Published online Aug 28, 2005. doi: 10.3748/wjg.v11.i32.5087
Revised: December 15, 2004
Accepted: December 20, 2004
Published online: August 28, 2005
Angiolipoma, a common benign tumor mostly seen in the subcutaneous tissue, is a rare pathological condition in the gastrointestinal tract that is usually diagnosed postoperatively. In this case report, an angiolipoma was diagnosed preoperatively by imaging (including CT scans, abdominal echo, barium enema, and colonoscopy). This pathology was confirmed postoperatively. Computed tomography scan, abdominal echo, and barium enema images were presented.
- Citation: Chen YY, Soon MS. Preoperative diagnosis of colonic angiolipoma: A case report. World J Gastroenterol 2005; 11(32): 5087-5089
- URL: https://www.wjgnet.com/1007-9327/full/v11/i32/5087.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i32.5087
Angiolipoma is a benign tumor, commonly occurring in the subcutaneous tissue and other locations, but is rarely found in the gastrointestinal tract. Histologically, it is comprised of adipose tissue and proliferative blood vessels. There have been three cases of colonic angiolipoma reported in the literature, which were all diagnosed postoperatively. This report presents the first preoperative diagnosis of colonic angiolipoma using a combination of colonoscopy, barium enema, abdominal echo, and CT scans. The diagnosis was confirmed postoperatively.
A 70-year-old male presented to Changhua Christian Hospital with a history of passing bloody stool once a day for 3 d. Additionally, the patient experienced abdominal distension and cramping pain for the past 7 d. Physical examination revealed mild anemia, abdominal obesity, no palpable mass, and hyperactive bowel sounds. Full blood count showed Hb of 10.7 and Hct of 31.5, but otherwise normal results. Colonoscopy found a submucosal tumor with ulceration of 5 cm located in the transverse colon obstructing the lumen almost completely. Contrast barium enema also revealed a 5-cm submucosal tumor located at the transverse colon with nearly complete obstruction of the lumen (Figure 1). Abdominal echo showed a centrally hyperechoic dense tumor surrounded by hypoechoic density (Figure 2). Pre-contrast enhancement CT scan showed a mixed low density and isodensity tumor (Figure 3). Post-contrast enhancement scans showed a high-density tumor with a fat component (Figure 4).
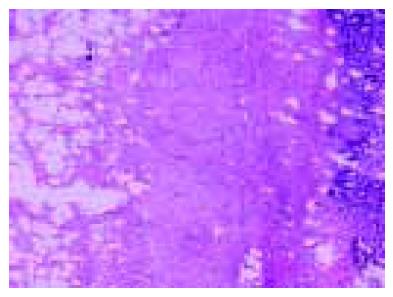
Based on the combined findings, it was diagnosed as an angiolipoma and surgical segmental resection was carried out. The resected tumor was encapsulated by a thin layer of connective tissue arising from the submucosa. Histology showed that the tumor was comprised of mature adipose tissue and proliferative blood vessels (Figure 5). After 2 years of follow-up, the patient did not have any abnormalities.
Angiolipoma was first described in 1912 by Bowen. In 1960, Howard and Helwig described its clinical pathological characteristics, which are different from those of lipoma[1]. Since then, angiolipoma has been regarded as a new entity. Angiolipoma is an encapsulated, subcutaneous tumor commonly occurring in young adults. It usually occurs in multiple locations on both the arms and trunk[2,3]. Angiolipoma is usually painful. Histologically it is comprised of mature adipose tissue and proliferative vascular tissues. It can be classified as predominantly lipomatous- or angiomatous-type, based on the ratio of adipose tissue and vascular tissue composition.
A search of the current literature revealed only seven cases of angiolipoma in the gastrointestinal tract. Of these, three cases had angiolipoma in the stomach[4-6]. One angiolipoma was in the small intestine[7] and three were reported to be in the colon[8-10]. Two of the colonic angiolipomas were located at the ileocecal valve. One case had intussusception originally thought to be due to malignant tumor. Thus, the author emphasizes using histological pathology to diagnose this condition[8]. In another case, the patient had right lower quadrant abdomen. Laparoscopy-assisted ileocecostomy is selected to remove the tumor[9]. In the third case, the patient was asymptomatic, but had positive occult blood on routine medical examination. Double-contrast barium enema showed angiolipoma in the sigmoid colon, which was resected by colonoscopic polypectomy. The patient in this case report had lower gastrointestinal tract bleeding. Preoperative imaging allowed the diagnosis of angiolipoma, which was removed by segmentectomy.
None of the seven patients with gastrointestinal tract angiolipoma had preoperative abdominal echogram. Because the composition of angiolipoma can range from predominantly lipomatous to angiomatous type, echogram can vary from hyperechoic to hypoechoic density. In 1998, Mintz and Mengoni[11] used sonography to diagnose breast angiolipoma, which showed homogenously hyperechoic density under echogram. In this case report, the tumor was between the two types of angiolipoma, showing hyperechoic density centrally and hypoechoic density peripherally.
Computed tomography scan pattern depends on the composition of fat in the tumor. It can vary from a lipomatous type of tumor comprised totally of fat without post-contrast enhancement, which was thought to be lipoma preoperatively[12], to a low-fat containing tumor, showing numerous small round density enhancements[13,14]. In this case, diffuse high-density enhancement post-contrast was observed around the adipose tissue, which is consistent with the histological pattern.
In our case, contrast barium enema confirmed the submucosal tumor. Sonography showed hyperechoic density surrounded by hypoechoic density, and CT showed post-contrast fat containing mass, surrounded by high-density enhancement. The combination of these results allowed the tumor to be differentiated from lipoma, thus it could be diagnosed as an angiolipoma preoperatively.
Although management of colonic lipoma or angiolipoma is still controversial, endoscopic resection should not be used on sessile or broad-based lesions because of increased risk of bleeding or perforation. Urgent treatment should be given to those with intussusception, obstruction, or bleeding, as in this case. The tumor should then be removed, while the patient is still in the hospital. However, both lipoma and angiolipoma are benign tumors, thus colonic resection should be kept to a minimum when the tumor is removed[9,10]. In this case, a small segmental resection was performed.
| 1. | Howard WR, Helwig EB. Angiolipoma. Arch Dermatol. 1960;82:924-931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 240] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 2. | Ackermano LV, Rosai J. Tumors of adipose tissue. 8th ed Vol 12. St Louis: Mosby 1996; 2053-2060. |
| 3. | Enzinger FM, Weiss SW. Soft tissue tumors 3rd ed. Benign lipomatous tumors, St. Louis Mosby. St Louis: Mosby 1995; 390. |
| 4. | DeRidder PH, Levine AJ, Katta JJ, Catto JA. Angiolipoma of the stomach as a cause of chronic upper gastrointestinal bleeding. Surg Endosc. 1989;3:106-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | McGregor DH, Kerley SW, McGregor MS. Case report: gastric angiolipoma with chronic hemorrhage and severe anemia. Am J Med Sci. 1993;305:229-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Hunt J, Tindal D. Solitary gastric Peutz-Jeghers polyp and angiolipoma presenting as acute haemorrhage. Aust N Z J Surg. 1996;66:713-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Kaneko T, Karasawa Y, Inada H, Tamura Y, Yamamura N, Iijima Y, Nagata A, Oohata T, Shirota H, Nakamura T. An adult case of intussusception due to inverted Meckel's diverticulum accompanied by angiolipoma. Nihon Shokakibyo Gakkai Zasshi. 1996;93:260-265. [PubMed] |
| 8. | Saroglia G, Coverlizza S, Roatta L, Leli R, Fontana D. Angiolipoma of the cecum. Minerva Chir. 1996;51:59-62. [PubMed] |
| 9. | Kato K, Matsuda M, Onodera K, Sakata H, Kobayashi T, Kasai S. Angiolipoma of the colon with right lower quadrant abdominal pain. Dig Surg. 1999;16:441-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Okuyama T, Yoshida M, Watanabe M, Kinoshita Y, Harada Y. Angiolipoma of the colon diagnosed after endoscopic resection. Gastrointest Endosc. 2002;55:748-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Mintz AD, Mengoni P. Angiolipoma of the breast: sonographic appearance of two cases. J Ultrasound Med. 1998;17:67-69. [PubMed] |
| 12. | Ferrozzi F, Tognini G, Bova D, Pavone P. Lipomatous tumors of the stomach: CT findings and differential diagnosis. J Comput Assist Tomogr. 2002;24:854-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Biondetti PR, Fiore D, Perin B, Ravasini R. Infiltrative angiolipoma of the thoracoabdominal wall. J Comput Assist Tomogr. 1982;6:847. [PubMed] |
| 14. | Pfeil SA, Weaver MG, Abdul-Karim FW, Yang P. Colonic lipomas: outcome of endoscopic removal. Gastrointest Endosc. 1990;36:435-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 71] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
Science Editor Wang XL and Guo SY Language Editor Elsevier HK