Published online Oct 21, 2005. doi: 10.3748/wjg.v11.i39.6219
Revised: September 23, 2004
Accepted: September 30, 2004
Published online: October 21, 2005
Primary biliary cirrhosis (PBC) is an autoimmune disease characterized by anti-mitochondrial antibodies and destruction of intra-hepatic bile ducts. Though little is known about the etiology of PBC, some reports suggest that xenobiotics and viral infections may induce PBC. We describe a case of PBC after the aortoiliac reconstruction surgery using a Y-graft.
- Citation: Inoue T, Shiraki K, Fuke H, Yamanaka Y, Miyashita K, Ito K, Suzuki M, Sugimoto K, Murata K, Nakano T. Primary biliary cirrhosis after aortoiliac reconstruction surgery using a Y-graft: A case report. World J Gastroenterol 2005; 11(39): 6219-6220
- URL: https://www.wjgnet.com/1007-9327/full/v11/i39/6219.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i39.6219
Primary biliary cirrhosis (PBC) is a chronic inflammatory process primarily affecting the medium-sized intra-hepatic bile ducts, leading to chronic cholestasis and often progressing to cirrhosis and liver failure, which requires liver transplantation. PBC is thought of as an autoimmune disease because it is closely associated with various immunological abnormalities, the hallmark being the presence of anti-mitochondrial antibodies in over 95% of patients.
A 61-year-old male was admitted to our hospital in September 1995 with biochemical cholestasis and abnormal liver function tests. He had taken anti-hypertensive agents (amlodipine and betaxolol) since February 1995. His blood examination sometimes presented very mild biochemical cholestasis without any symptoms. Viral hepatitis was denied, but autoantibody was not checked at that time. Earlier in March 1995, he had an abdominal aortic aneurysm and underwent aortoiliac reconstruction using a Y-graft. Ten days after the surgery, his chemistry showed marked cholestasis, including alkaline phosphatase levels 5-10 times the upper limit of normal and gamma glutamyltransferase levels 5-15 times higher than the upper limit of normal. At first, drug-induced cholestasis was suspected and he started other anti-hypertensive medications (nifedipine and imidapril). Cholestasis improved after changing these medications for a while, but it worsened in August 1995. On admission to our hospital in September 1995, he denied any preceding or on-going fever, flu-like illness, pruritus, abdominal pain, anorexia, vomiting, joint pain, dry eyes, or skin rashes. He denied previous blood transfusion, iv drug abuse, or alcohol abuse. There was no family history of liver disease or malignancy.
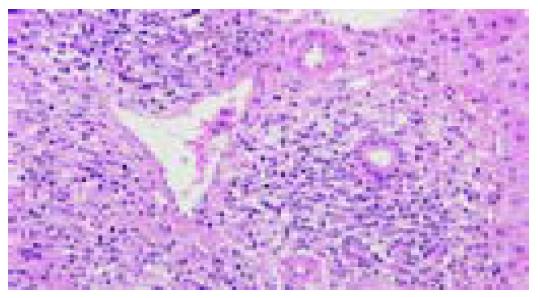
Physical examination revealed mild hepatomegaly, but no ascites or mass. The laboratory data showed an alkaline phosphatase level of 572 IU/L, a gamma glutamyltransferase level of 726 IU/L, an AST of 43 IU/L, an ALT of 30 IU/L, a total bilirubin of 0.5 g/dL, a direct bilirubin of 0.2 g/dL, an IgG level of 2 180, an IgM level of 384, and a total cholesterol level of 204 mg/dL. Antinuclear antibody titer was 1 280-fold beyond the upper normal limit, anti-smooth muscle antibody was 80-fold, and anti-mitochondrial antibody was 80-fold higher. A hepatitis profile for hepatitis B and C was negative. An abdominal ultrasound revealed a slightly atrophic liver with dull edge, dilated common bile duct (12 mm), and a gallbladder stone. His liver biopsy showed inflammatory destruction of the intrahepatic septal and interlobular bile ducts within the portal space, and expanded portal tracts by lymphocytes with sparse neutrophils or eosinophils, suggesting PBC (stage I by Scheuer staging) (Figure 1).
A diagnosis of asymptomatic PBC was established on the basis of cholestasis, a positive AMA, and the histological findings. The patient was started on ursodeoxycholic acid 600 mg thrice a day, with a positive response to the cholestasis.
PBC is a chronic cholestatic liver disease of unknown cause. Progressive bile duct injury from portal and periportal inflammation could result in progressive fibrosis and eventually cirrhosis. Evidence to date suggests that immunological and genetic factors might cause the disease. Evidence for an immunologic cause of PBC includes immunohistochemical data showing the presence of activated T cells in areas of bile duct destruction and the presence of highly specific autoantibodies reactive with antigens on the surface of biliary epithelial cells. Environmental factors[1] and infectious agents[2-4] also may trigger an autoimmune attack. Other reports suggest that the disease may be induced by xenobiotics and that halogenated compounds will bind to the PDC-E2 autoantigen, breaking tolerance and leading to an intense mucosal response[5]
Our patient had mild cholestasis before the operation and developed marked biochemical cholestasis after the aortoiliac reconstruction using a Y-graft. This suggests that he may have been in the very early stages of PBC before the surgery and the graft implantation might have exacerbated the autoimmune response, leading to further bile duct injury. The trigger might be the graft itself or the drugs used in the perioperative period. There is only one case report of PBC after graft replacement for abdominal aortic aneurysm[6], in which the graft itself was considered to induce the autoimmune response, resulting in liver injury. Some reports suggest that xenobiotics are metabolized in the liver, thereby increasing the potential for liver-specific alteration of proteins, and that a liver-specific autoimmune disease can be observed in some patients exposed to anesthetics[5]
We report a rare case of PBC after aortoiliac reconstruction using a Y-graft, suggesting that the graft itself or medications in the perioperative period might induce or exacerbate an autoimmune response, leading to bile duct injury. In the view of the risk to trigger onset of PBC, it becomes worthwhile to carefully evaluate past surgeries and medications carefully.
| 1. | Parikh-Patel A, Gold EB, Worman H, Krivy KE, Gershwin ME. Risk factors for primary biliary cirrhosis in a cohort of patients from the united states. Hepatology. 2001;33:16-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 170] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 2. | Roesler KW, Schmider W, Kist M, Batsford S, Schiltz E, Oelke M, Tuczek A, Dettenborn T, Behringer D, Kreisel W. Identification of beta-subunit of bacterial RNA-polymerase--a non-species-specific bacterial protein--as target of antibodies in primary biliary cirrhosis. Dig Dis Sci. 2003;48:561-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Poupon R, Poupon RE. Retrovirus infection as a trigger for primary biliary cirrhosis? Lancet. 2004;363:260-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Xu L, Shen Z, Guo L, Fodera B, Keogh A, Joplin R, O'Donnell B, Aitken J, Carman W, Neuberger J. Does a betaretrovirus infection trigger primary biliary cirrhosis? Proc Natl Acad Sci USA. 2003;100:8454-8459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 163] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 5. | Long SA, Van de Water J, Gershwin ME. Antimitochondrial antibodies in primary biliary cirrhosis: the role of xenobiotics. Autoimmun Rev. 2002;1:37-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Ohmori S, Itoh K, Kuniyoshi M, Shimizu A, Takase K, Nakano T, Tameda Y, Kosaka Y. An elder man's case of primary biliary cirrhosis with autoimmune hepatitis after the graft replacement of abdominal aortic aneurysma. Acta Hepatol Japonica. 1999;40:409-413. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
Science Editor Zhu LH and Guo SY Language Editor Elsevier HK