Published online Aug 14, 2005. doi: 10.3748/wjg.v11.i30.4766
Revised: July 20, 2004
Accepted: July 22, 2004
Published online: August 14, 2005
Acute pancreatitis as an initial symptom of systemic lupus erythematosus (SLE) is rare. We present a report of a 46-year-old female patient who had fever, abdominal pain and vomiting, elevated pancreatic enzyme levels, hypocalcemia, hypoxemia, and various other laboratory abnormalities. She was first diagnosed with acute severe pancreatitis and then with SLE after further investigations. After a 2-mo treatment with somatostatin, the patient recovered.
- Citation: Wang F, Wang NS, Zhao BH, Tang LQ. Acute pancreatitis as an initial symptom of systemic lupus erythematosus: A case report and review of the literature. World J Gastroenterol 2005; 11(30): 4766-4768
- URL: https://www.wjgnet.com/1007-9327/full/v11/i30/4766.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i30.4766
Systemic lupus erythematosus (SLE) is a multi-system, autoimmune disorder characterized by a broad range of manifestations, including presence of antibodies against cell nuclei. The initial manifestations of SLE, however, can involve many organ systems either singly or in combination, which frequently makes diagnosis difficult. The American Rheumatism Association recommends that the diagnosis of SLE can be confirmed if it meets 4 of the following 11 revised criteria: malar rash, discoid rash, photo-sensitivity, oral ulcers, arthritis, serositis, renal disorder, neurologic disorder, hematologic disorder, immunologic disorder, and antinuclear antibodies.
We report a 46-year-old female patient with fever, abdominal pain and vomiting, elevated levels of pancreatic enzyme, hypocalcemia, hypoxemia, and other laboratory abnormalities. She was first diagnosed with acute severe pancreatitis and then with SLE, after further investigations.
A 46-year-old woman came to the Sixth Hospital attached to Shanghai Jiaotong University, complaining of a 6-d history of persistent abdominal pain, loss of appetite, occasional nausea and vomiting without obvious reasons. She also had a 3-d history of fever and generalized weakness.
She reported bilateral thigh pain, finger pain and swelling 5 mo ago, which were abated after 7-d treatment with hydroxy-chloroquine. Four months ago, she had elevated alanine aminotransferase, and received no treatment. She also reported some thinning of her hair and a weight loss of 5 kg in the past 2 mo. Her family history was unremarkable for auto-immune disorders.
Her body temperature was 38°C, pulse rate 100 beats per minute, blood pressure 120/80 mmHg. She had no skin lesions, but had swollen and painless lymph nodes. She had fine rales on bilateral lungs, and 3-degree systolic murmur in the mitral valve area and a pericardial friction sound. Her abdomen was soft with mild epigastric tenderness, minimal guarding, and no rebound tenderness.
Her blood chemistry was as follows: 126 mmol/L sodium, 4.4 mmol/L potassium, 97 mmol/L chloride, 22.5 mmol/L bicarbonate, 1.6 mmol/L blood urea nitrogen, 31 µmol/L creatinine, 5.1 mmol/L glucose, 83 U/L aspartate aminotr-ansferase, 16 U/L alanine aminotransferase, 66 g/L protein, 37 g/L albumin, 1.70 mmol/L calcium, and 18 mol/L total bilirubin. A complete blood count showed a white cell count of 3.0×109/L with 78.9% neutrophils, 19.8% lymphocytes, 2.3% monocytes. Hemoglobin was 89 g/L, hematocrit 33.8%, and platelets 112×109/L. Pancreatic enzyme determinations disclosed a blood amylase level of 1 000 U/L (normal 20-115 U/L) and urine amylase level of 830 U/L, and a lipase level of 690 U/L. Urinalysis showed cloudy urine with a protein level of 260 mg/dL, a white cell count of 3-4/µL, granular casts 0. Nitrite and leukocyte esterase were negative. Blood culture was negative.
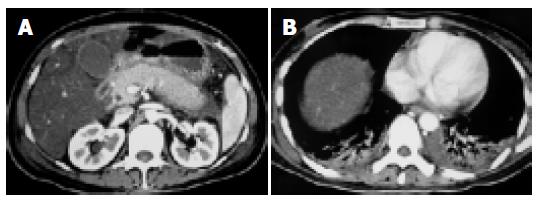
Computed tomographic (CT) scan and ultrasonic scan of the abdomen with contrast, showed swollen pancreas but no gallbladder stones (Figure 1A). Another CT scan of the bosom showed effusion both in right and in left pleurae (Figure 1B).
Connective tissue showed an antinuclear antibody (ANA) titer of 1:640, positive anti-double-stranded DNA (dsDNA) antibody, negative anti-Smith antibody, anti-ribonucleoprotein, anti-SSA, and anti-SSB. The erythrocyte sedimentation rate was 92, complement 3 (C3) was 0.75 g/L (normal 1.0-1.8 g/L), anti-cardiolipin antibodies and lupus anti-coagulant were negative.
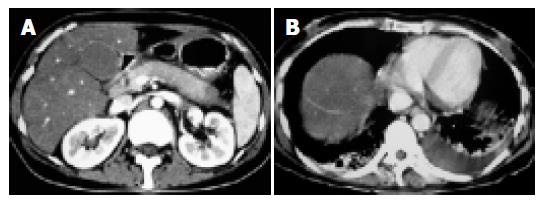
After a 2-mo treatment with somatostatin, the pancreatic enzyme was 29 U/L. Repeated CT scan revealed a less swollen pancreas (Figure 2A) and still bilateral pleural effusion (Figure 2B). But the patient still had fever and palpitation. A diagnosis of SLE pancreatitis was made on the 66th d of admission, and 40 mg methylprednisolone intravenous injection qd was started. Once steroid therapy began, the heart rate declined to 90 beats per minute. Two weeks after continuous steroid therapy, the heart rate was 78 beats per minute and the temperature was 36.6°C. Pleural effusion disappeared.
Although the patient on admission was positive for ANA and anti-dsDNA, arthritic, serositic and blood cells reduced, which fulfills the American Rheumatism Association criteria for the diagnosis of SLE. Our case illustrates the protean manifestations of SLE and a rare initial manifestation as acute pancreatitis. Over 50% SLE patients have manifestations of digestive system, but pancreatitis is few, and such acute pancreatitis as an initial manifestation is even rare. The association between SLE and pancreatitis was first documented in 1939[1]. Since then, only 70 cases of SLE pancreatitis have been documented in the literature, and only 10 of these cases, including this one, have pancreatitis as their initial manifestation[2-5].
The mechanisms involved in the origin of SLE pancreatitis are not clear. SLE pancreatitis might result from vasculitis, microthrombi, anti-pancreas autoantibody, side-effects of medicine, intimal thickening and virus infection. Most lupus pancreatitis is found in patients with long-standing SLE who have multi-organ involvement and are already on steroid, diuretic, or immunosuppressive therapy, all of which have been implicated in the etiology of pancreatitis. Since the initial description of SLE pancreatitis, whether steroid or SLE is the primary cause has been controversial. Recent studies support that SLE is the primary etiologic factor of SLE pancreatitis, and drug toxicity may also play a role[5-9].
Pathological changes of SLE pancreatitis bear similarities to those of pancreatitis due to other causes. SLE pancreatitis can occur during a generalized flare-ups and disease quiescence, though the latter seems more likely[3]. Its manifestation can be acute, severe, or chronic, self-limiting or fulminant. It is believed that subclinical pancreatitis which has an elevation of pancreatic enzymes without clinical symptoms is much more frequent than symptomatic pancreatitis[10-14]. About 30.5% of asymptomatic SLE patients have hyperamylasemia; therefore subclinical pancreatic damage might occur very frequently in SLE[15].
Within the context of SLE, the diagnosis of SLE pancreatitis is usually based on clinical findings as abdominal pain, nausea, and vomiting as well as laboratory findings like abnormal pancreatic enzymes and suggestive tomographic findings. Etiology diagnosis is fairly important, which decides whether steroid can be used. If drug toxicity is not considered as the origin, SLE pancreatitis is treated with steroid. Of course, steroid or other drugs should be stopped once they are regarded as the cause[16,17].
In conclusions, it is important to determine whether drug toxicity is the cause of SLE pancreatitis. If the condition of patients with SLE pancreatitis can be improved with somatostatin, steroid might not be necessary during the acute episode.
| 1. | Jaspersen D. [Gastrointestinal manifestations of systemic lupus erythematosus: symptoms, diagnosis and differential diagnosis]. Fortschr Med. 1992;110:167-169. [PubMed] |
| 2. | Penalva JC, Martínez J, Pascual E, Palanca VM, Lluis F, Peiró F, Pérez H, Pérez-Mateo M. Chronic pancreatitis associated with systemic lupus erythematosus in a young girl. Pancreas. 2003;27:275-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Duncan HV, Achara G. A rare initial manifestation of systemic lupus erythematosus--acute pancreatitis: case report and review of the literature. J Am Board Fam Pract. 2003;16:334-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Swol-Ben J, Bruns CJ, Müller-Ladner U, Hofstädter F, Link J, Hechenrieder C, Jauch KW. Leukoencephalopathy and chronic pancreatitis as concomitant manifestations of systemic lupus erythematosus related to anticardiolipin antibodies. Rheumatol Int. 2004;24:177-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Lê Thi Huong D, Papo T, Laraki R, Wechsler B, Blétry O, Chapelon C, Cabane J, Godeau P. Pancreatitis in systemic lupus erythematosus. Review of the literature apropos of 5 cases. Rev Med Interne. 1994;15:89-94. [PubMed] |
| 6. | Yeh TS, Wang CR, Lee YT, Chuang CY, Chen CY. Acute pancreatitis related to anticardiolipin antibodies in lupus patients visiting an emergency department. Am J Emerg Med. 1993;11:230-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Kolk A, Horneff G, Wilgenbus KK, Wahn V, Gerharz CD. Acute lethal necrotising pancreatitis in childhood systemic lupus erythematosus--possible toxicity of immunosuppressive therapy. Clin Exp Rheumatol. 1995;13:399-403. [PubMed] |
| 8. | Saab S, Corr MP, Weisman MH. Corticosteroids and systemic lupus erythematosus pancreatitis: a case series. J Rheumatol. 1998;25:801-806. [PubMed] |
| 9. | Ikura Y, Matsuo T, Ogami M, Yamazaki S, Okamura M, Yoshikawa J, Ueda M. Cytomegalovirus associated pancreatitis in a patient with systemic lupus erythematosus. J Rheumatol. 2000;27:2715-2717. [PubMed] |
| 10. | Al-Mayouf SM, Majeed M, Al-Mehaidib A, Alsuhaibani H. Pancreatic pseudocyst in paediatric systemic lupus erythematosus. Clin Rheumatol. 2002;21:264-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Singh R, Saunders B, Scopelitis E. Pancreatitis leading to thrombotic thrombocytopenic purpura in systemic lupus erythematosus: a case report and review of literature. Lupus. 2003;12:136-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Langlet P, Karmali R, Deprez C, Brandelet B, Kleynen P, Dratwa M, de Koster E, Denis P, Deltenre M. Severe acute pancreatitis associated with peliosis hepatis in a patient with systemic lupus erythematosus. Acta Gastroenterol Belg. 2001;64:298-300. [PubMed] |
| 13. | Singh M, Wani S, Murtaza M, Joglekar S, Kasubhai M. Systemic lupus erythematosus presenting with acute fatal pancreatitis as an initial manifestation. Am J Gastroenterol. 2001;96:2280-2281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Marum S, Veiga MZ, Silva F, Vasconcelos T, Ferreira A, Viegas J. Lupus pancreatitis. Acta Med Port. 1998;11:779-782. [PubMed] |
| 15. | Ranson JH. Diagnostic standards for acute pancreatitis. World J Surg. 1997;21:136-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 55] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Frank B, Gottlieb K. Amylase normal, lipase elevated: is it pancreatitis? A case series and review of the literature. Am J Gastroenterol. 1999;94:463-469. [PubMed] |
| 17. | Eaker EY, Toskes PP. Systemic lupus erythematosus presenting initially with acute pancreatitis and a review of the literature. Am J Med Sci. 1989;297:38-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
Science Editor Wang XL Language Editor Elsevier HK