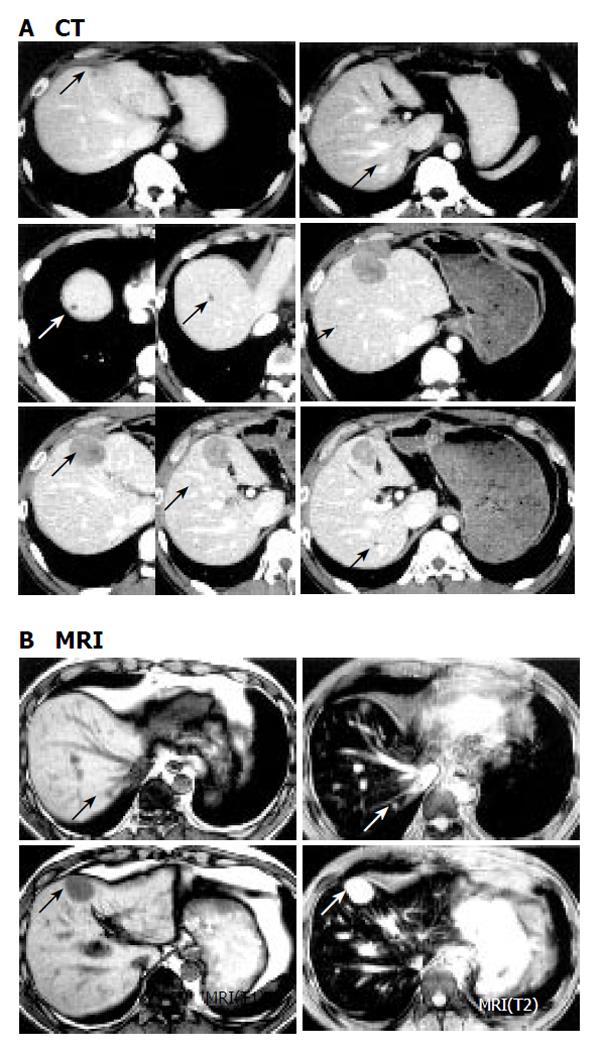
Figure 4 Abdominal MRI showing multiple liver metastases and complete remission in response to imatinib therapy.
Panel A: MRI images of the patient with multiple liver metastases after 3 mo of pancreaticoduodenectomy for malignant duodenal GIST; Panel B: Follow-up MRI images after 1 mo of oral imatinib therapy at 400 mg daily.
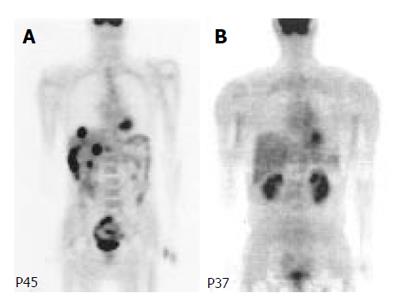
Figure 5 PET scan of liver metastases before and after imatinib treatment.
A: pretreatment with imatinib; B: posttreatment with imatinib.
The patient was then treated with imatinib after his written informed consent had been obtained. Treatment with four 100 mg capsules of imatinib once daily was started in May 2003. This dose was based on evaluations of the safety and tolerability of imatinib for patients with chronic myeloid leukemia[9]. Toxicity was assessed at follow-up visits every two to four weeks, and blood cell counts and blood chemistry were examined every one to two weeks. The response to treatment was assessed with dynamic MRI and PET with 18F-fluorodeoxyglucose as a tracer.
When measured as the sum of the products of the two perpendicular axes of each of six large liver metastases, the size of the tumor one day before the start of imatinib treatment was 42 cm2, but subsequent MRI scans showed that the size of the tumor had been reduced to 1 cm2. No enhancement was seen on dynamic MRI obtained during the treatment, and many of the metastases became hypodense. Until October 2004, the tumors at all sites had continued to respond to the treatment, and the patient had remained clinically well. Multiple liver metastases and increased accumulation of 18F-fluorodeoxyglucose were observed on the first PET obtained 4 d before the treatment with imatinib was started. One month after the treatment, PET scan showed no abnormal uptake of 18F-fluorodeoxyglucose in the liver. On the PET scan obtained after two months of the imatinib treatment, cold areas with less uptake of 18F-fluorodeoxyglucose than in the surrounding liver parenchyma were seen at the sites of liver metastases.
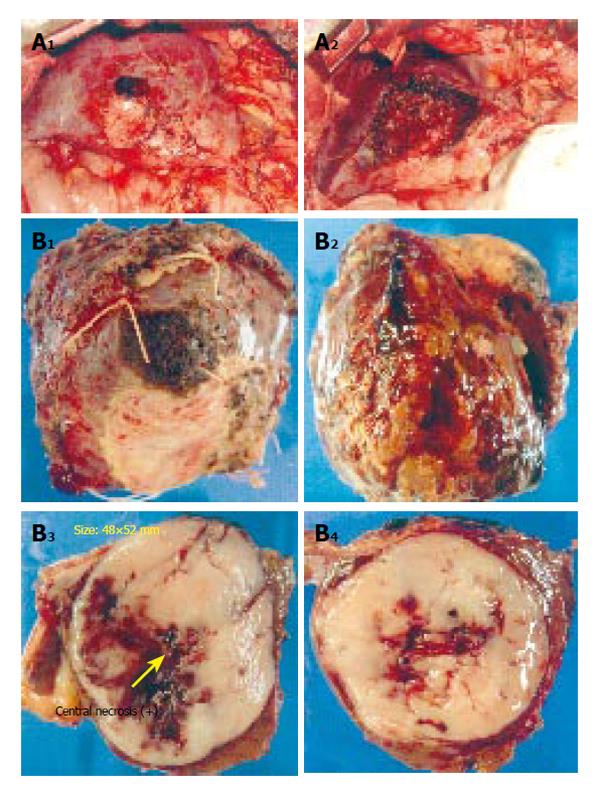
Although the response to treatment was initially CR and continued for 16 mo, single liver metastasis showed regrowth in the left lobe of the liver (S4) during the imatinib treatment. Other sites remained hypodense and no sign of recurrence was seen (Figure 6). Partial resection of recurrent tumor resulted a satisfactory postoperative course and the patient remains still alive without recurrence for 24 mo since the initial treatment with IM. The effect of IM treatment on other liver metastases besides the lesion of left hepatic lobe continued (Figures 6 and 7).
Figure 6 Abdominal CT and MRI showing recurrence of liver metastasis.
A: CT; B: MRI.
Figure 7 Surgical specimen of partial hepatectomy for GIST recurrence.
A: Operative findings; B: Resected specimens.
Mutation analysis of c-kit in exons 7, 11, and 13 was performed in the primary tumor as well as recurrent tumor as previously described[9]. Primary tumor showed the c-kit mutation at exon 11 codon 567-576 (AAT TAT GTT TAC ATA GAC CCA ACA CAA CTT → GAA), and an additional mutation was observed at exon 17 codon 820 GAT(Asp) to GGT(Gly) in recurrent tumor in the liver.
DISCUSSION
There is no effective therapy for unresectable or metastastic GIST, which is invariably fatal. The management of unresectable or metastatic GISTs has been difficult because they are resistant to conventional chemotherapy and radiation.
Imatinib, a phenylaminopyrimidine derivative, is a small molecule that selectively inhibits the enzymatic activity of several tyrosine kinases, including ABL and the BCR-ABL fusion protein of chronic myeloid leukemia and Philadelphia chromosome-positive acute lymphoblastic leukemia. This selective activity of imatinib suggests that its inhibition of the constitutively active mutant c-kit tyrosine kinase seen in GIST can be an effective therapy for these tumors. Our patient had a rapidly progressive metastatic GIST. He showed a complete metabolic response within one month after the start of imatinib treatment, as shown by negative findings on PET, which indicated reduced tumor viability. In this case, histopathological evaluation and serial MRI analysis could not be performed soon, but dramatic shrinkage of the metastastic liver tumors was observed within two months. The close relation between clinical outcome and the findings on 18F-fluoro-2-deoxy-D-glucose PET scanning indicates that such scanning is a useful complement to standard anatomical imaging with CT or MRI for monitoring the therapeutic effect of imatinib in patients with GISTs. Side effects of imatinib include nausea, diarrhea, edema, leukocytopenia, GI tract bleeding, liver dysfunction and so on[10]. In our case, however, only mild liver dysfunction was observed, and treatment with imatinib could be continued safely. This effect continued for more than 16 mo and there has been no sign of the recurrence. However, recurrence was subsequently detected and partial resection of recurrent tumor was performed.
It has been reported that the initial phase II study of imatinib treatment for metastatic GIST reported long-lasting responses in patients who followed up for 13 mo. However, it has become evident with extended follow-up that tumor progression can occur despite initially positive responses to imatinib therapy. The median duration of the responses was 19 mo for a series of patients with 2-year progression-free survival rate of 38%, which is a substantial drop from 90% at a 1 year[11]. Similar to previously reported cases, our case showed recurrence 16 mo after initial treatment with IM in one of six metastatic lesions. Resectability was confirmed and hepatic resection of the recurrence was successfully performed. The combination of IM and surgical treatment can prolong survival as shown in our case. Therefore, if the recurrent tumor is resectable, a second operation combined with adjuvant therapy with IM should be performed. If tumor re-growth occurs, surgical treatment should thus be considered.
Several studies have reported the relationship between c-kit mutation and imatinib sensitivity[11-19]. Although the mechanism of tolerance to imatinib is still unclear, screening of kit mutation may be useful for prediction of the imatinib sensitivity and recurrence. Many kinds of c-kit mutations related to IM resistance have been reported[11,13-19]. In our case, a mutation in exon 11 of KIT was initially noted. After interruption of the treatment, an additional point mutation arose in exon 17 that caused resistance to imanitib. It has been postulated that the emergence of c-kit mutations that are resistant to imatinib-targeted therapy may account for these late treatment failures, and investigation into the biologic phenomena of imatinib resistance is an area of current research. As the mechanisms of recurrence and resistance to imatinib in GIST remains unclear, they should be investigated in detail from both the clinical and molecular biological point of view.
Imatinib is a recent and very promising treatment modality for the GIST, but complete surgical extirpation remains the only curative treatment of malignant GIST, as evidenced by our patient, who became disease-free only after resection. Even then, however, significant risk of recurrence remains, despite successful resection and imatinib treatment. Our patient’s favorable response to imatinib supports the concept that specific inhibition of tyrosine kinase is a clinically useful therapeutic intervention for tumors in which aberrant kinase signaling is critical.Depending on individual circumstances, we should choose the most desirable treatment modality, and the combination of surgical extirpation and imatinib therapy should help to improve the prognosis of GIST patients in some cases. Further studies are necessary to clarify the various mechanisms involved.
S- Editor Guo SY L- Editor Kumar M E- Editor Bai SH