Published online Feb 14, 2005. doi: 10.3748/wjg.v11.i6.899
Revised: September 15, 2004
Accepted: October 8, 2004
Published online: February 14, 2005
AIM: To study the practical use of the model for end-stage liver disease (MELD) on clinic and assess its validity by the concordance (C)-statistic in predicting the prognosis of the patient with severe viral hepatitis.
METHODS: One hundred and twenty-one patients were divided into plasma exchange group and non-plasma exchange group, and were graded with MELD formula. The death rate was observed within 3 mo.
RESULTS: Eighty-one patients died within 3 mo (35 cases in PE group, 46 cases in non-PE group). The mortality of patients in PE group whose MELD score between 20-30 and 30-40 were 31.6% and 57.7%, respectively, but in non-PE cases they were 67.6%, 81.3% respectively. There was significant difference between PE group and non-PE group (P<0.05). However, the mortality of patients whose MELD score higher than 40 were 93.3% in PE group and 100% in non-PE group and there was no significant difference between the two groups (P = 0.65>0.05). The optimal cut-off values of MELD to predict the prognosis of patients were 30 in PE group whose sensitivity, specificity and C-statistic were 80.0%, 52.0% and 0.777, but in non-PE group they were 25, 82.6%, 86.7% and 0.869, respectively.
CONCLUSION: The MELD score can act as a disease severity index for patients with severe viral hepatitis, and the mortality of the patient increases with the increase of the MELD score. The MELD can accurately predict the short-term prognosis of patients with severe viral hepatitis.
- Citation: Weng ZH, Cai SQ. Analysis of prognosis on patients with severe viral hepatitis using the model for end-stage liver disease. World J Gastroenterol 2005; 11(6): 899-902
- URL: https://www.wjgnet.com/1007-9327/full/v11/i6/899.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i6.899
Viral hepatitis is one of the diseases endangering people’s health worldwide, especially patients with severe viral hepatitis (severe hepatitis in short) with bad prognosis and a high mortality. Despite exploitation of new medicines and continuous advances in supporting therapy, mortality of patients undergoing conservative therapy of internal medicine is still reaching 60-80%[1]. It is important to establish a good method to estimate the prognosis of severe hepatitis, assess the severity of disease and development direction afterwards in order to select reasonable and effective therapy on the basis of relative clinical information.
These years, the establishment of Artificial Liver Support System (ALSS) provides important methods for the treatment of severe hepatitis, of which plasma exchange has become a relatively mature method in many hospitals. However, in the absence of unity of the index to estimate the therapy effect, people lack uniform cognition about the clinical effect of plasma exchange.
This study uses the model for end-stage liver disease (MELD)[2] to predict the short-term(3 mo) prognosis of patients with severe viral hepatitis and assess its practical value on clinic.
One hundred and twenty-one hospitalized patients with severe hepatitis diagnosed according to the diagnostic standards recommended in Xian National Hepatopathy Meeting in 2000[3] from April of 2001 to August of 2003 were recruited for the study. We collected the case history of the 121 patients and they were divided into plasma exchange group and non-plasma exchange group, with 60 cases in PE group and 61 cases in non-PE group. There is no statistically significant difference between the two groups. Patients with autoimmune hepatitis, drug hepatitis, toxic hepatitis, alcoholic hepatitis and fatty liver were excluded. Comparison of the clinical statistics between the two groups is shown in Table 1.
| PE group | Non-PE group | |
| Sex (male/female) | Jul-53 | Mar-58 |
| Age (yr) | ||
| Median (range) | 42 (18-65) | 40 (18-68) |
| Etiology (cases) | ||
| B | 45 | 41 |
| B+E | 13 | 16 |
| B+C | 2 | 4 |
| Clinical type (cases) | ||
| Subacute severe hepatitis | 9 | 6 |
| Chronic severe hepatitis | 51 | 55 |
| Laboratory parameters | ||
| Serum total bilirubin (mmol/L) | 588.88 | 514.99 |
| (Range) | (217.0-1 015.5) | (293.0-1 140.3) |
| Serum creatinine (mmol/L) | 131.63 | 142.09 |
| (Range) | (43.3-401.8) | (42.0-945.0) |
| INR1 | 3.18 | 2.88 |
| (Range) | (1.90-6.60) | (1.91-7.20) |
The basic management of the two groups were the same: bed rest; venous infusion with liver-protecting medicine; transfusing blood product such as albumin and plasma; supplying energy and vitamin; maintaining electrolytic and acid-base homeostasis; preventing complications. PE group was appended with plasma exchange therapy and times of treatments were according to the state of each patient.
Patients were kept in plasma exchange therapy’s room under strict disinfection and temperature control. A dual lumen catheter placed percutaneously into the femoral vein used as a blood access. Heparin was added to prevent clotting. Plasma exchange device of M-25 made in the USA was used. The blood flow rate in PE circuit was 10-20 mL/min. The duration of PE was 3 to 4 h. Some volumes of plasma (3000-3500 mL) per PE were exchanged and replaced with homotypic fresh frozen plasma.
Function index of liver and kidney and international normalized ratio of the 121 patients tested in our hospital clinical laboratory were studied, and test data of the subsequent day after plasma exchange was compared with the data before treatment. Developments of liver disease were observed during 3-mo follow-up period from the day of hospitalization (recovery and discharge from hospital, transit to receiving liver transplantation or death for instance).
The formula for the MELD score is: score of MELD[4] = 3.8×ln [Total bilirubin (mg/dL)] +11.2× ln (INR) +9.6×ln [creatinine (mg/dL)] +6.4× (etiology: 0 if cholestatic or alcoholic, 1 otherwise). MELD score (integer) can be obtained from the official web site of American Mayo Clinic research center http://www.mayoclinic.org/gi-rst/mayomodel 5.html by inputting the patients’ clinical data.
Comparisons between groups were performed using t test, the rates were compared by χ2 test and Fisher’s exact test. The validity of MELD model in predicting the prognosis was measured by the C-statistic, which was equivalent to the area under receiver operating characteristic curve (ROC curve)[5]. Besides, the optimal cut-off values of MELD to discriminate between deceased and surviving patients with severe hepatitis were calculated by ROC curves.
Statistically, a C-statistic between 0.8 and 0.9 indicates excellent diagnostic accuracy and a C-statistic greater than 0.7 is generally considered a useful test. For prognostic models, a C-statistic of 0.9 or greater is seldom seen[6,7]. For all analyses P <0.05 was considered statistically significant. Data were analyzed with the SPSS software package for Windows.
Scores obtained by the two groups according to MELD tormula and MELD scores, of all the cases were 20 or above. Both groups were categorized into three subsets: 20≤MELD<30, 30≤MELD<40, MELD≥40 (Table 2).
| 20 ≤MELD<30 | 30 ≤MELD<40 | MELD≥40 | ||||
| PE group | Non-PE group | PE group | Non-PE group | PE group | Non-PE group | |
| Bilirubin (mmol/L) | 561.66±148.92 | 463.28±169.69 | 606.40±150.60 | 526.44±148.00 | 600.77±140.90 | 677.79±221.18 |
| INR | 2.13±0.62 | 2.34±0.67 | 3.54±1.16 | 4.14±1.24 | 4.01±1.58 | 3.58±1.69 |
| Creatinine (mmol/L) | 70.53±18.69 | 72.51±26.11 | 106.45±37.31 | 101.97±65.85 | 237.12±136.64 | 523.01±289.10 |
| MELD score | 24.7±3.1 | 24.2±3.0 | 34.7±2.2 | 32.4±7.1 | 42.7±1.7 | 48.6±5.3 |
The changes in clinical biochemical index and MELD score of the PE group after several times of plasma exchange are shown in Table 3.
| 20 ≤MELD<30 | 30 ≤MELD<40 | MELD≥40 | ||||
| Before PE | After PE | Before PE | After PE | Before PE | After PE | |
| Bilirubin (mmol/L) | 561.66±148.92 | 242.01±134.39b | 606.40±150.60 | 260.85±64.65b | 600.77±140.90 | 289.70±147.50b |
| INR | 2.13±0.62 | 1.55±0.28a | 3.54±1.16 | 1.59±0.22a | 4.01±1.58 | 2.40±1.52a |
| Creatinine (mmol/L) | 70.53±18.68 | 88.00±21.28 | 106.45±37.31 | 124.78±41.22 | 237.12±136.64 | 228.38±132.04 |
| MELD score | 24.7±3.1 | 19.7±3.5 a | 34.7±2.2 | 22.7±3.7a | 42.7±1.7 | 28.4±5.3a |
There were significant decreases in the concentrations of the serum total bilirubin, INR and MELD score between, before and after the plasma exchange treatments (Table 3). Serum creatinine level also changed after plasma exchange therapy, but without statistically significant difference (P>0.05).
The transformations of the disease of the two groups were observed from the day of hospitalization. The mortality and MELD score of all patients within 3 mo are shown in Table 4.
The study shows that the mortality of the patients with the MELD score between 20-30 and 30-40 in PE group was obviously lower than that of non-PE group. However, the mortalities of the patients with MELD score reaching or exceeding 40 in PE group and non-PE group were 93.3% and 100% respectively, and P value was 0.65 under Fisher’s exact test which means the difference between the two groups was of no statistical significance.
Using different MELD scores as cut-off value to discriminate between deceased and surviving patients, true/false positive value, true/false negativity value, and corresponding sensitivity and specificity can be obtained from four-fold table analysis of diagnostic experiment (Table 5).
| Real prognosis | Predicted prognosis | |
| Number of deaths | Number of survivors | |
| Number of deaths | Value of true positivea | Value of false negativeb |
| Number of survivors | Value of false positivec | Value of true negatived |
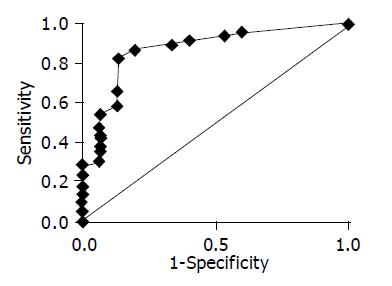
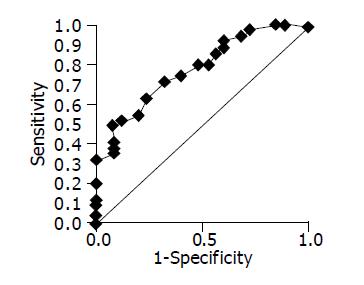
The cut-off values with the best sensitivity and specificity in predicting a 3-mo survival for MELD score were calculated using ROC curve, which gained from ROC software package with sensitivity as vertical axis and 1-specificity as horizontal axis (Figures 1, 2). The more the area under the curve, the higher the diagnostic validity[7].
Figure 1 shows the ROC curve estimating the prognosis of the non-PE group within 3 mo through MELD model. ROC analysis software can output the following results: Area under the curve is 0.869; SE is 0.055; P is less than 0.0001; 95% CI is 0.760-0.978; the optimal cut-off value is 25; corresponding sensitivity is 82.6% and specificity is 86.7%.
Figure 2 demonstrates the ROC curve estimating the prognosis of the PE group within 3 mo through MELD model. The following results can be obtained from the ROC analysis software: Area under the curve is 0.777; SE is 0.059; P is less than 0.0001; 95% CI is 0.661-0.892; the optimal cut-off value is 30; corresponding sensitivity is 80.0% and specificity is 52.0%.
MELD scoring system was originally developed to access the short-term prognosis of patients with cirrhosis hypertension undergoing the transjugular intrahepatic portosystemic shunt (TIPS) procedure by Mayo Clinic research center. MELD scoring system uses serum creatinine, total bilirubin, INR for prothrombin time and etiology of hepatopathy as indices and calculates the data through mathematical formula. Those patients with high score are of bad prognosis and greater possibility of death in short term. Besides using objective indices, this scoring system employs the renal function as an independent variable in estimating the prognosis of the hepatopathy, while other models don’t.
A European study[8] showed that 6-mo survival sensitivity, specificity and C-statistic of using MELD score of 14 as the cut-off value to discriminate between deceased and surviving patients with hepatic cirrhosis is 75%, 72% and 0.82, respectively. The MELD scoring system showed nice discriminant ability. The study also demonstrated that MELD score correlates with the degree of liver functional impairment.
Recently, scholars both at home and abroad made a lot of research and study about predicting the prognosis of the severe hepatitis, but most of them are limited to univariate analysis. Some multivariate analysis cannot be widely used in clinic due to the complexity of their indices. Most scholars discussed the plasma exchange therapy, about its improvement of symptom, mend of biochemical index and increase of survival rate, but the therapeutic effect reported by different research institutions has not been consistent with each other due to the absence of the objective of the index. The establishment of MELD scoring system solved these problems primitively.
The purpose of this study is to evaluate the ability of the MELD scoring system in discriminating the prognosis of the patients with severe hepatitis in short term (within 3 mo), and its validity in prediction is also analyzed by ROC curve, which gives out the optimal cut-off value of MELD score to discriminate between deceased and surviving patients in 3 mo.
The mortalities of patients in non-PE group whose MELD score in 20-30, 30-40 and ≥40 are 67.6%, 81.3%, 100%, respectively and the C-statistic is 0.869, which is nearer to the result of Kamath et al[2]. In PE cases they are 31.6%, 57.7% and 93.3%, respectively. MELD score can act as a severity index for the severe hepatitis, and mortality in 3 mo increases as the MELD score increases. The mortality of the patients in PE group with MELD score in 20-30 and 30-40 is significantly lower than that of non-PE group (P<0.05), thus plasma exchange therapy can increase the short-term survival rate of some patients with severe hepatitis.
Therapeutic effect of internal medicine for patients with MELD score reaching or exceeding 25 is not so well with bad prognosis in 3 mo. Plasma exchange or other artificial liver support system such as molecular absorbing recirculating system and liver transplantation should be applied early. Plasma exchange is of little effect for the patients whose MELD score is reaching or exceeding 40 and liver transplantation may be the only way to save their lives.
The following conclusions can be drawn from this study: the MELD score can act as a disease severity index for patients with severe viral hepatitis, and the mortality of the patient increases with the increase of the MELD score. The MELD can accurately predict the short-term prognosis of patients with severe viral hepatitis, and it can be popularized in clinic. Clinical doctors can rely on MELD score for reference in determining whether the patients with severe hepatitis need plasma exchange or other therapy of artificial liver, even liver transplantation and its treatment occasion, and avoiding waste of medical resources. Further studies will be required to research and develop more exact quantified method in estimating liver function, increase the prediction vitality of clinical model, in order to predict the possibility of survival/fatality of individual patient.
| 1. | Bathgate AJ, Garden OJ, Forsythe JR, Madhaven KK, Finlayson ND, Simpson KJ, Hayes PC, MacGilchrist AJ. The outcome of the first 165 orthotopic liver transplants in Scotland. Scott Med J. 1999;44:9-10. [PubMed] |
| 2. | Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, D'Amico G, Dickson ER, Kim WR. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3462] [Cited by in RCA: 3778] [Article Influence: 151.1] [Reference Citation Analysis (2)] |
| 3. | Institution of infectious disease and verminosis of Chinese Medical Institution, Branch of hepatology. Prevention blue print for viral hepatitis. Zhonghua Ganzangbing Zazhi. 2000;8:324-329. |
| 4. | Forman LM, Lucey MR. Predicting the prognosis of chronic liver disease: an evolution from child to MELD. Mayo End-stage Liver Disease. Hepatology. 2001;33:473-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 149] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 5. | Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13773] [Cited by in RCA: 12591] [Article Influence: 286.2] [Reference Citation Analysis (1)] |
| 6. | Zweig MH, Campbell G. Receiver-operating characteristic (ROC) plots: a fundamental evaluation tool in clinical medicine. Clin Chem. 1993;39:561-577. [PubMed] |
| 7. | van Erkel AR, Pattynama PM. Receiver operating characteristic (ROC) analysis: basic principles and applications in radiology. Eur J Radiol. 1998;27:88-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 142] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 8. | Botta F, Giannini E, Romagnoli P, Fasoli A, Malfatti F, Chiarbonello B, Testa E, Risso D, Colla G, Testa R. MELD scoring system is useful for predicting prognosis in patients with liver cirrhosis and is correlated with residual liver function: a European study. Gut. 2003;52:134-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 246] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
Assistant Editor Li WZ Edited by Gabbe M