INTRODUCTION
Choledochal cyst is characterized by a balloon-like dilatation of the extrahepatic duct, occasionally associated with dilatation of the intrahepatic ducts. Ultrasonography (US) remains the primary imaging modality for the evaluation of the fetus and can suggest the diagnosis of choledochal cyst, when a tubular structure is identified at the right upper quadrant abdomen[1-4]. Magnetic resonance imaging (MRI) has evolved and has become an important complement to US, for more accurate and precise delineation and characterization of fetal anomalies. With recently developed ultrafast MR sequences such as half-Fourier, single-shot, turbo spin-echo (HASTE), a single slice can be obtained in less than 400 ms[5]. Many studies have shown the usefulness of these ultrafast MR scans in evaluating the fetus[6-8]. Here, we report a case of choledochal cyst prenatally diagnosed by using US and MRI and confirmed by postnatal surgery and histopathology.
CASE REPORT
A 29-year-old woman, gravida 2, para 1, presented at our hospital at 24th wk’ gestation for prenatal US surveillance. Fetal US showed an ovoid cystic lesion measuring 2.1 cm× 1.1 cm×1.2 cm at the right upper quadrant abdomen. A choledochal cyst or an enteric cyst was impressed.
Two weeks later, a fetal MRI (Philips 1.5 T Intera; Erlangen, Germany) was performed to further evaluate the cyst using HASTE sequence (TR 10 ms; TE 100 ms; time of acquisition 12 s; flip angle 90o; field of view 280 mm×250 mm; matrix 256×256). MRI showed a 1.3 cm× 1.2 cm×2.7 cm, ellipsoid, homogeneous cystic lesion extending from the liver hilum posteriorly and inferomedially to the mid-abdomen (Figure 1). This lesion showed hypointensity on T1-weighed and hyperintensity on T2-weighed images. A more detailed anatomical relationship of the cyst to the gall bladder and the biliary tracts was shown. Type 1 choledochal cyst was tentatively diagnosed.
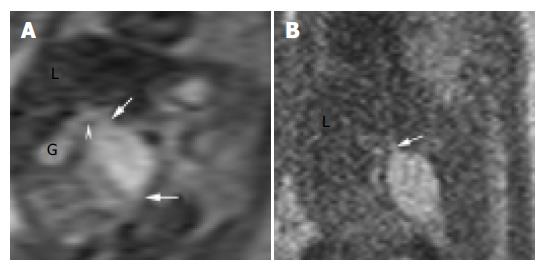
Figure 1 MRI performed at 26 wk’ gestation using HASTE sequence.
A: Coronal T2-weighed image showed the choledochal cyst, its tapered ends (arrows), its connection to the cystic duct (arrowhead), and its relationship to the gall bladder (G) and the liver (L); B: Sagittal T2-weighed image showed the posterio-inferior orientation of the choledochal cyst and its connection to the common hepatic duct (arrow).
A female infant weighing 3 890 g was delivered at 39 wk with APGAR scores of 8 and 10 at 1 and 5 min, respectively. Postnatal US at 3 d of age showed further enlargement of the cyst. At 13 d of age, the cyst was excised and a Roux-en-Y hepatico-jejunostomy was performed. Histopathological examination confirmed the diagnosis of a choledochal cyst. The infant was discharged a week later with no jaundice noted thereafter.
DISCUSSION
Choledochal cysts are rare anomalies, characterized by cystic or fusiform dilatation of the intrahepatic and/or extrahepatic biliary tracts. These cysts have been classified into five major types[9]. Cystic dilatation of the common bile duct (type 1 choledochal cyst) comprises 80-90% of the cysts. In affected newborns, about 70% had jaundice but only 25% had a palpable abdominal mass[4]. Potential complications in untreated patients include recurrent cholangitis, pancreatitis, liver cirrhosis, portal hypertension, and malignant transformation[10-12].
Ultrasonography is the primary imaging modality for evaluating the fetus due to its real-time display and non-invasiveness. In cases of choledochal cyst, tubular structures can be identified entering or leaving a right upper quadrant cyst[1,2,4]. However, the choledochal cyst could be missed, if confused with the gall bladder and the umbilical vein. Other common cystic lesions, including hydronephrosis, duodenal duplication, intestinal atresia, mesenteric cyst, and ovarian cyst, may appear similar to a choledochal cyst.
Recent development of ultrafast MR imaging techniques has allowed MRI to become an important complement to US in fetal imaging[5-8]. MRI offers superior soft tissue contrast, larger field of view, and is relatively operator independent. In our case, while the prenatal US showed a subhepatic cyst, the MRI showed additional findings of tapered ends of the cyst, its proximity to the liver hilum, its inferomedial orientation, and characteristic fluid-intensity of the cyst. Also, the relationship between the choledochal cyst, the cystic duct and the dilated gall bladder was clearly depicted. Concerning the differential diagnoses of a right upper quadrant cyst, an umbilical vein may be excluded by the lack of vascular flow void on MRI. Other common cystic lesions, including hydronephrosis, intestinal atresia, mesenteric cyst, and ovarian cyst have locations different from that of a choledochal cyst. Duodenal duplication may not be easily excluded, but it would be less likely to have tapered ends as a choledochal cyst[13]. To our best knowledge, we found two reports of prenatal MRI investigation of choledochal cysts[14,15]. However, the finding of tapered ends of the choledochal cyst, which may be specific to a biliary tract anomaly, was not emphasized in their reports.
In conclusion, owing to its excellent anatomical and contrast resolutions, MRI can clearly delineate a choledochal cyst and may be helpful in differential diagnosis of right upper quadrant cystic lesions. The additional information provided by prenatal MRI, which is complementary to US, may be valuable for family counseling, and may help clinicians manage pregnancy and plan post-natal treatment earlier.