Published online Apr 14, 2006. doi: 10.3748/wjg.v12.i14.2305
Revised: October 10, 2005
Accepted: November 18, 2005
Published online: April 14, 2006
Multiple myeloma is a neoplasm of mature and immature plasma cells. A 50-year-old woman with lumbago, dysphagia, and left arm pain was presented. Upper endoscopical examination was performed. There was an exudate-covered ulcer in the distal esophagus, located at 30-32 cm from the incisors, covering the whole mucosa. Histopathological examination of the specimens obtained from the lesion showed the involvement of plasma cells consistent with multiple myeloma of IgG kappa subtype. Esophageal involvement of multiple myeloma should be kept in mind in patients presenting with dysphagia.
- Citation: Pehlivan Y, Sevinc A, Sari I, Gulsen MT, Buyukberber M, Kalender ME, Camci C. An interesting cause of esophageal ulcer etiology: Multiple myeloma of IgG kappa subtype. World J Gastroenterol 2006; 12(14): 2305-2307
- URL: https://www.wjgnet.com/1007-9327/full/v12/i14/2305.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i14.2305
Multiple myeloma (MM) is a plasma-cell neoplasm characterized by skeletal destruction, renal failure, anemia and hypercalcemia. The most common symptoms at presentation are fatigue, bone pain and recurrent infections. New diagnostic criteria require the presence of at least 10% plasma cells on examination of the bone marrow (or biopsy of tissue with monoclonal plasma cells), monoclonal protein in the serum or urine, and evidence of end-organ damage[1].
Apart from the bone marrow, MM may involve any part of the body including spleen, liver, lymph nodes, thyroid, adrenal glands, ovary, testis, lung, pleura, pericardium, skin, pancreas and intestinal tract. Esophageal involvement by multiple myelomas is uncommon in the English literature. Here we report an extremely rare involvement in MM.
A 50-year-old woman was admitted to Gaziantep University Hospital with lumbago, dysphagia and left arm pain. She complained of lumbago in the last 3 mo, which deteriorated but was relieved by non-steroid anti-inflammatory drugs (NSAIDs). Dysphagia was particularly associated with solid foods over a period of month. Her severe arm pain began after lifting a heavy weight. She also complained of fatigue.
Her medical history revealed a 10-year history of hypertension and one year of type 2 diabetes mellitus. No abnormal signs were detected apart from the pale conjunctivas and the left arm pain during physical examination. She was taking gliclazide 3 mg/d and amlodipine 10 mg/d.
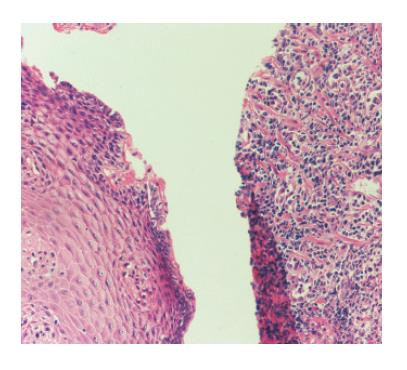
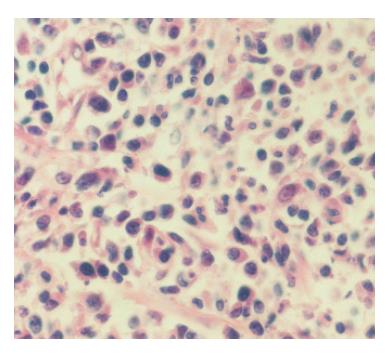
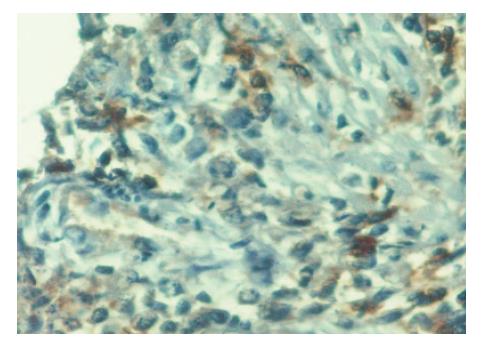
Biochemical examination and complete blood count showed (normal reference ranges are given in parenthesis) hemoglobin:102 g/L (110-180 g/L); hematocrit: 0.32 (0.35-0.60); ESR: 110 mm/h (1-18 mm/h); glucose: 160 mg/dL (70-110 mg/dL); total serum protein: 144 g/L (64-82 g/L); albumin: 22 g/L (34-50 g/L); globulin: 122 g/L (14-30 g/L); calcium: 12.6 mg/dL (8.5-10.1); (BUN, Cr, Na, Cl, and P were in the normal limits). IgG: 46.7 g/L (7-16); IgA:0.29 g/L (0.7-4); IgM:0.171 IU/mL (0.4-2.3); and IgE:184 g/L (0-100). Bone marrow aspiration and biopsy confirmed multiple myeloma (30% plasma cells) besides hyperglobulinemia, hypercalcemia, anaemia, elevated ESR, and bone pain. Multiple lytic lesions were encountered on radiographic examination of the arms, the vertebras, and the cranium. Endoscopic examination showed exudate-covered ulcer in the distal esophagus located at 30-32 cm from the incisors, covering the whole mucosa (Figure 1) and no pathological finding in the sto-mach. Histopathologic examination of the specimens obtained from the lesion showed the involvement of plasma cells in the ulcerated esophageal mucosa (Figure 2). Immunohistochemically, plasma cells revealed positive reaction with CD38, CD56, and kappa light chain and (Figure 3) negative reaction with CD20 and lambda light chain both in the bone marrow and in the esophagus (Figure 4). It was consistent with MM of IgG kappa subtype. Left upper extremity MRI revealed an irregularly shaped 5 cm × 4 cm × 6 cm mass on the humeral head. Total excision of the mass in the left arm was performed. It was also consistent with MM.
The patient was diagnosed with MM of IgG kappa subtype, and chemotherapy regimen of VAD was applied (vincristine 0.4 mg for 24 h infusion on days 1-4, adriablastina 9 mg/m2 for 24 h infusion on days 1-4, dexamethasone 40 mg po on days 1-4, 9-12, 17-20). Dysphagia was relieved after administration of the chemotherapy regimen. Control endoscopical examination revealed that the formerly detected ulcers on admission were improved.
Multiple myeloma is a neoplastic proliferation of monoclonal plasma cells that can result in osteolytic bone lesions, hypercalcemia, renal impairment, bone marrow failure, and the production of monoclonal gammopathy. Although it is usually restricted to the bone marrow, extramedullary involvement can occur in the form of plasmacytomas in up to 20% of cases. The most common site of extramedullary involvement is the upper respiratory tract, including the oropharynx, nasopharynx, nasal cavity, paranasal sinuses, and larynx[1,2]. Gastrointestinal involvement by plasma cells is rare, representing less than 5% of all extramedullary plasmacytomas. Presentation may be either primary or secondary. Before a diagnosis of multiple myeloma is made it is mandatory to exclude primary extramedullary plasmacytoma (PEMP) by performing the necessary investigations. The differential diagnosis of PEMP from multiple myeloma is important because these two entities are thought to be biologically different and their prognoses are not the same.
Most of the reported cases represent involvement of the gastrointestinal tract by solitary plasmacytomas. All segments of the gastrointestinal tract may be involved by plasma cell infiltration. Small bowel is the most common site of involvement, followed by stomach, large bowel and esophagus[2-5]. Esophageal involvement by multiple mye-loma is uncommon (Figure 3). A search of the English literature for plasmacytoma of the esophagus has revealed only four previous reports. The case reported by Morris and Pead[6] occurred in a 59-year old woman who presented with weight loss and intermittent dysphagia that progressively worsened over a 4- 5-mo period. Plasmacytoma is a protuberant mass occurring in the lower esophagus and involving the full thickness of the wall. Ahmed et al[7] encountered an esophageal PEMP in a 67-year-old man who, in addition to dysphagia, had weakness and weight loss. The lower third of the esophagus was invaded by an 8 cm tumour that extended to the gastric cardia and pene-trated the entire thickness of the esophageal wall. Davis and Boxer[8] described a PEMP of esophagus in a 69-year-old man who only had a two-week history of dysphagia. Furthermore, this patient did not have weight loss, malaise or constitutional symptoms. The tumour was polypoid, measured 4 cm in diameter, and involved the distal third of the esophagus. Recently, Chetty et al[9] described a PEMP of esophagus in a 58-year-old man. Dysphagia occurs particularly with consumption of solid foods over a period of 2 mo. Gross examination of esophagus can reveal large polypoid tumour. In the present case, however, dysphagia was particularly with solid foods over a period of one month. The lesion was in the form of ulcer and was pro-bably induced by impairment of the esophageal mucosa due to replacement of the stromal tissue by the plasma cells (Figure 4).
The presenting features of esophageal plasmacytoma are similar to esophageal carcinoma, i.e., progressive dysphagia, profound weight loss, signs of malnutrition, and anemia. Diagnosis on clinical grounds alone is impossible and the radiologic appearance does not seem distinctive. Endoscopic biopsy is the earliest opportunity for diagnosis.
Diffuse plasma cell infiltration may also be seen in Barrett’s esophagus that should be ruled out in the differential diagnosis. Plasma cells are positive for monoclonal light chain in MM as in the present case, but they are polyclonal in Barrett’s esophagus. Additionally, there was no intestinal glandular metaplasia in the present case.
In conclusion, multiple myeloma is a systemic disease which may be rarely presented with esophageal involvement. It should be kept in mind that esophageal ulcers in patients diagnosed with MM may be related to the myeloma involvement and these patients should be examined further.
| 1. | Kyle RA, Rajkumar SV. Multiple myeloma. N Engl J Med. 2004;351:1860-1873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1078] [Cited by in RCA: 1082] [Article Influence: 49.2] [Reference Citation Analysis (0)] |
| 2. | DOLIN S, DEWAR JP. Extramedullary plasmacytoma. Am J Pathol. 1956;32:83-103. [PubMed] |
| 3. | Sloyer A, Katz S, Javors FA, Kahn E. Gastric involvement with excavated plasmacytoma: case report and review of endoscopic criteria. Endoscopy. 1988;20:267-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Pimentel RR, van Stolk R. Gastric plasmacytoma: a rare cause of massive gastrointestinal bleeding. Am J Gastroenterol. 1993;88:1963-1964. [PubMed] |
| 5. | Goeggel-Lamping C, Kahn SB. Gastrointestinal polyposis in multiple myeloma. JAMA. 1978;239:1786-1787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Morris WT, Pead JL. Myeloma of the oesophagus. J Clin Pathol. 1972;25:537-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Ahmed N, Ramos S, Sika J, LeVeen HH, Piccone VA. Primary extramedullary esophageal plasmacytoma: First case report. Cancer. 1976;38:943-947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Davies RA, Boxer DI. Primary plasmacytoma of the oesophagus. Br J Radiol. 1988;61:1180-1181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Chetty R, Bramdev A, Reddy AD. Primary extramedullary plasmacytoma of the esophagus. Ann Diagn Pathol. 2003;7:174-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
S- Editor Wang J L- Editor Wang XL E- Editor Bi L