Published online Apr 7, 2006. doi: 10.3748/wjg.v12.i13.2086
Revised: September 21, 2005
Accepted: October 9, 2005
Published online: April 7, 2006
AIM: To evaluate whether an automatically controlled cut system (endocut mode) could reduce the complication rate of endoscopic sphincterotomy (EST) and serum hyperamylasemia after EST compared to the conventional blended cut mode.
METHODS: From January 2001 to October 2003, 134 patients with choledocholithiasis were assigned to either endocut mode group or conventional blended cut mode group at the time of sphincterotomy. The two groups were retrospectively compared for the complications after EST and serum amylase level before and 24 h after the procedure.
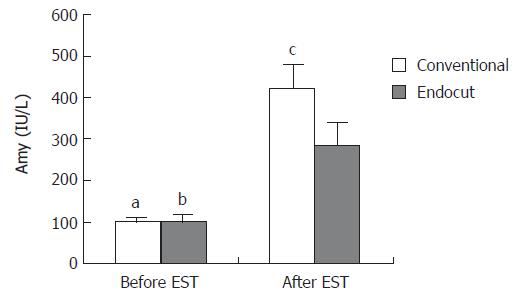
RESULTS: Of the 134 patients treated, 79 were assigned to conventional blended cut mode group and 55 to endocut mode group. There was no significant difference in age, sex, and serum amylase level before EST between the two groups. Complications were found in 5 patients of the endocut mode group (9%): hyperamylasemia (5 times higher than normal) in 4 and moderate pancreatitis in 1. Complications were found in 13 patients of the conventional blended cut mode group (16%): hyperamylasemia in 12 and moderate pancreatitis in 1. Serum amylase levels were elevated in both groups 24 h after EST (P < 0.02). The average serum amylase level 24 h after EST in the conventional blended cut mode group was significantly higher than that in the endocut mode group (P < 0.05).
CONCLUSION: Endocut mode offers a safety advantage over conventional blended cut mode for pancreatitis after EST by reducing hyperamylasemia.
- Citation: Akiho H, Sumida Y, Akahoshi K, Murata A, Ouchi J, Motomura Y, Toyomasu T, Kimura M, Kubokawa M, Matsumoto M, Endo S, Nakamura K. Safety advantage of endocut mode over endoscopic sphincterotomy for choledocholithiasis. World J Gastroenterol 2006; 12(13): 2086-2088
- URL: https://www.wjgnet.com/1007-9327/full/v12/i13/2086.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i13.2086
The main complications of endoscopic sphincterotomy (EST) are pancreatitis, hemorrhage, perforation and sepsis[1-4]. Acute pancreatitis is still the most common complication associated with the procedures. Testoni et al[5] have shown that pancreatitis is associated with the elevation of serum amylase level 24 h after ERCP/EST.
An automatically controlled cut system, endocut mode (ICC 200 ERBE), can reduce the danger of papillary hemorrhage but may lead to pancreatitis[6]. This study was to evaluate whether the endocut mode could reduce the complication rate of EST and serum hyperamylasemia after EST compared to the conventional blended cut mode.
From January 2001 to October 2003, 134 patients admitted to Aso Iizuka Hospital due to choledocholithiasis were assigned to either endocut mode group or conventional blended cut mode group at the time of EST. Three gastroenterologists performed the procedure. An Olympus UES-10 electrosurgical generator (Olympus, Japan) was used for conventional cut with the blended current set at output limit 30W and the coagulation current set at output limit 15W. An Erbe ICC200 (Erbe, Germany) was used for endocut with the effect 3 current set at output limit 120W and forced coagulation current set at output limit 30W.
The two groups were retrospectively compared for the complications, pancreatitis, hemorrhage after EST and serum amylase level before and 24 h after the procedure. Pancreatitis was defined when CT grade was higher than grade II (local pancreas swelling). A bleeding complication was defined when the patient required blood transfusion or had a drop in hematocrit level greater than 5%.
Results were presented as mean ± SE. Complications in the two groups were evaluated using χ2 test and Fisher’s exact test. Differences in serum amylase levels between the two groups were evaluated by Student’s t test. P < 0.05 was considered statistically significant.
One hundred and thirty-four patients were evaluated in this study. Seventy-nine patients underwent conventional blended cut and 55 patients underwent endocut. There were no significant differences in age and sex distribution as well as serum amylase level before EST (Table 1).
| Number of patients | Yr | Male (%) | Female (%) | Amylase(IU/L) | |
| Conventional cut group | 79 | 73.5 ± 1.3 | 54 | 46 | 102 ± 8 |
| Endocut group | 55 | 70.8 ± 1.8 | 56 | 44 | 101 ± 18 |
Complications were found in 5 patients of the endocut mode group (9%): hyperamylasemia in 4 (serum amylase level was 5 times higher than normal) and moderate pancreatitis in 1 patient. On the other hand, complications were found in 13 patients of the conventional blended cut mode group (16%): hyperamylasemia in 12 patients and moderate pancreatitis in 1 patient (Table 2). One patient in each group had mild bleeding not showing hematocrit decrease. No major complications such as perforation were found in both groups. There were no significant differences in the incidence of complications such as pancreatitis, hemorrhage, and hyperamylasemia between the two groups.
| Hyperamylasemia( > 5 times upper normal limit) | Pancreatitis | |
| Conventinal cut group | 12 | 1 |
| Endocut group | 4 | 1 |
Serum amylase levels were elevated in both groups 24 h after EST (P < 0.02). The average serum amylase level 24 h after EST in the conventional blended cut mode group was significantly higher than that in the endocut mode group (P < 0.05, Figure 1).
Since the introduction of EST, the indications for the procedure have grown steadily. The complications of EST are similar to those of diagnostic ERCP but occur more frequently. Freeman et al[3] have shown that the incidence of pancreatitis after EST is 5.4% and significant risk factors for pancreatitis are sphincter of Oddi dysfunction, younger age, the number of pancreatic contrast injections, precut sphincterotomy, and difficulty of cannulation. Elta et al[7] reported that the type of electrocautery current affects this risk and found that the use of pure cut current is associated with a lower incidence of pancreatitis rather than blended current.
A new high-frequency current generator equipped with an automatically controlled system (endocut mode) has been currently used in EST. With endocut mode, each interval of cutting is automatically triggered by the initial electric arc sensor within the ICC 200 and is thus reproducible in duration. The automatically-fractionated cut and controlled cutting speed can prevent perforation of the major papilla[6].
In this study, we observed the most common complications such as moderate pancreatitis and mild hemorrhage in both groups, which are consistent with the other reports[3,4,6,7]. The endocut mode could reduce hemorrhage after EST[6,9-10], but leads to pancreatitis[6]. On the other hand, Ellahi et al[11] reported that the endocut mode does not offer a safety advantage over the conventional blended cut mode. In this study, there were no significant differences in the incidence of complications such as pancreatitis and hemorrhage between the two groups. The rate of hyperamylasemia (serum amylase level was 5 times higher than normal) was 7% in the endocut mode group and lower than 15% in the conventional blended cut mode group. But there was no significant difference in the incidence of hyperamylasemia between the two groups. In this study, the number of patients might be too small to have a statistical significance as for the incidence of complications.
A larger study is needed for the evaluation of usefulness about the endocut mode in EST, because the number of patients was less than 150 in this and other studies[6,9-11]. It was reported that the endocut mode reduces hemorrhage after EST[8]. Our results showed that the average serum amylase level 24 h after EST in the endocut mode group was significantly lower than that in the conventional blended cut mode group (P< 0.05), which is consistent with study of Shinozuka et al[9]. In this study, in comparison with a conventional blended cut mode unit, all the examiners noted the smooth, easy EST by the endocut mode unit. Thus it might shorten the procedure time, lower the risk of major papilla’s edema as well as the number of contrast injections and the serum amylase level after EST.
The endocut mode offers a safety advantage over conventional blended cut mode for pancreatitis after EST by reducing the hyperamylasemia.
| 1. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1890] [Cited by in RCA: 2085] [Article Influence: 59.6] [Reference Citation Analysis (2)] |
| 2. | Lambert ME, Betts CD, Hill J, Faragher EB, Martin DF, Tweedle DE. Endoscopic sphincterotomy: the whole truth. Br J Surg. 1991;78:473-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 82] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1716] [Cited by in RCA: 1703] [Article Influence: 56.8] [Reference Citation Analysis (2)] |
| 4. | Huibregtse K. Complications of endoscopic sphincterotomy and their prevention. N Engl J Med. 1996;335:961-963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 69] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Testoni PA, Bagnolo F. Pain at 24 hours associated with amylase levels greater than 5 times the upper normal limit as the most reliable indicator of post-ERCP pancreatitis. Gastrointest Endosc. 2001;53:33-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Kohler A, Maier M, Benz C, Martin WR, Farin G, Riemann JF. A new HF current generator with automatically controlled system (Endocut mode) for endoscopic sphincterotomy--preliminary experience. Endoscopy. 1998;30:351-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 48] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Elta GH, Barnett JL, Wille RT, Brown KA, Chey WD, Scheiman JM. Pure cut electrocautery current for sphincterotomy causes less post-procedure pancreatitis than blended current. Gastrointest Endosc. 1998;47:149-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 72] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Perini RF, Sadurski R, Patel RG, Payne KM, Hawes RH, Cotton PB, Cunningham JT. Post-sphincterotomy bleeding: Has the ERBE electrocautery helped. Gastrointest Endosc. 2001;53:AB89 Abstract. [DOI] [Full Text] |
| 9. | Shinozuka N, Koyama I, Minoshima T, Tawara H, Kamisasa N, Watanabe T, Matsumoto T, Anzai H, Kyo S. Effect of automatically controlled system (Endocut mode) in endoscopic sphincterotomy. Nihongekakeirengougakkaisi. 2001;26:41-44. |
| 10. | Kida M, Kikuchi H, Araki M, Takezawa M, Watanaba M, Kida Y, Imaizumi H, Saigenji K. Randomized control trial of EST with either endocut mode or conventional pure cut mode. Gastrointest Endosc. 2004;59:201 Abstract. [DOI] [Full Text] |
| 11. | Ellahi W, Kasmin FE, Cohen SA, Siegel JH. "Endocut" technique versus pure cutting current for endoscopic sphincterotomy: a comparison of complication rates. Gastrointest Endosc. 2001;53:AB95 Abstract. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
S- Editor Wang J L- Editor Wang XL E- Editor Ma WH