Published online Sep 7, 2005. doi: 10.3748/wjg.v11.i33.5239
Revised: December 18, 2004
Accepted: December 20, 2004
Published online: September 7, 2005
Cholangiocarcinoma is the second most common primary hepato-biliary malignancy. The majority of patients with primary hepatic tumors are not suitable candidates for resection, due to advanced stage of the disease at presentation, anatomic limitations and medical co-morbidities. At present, radiofrequency ablation (RFA) may offer an alternative, feasible and safe therapy for selected patients with hepatic tumors, who are not otherwise candidates for hepatic resection. Herein, we present the case of successful RFA in a patient with a solitary, primary intrahepatic cholangiocarcinoma. The patient remained free of disease 24 mo after the procedure, and is still followed up. This is the first report of RFA application in the treatment of primary intrahepatic cholangiocarcinoma.
- Citation: Zgodzinski W, Espat NJ. Radiofrequency ablation for incidentally identified primary intrahepatic cholangiocarcinoma. World J Gastroenterol 2005; 11(33): 5239-5240
- URL: https://www.wjgnet.com/1007-9327/full/v11/i33/5239.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i33.5239
Cholangiocarcinoma is a rare, malignant neoplasm arising from the biliary epithelium. The worldwide incidence of this malignancy is increasing and the annual incidence in USA is approximately 3 000-4 000 cases (0.85 per 100 000 rate)[1]. These cases are equally distributed between intrahepatic and extrahepatic lesions. The highest incidence rates of intrahepatic cholangiocarcinoma are noted in Northeast Thailand (96 per 100 000 for men and 38 per 100 000 for women). This variation in incidence is related to variations in the prevalence of risk factors. For example, in Thailand it is closely associated with liver fluke infestations[2]. The only potentially curative treatment for cholangiocarcinoma is surgical resection, but resectability of these tumors is determined by several factors including stage of the disease, anatomic conditions and patient’s medical co-morbidities.
At present, RFA in selected cases of intrahepatic cholangiocarcinoma may be one alternative treatment approach, particularly for patients who are not candidates for major surgery. Herein, we present a case of successful RFA application in the patient with primary intrahepatic cholangiocarcinoma.
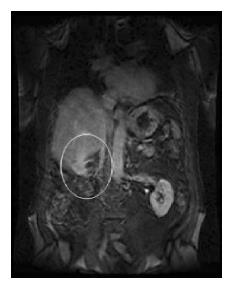
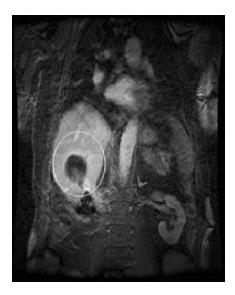
Subsequent to right upper abdominal discomfort, a 78-year-old man was found to have a solitary tumor in the right posterior hepatic lobe, by abdominal ultrasound examination. On physical examination, no significant findings were noted. Magnetic resonance scan confirmed the presence of an enhancing lesion located in segment VII, measuring approximately 4 cm×4 cm with enhancement on post-contrast images (Figure 1). No additional liver lesions or lymphadenopathy were identified. The patient’s history was remarkable for radical right nephrectomy and partial left (upper-pole) nephrectomy for bilateral renal cell carcinoma, one year prior to the presentation. Given the history and radiographic findings, the most likely diagnosis was considered to be that of metastatic renal cell carcinoma. While the lesion was amenable to resection by proper posterior sectorectomy (segments VI, VII), the patient suffered from morbid obesity with BMI = 36, insulin-dependent diabetes, hypertension, renal insufficiency (baseline creatinine 1.8 mg/dL); placing him at significant risk for morbidity from major surgery. Treatment options inclusive of laparoscopic-guided RFA were presented to the patient and subsequently the patient underwent diagnostic laparoscopy with intent to perform RFA. At operation, no evidence of extrahepatic disease was identified. The lesion was observed to encompass the inferior-most aspect of the segment VI/VII interface with significant post right nephrectomy adhesions. To prevent inadvertent thermal injury to the colon at the hepatic flexure, the procedure was converted to open using a lateral sub-costal mini-laparotomy incision. A core needle biopsy of the lesion was performed and sent for permanent pathology review. Using the RITA 7-0 XLi device, and saline infusion, the lesion was targeted by intraoperative ultrasound, and the RFA system was deployed and placed at a 1.0 cm forward-throw distance from the deepest tumor margin. The system was initiated as per the manufacturer’s instructions at 2 cm and subsequently advanced sequentially to 4-7 cm. The device needle was retracted in tract-ablation mode and the patient was awakened without complication. The post-operative period was uneventful and the patient was discharged at d 4 with post-operative follow-up imaging at 1 mo (Figure 2).
Unexpectedly, the tumor biopsy pathology revealed primary bile duct adenocarcinoma with strong immunoreactivity for Cytokeratin 7, Cytokeratin CAM 5.2 and CEA. The tumor cells were negative for Cytokeratin 20 and Vimentin. The patient remained free of detectable disease after 24 mo (Figure 3) with stable normal liver function tests.
We have presented a case of successful ablation of incidentally found primary intrahepatic cholangiocarcinoma using the RFA technique. RFA has become a common treatment for patients otherwise not candidates for resection either as potentially curative or within the context of consolidation therapy in the multi-disciplinary management of patients with primary hepatic malignancy in the liver (including hepatocellular carcinoma) and hepatic metastasis from colon and rectum, lungs, breast, and numerous other sites[3-5]. RFA can be performed during an open intraoperative procedure, laparoscopically or percutaneously under ultrasound guidance. The tumor is destroyed by generating heat within the lesion which results in coagulative necrosis of the neoplastic tissue. Once tissue is heated above 48-50 °C for 4 min, mitochondrial death ensues, cell membranes melt and fuse, and with continued heating, protein denaturation and irreversible cell death occurs. A typical treatment results in local tissue temperatures that exceed 100 °C. RFA has been reported to be relatively safe with acceptable rate of complications, when used by experienced surgeons. The combined overall early and late complication for this technique has been reported as 9.5% with higher risk in cirrhotic patients.
RFA has been previously reported as a salvage therapy for intrahepatic recurrent cholangiocarcinoma with a reported 10 mo survival after the procedure and ongoing follow-up. The present case report illustrates the potential expanding application of RFA technology in patients with primary cholangiocarcinoma, who are not otherwise surgical candidates. We emphasize that the selection criteria for RFA ablation should agree with the criteria used in selecting patients for potentially curative resection; i.e. tumor diagnosis that has demonstrated benefit from resection, no evidence of extrahepatic disease, capacity to encompass the entire lesion with a “margin”, and recognition that ablation results in hepatic parenchymal destruction which is equivalent to resection volume loss, thus the underlying Child’s status of the liver needs to be considered to prevent post-procedure hepatic failure. In the case presented, the diagnosis of cholangiocarcinoma was unknown and confirmed post procedure. The observed relatively long survival of this patient (24 mo) supports that, for selected patients, RFA may be a reasonable approach for effective therapy. However, until equivalence and/or survival data from appropriately designed clinical studies becomes available, the authors caution the judicious application of this technology.
| 1. | American cancer society. What are the key statistics for bile duct cancer?. Available from: www.cancer.org. |
| 2. | Shaib Y, El-Serag HB. The epidemiology of cholangiocarcinoma. Semin Liver Dis. 2004;24:115-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 839] [Cited by in RCA: 855] [Article Influence: 38.9] [Reference Citation Analysis (0)] |
| 3. | Curley SA, Izzo F, Delrio P, Ellis LM, Granchi J, Vallone P, Fiore F, Pignata S, Daniele B, Cremona F. Radiofrequency ablation of unresectable primary and metastatic hepatic malignancies: results in 123 patients. Ann Surg. 1999;230:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 886] [Cited by in RCA: 805] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 4. | Curley SA, Izzo F, Ellis LM, Nicolas Vauthey J, Vallone P. Radiofrequency ablation of hepatocellular cancer in 110 patients with cirrhosis. Ann Surg. 2000;232:381-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 574] [Cited by in RCA: 530] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 5. | Allgaier HP, Deibert P, Zuber I, Olschewski M, Blum HE. Percutaneous radiofrequency interstitial thermal ablation of small hepatocellular carcinoma. Lancet. 1999;353:1676-1677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 85] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
Science Editor Guo SY Language Editor Elsevier HK