Published online Jul 21, 2005. doi: 10.3748/wjg.v11.i27.4287
Revised: November 23, 2004
Accepted: November 26, 2004
Published online: July 21, 2005
Ciliated hepatic foregut cyst (CHFC) is a very rare cystic lesion of the liver that is histologically similar to bronchogenic cyst. We report one case of CHFC that was hard to distinguish from solid-cystic neoplasm in imaging features. Magnetic resonance imaging was helpful in differentiating these cysts from other lesions.
- Citation: Fang SH, Dong DJ, Zhang SZ. Imaging features of ciliated hepatic foregut cyst. World J Gastroenterol 2005; 11(27): 4287-4289
- URL: https://www.wjgnet.com/1007-9327/full/v11/i27/4287.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i27.4287
Ciliated hepatic foregut cyst (CHFC) is a very rare, benign and solitary cyst[1,2]. It is most often unilocular[2]. To our knowledge, 5 cases of CHFC were reported in the 19th century, 53 cases in the 20th century and 5 cases in the 21st and its medical imaging findings are seldom reported[1,3]. It is difficult to differentiate the CHFC from malignant tumor[1,4,5]. Herein, we present the radiologic features from one CHFC that was not similar to other nonparasitic cysts, but rather mimicked cystic-solid mass of the liver on the images obtained.
A 30-year-old man presented with a 5-mo history of left upper abdominal discomfort and mild fatigue. Physical examination and laboratory studies had no positive findings including hepatitis.
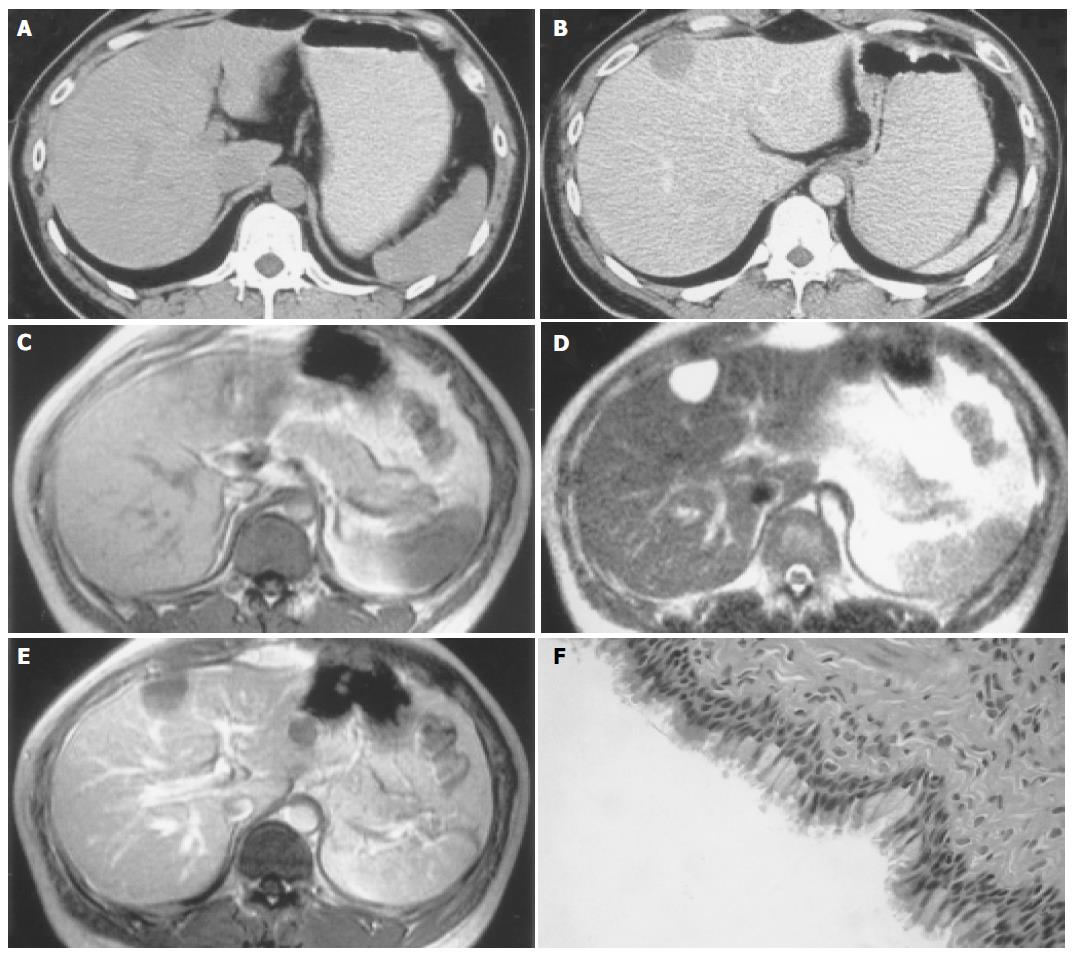
A plain radiograph of the abdomen was normal. Sonographic examination revealed a well-delineated hypoechoic mass, 3 cm × 4 cm in size, in the liver. It was located in the medial segment of the left lobe (segment IV), just adjacent to the surface of the liver. Unenhanced computed tomographic (CT) scan was obtained, and the lesion appeared slightly hypoattenuating relative to surrounding liver parenchyma (Figure 1A). The attenuation value of the lesion was 47 HU. At contrast material-enhanced CT, this lesion was not enhanced and appeared slightly hypoattenuating with well-defined margin (Figure 1B). On delayed CT scan, it had still no enhancement. Magnetic resonance (MR) imaging at 1.5 T was performed for more detailed examination. The lesion appeared isointense relative to surrounding liver parenchyma on T1-weighted imaging (Figure 1C) and markedly homogeneously hyperintense on T2-weighted imaging (Figure 1D). It was also not enhanced after Gd-DTPA administration (Figure 1E).
The lesion was resected surgically because the possibility of hypovascular neoplasm could not be excluded completely according to the imaging. The resected specimen revealed an unilocular cystic lesion containing a mucinous fluid.
On pathologic examination, the cyst had a fibrous wall lined by ciliated pseudostratified columnar epithelial cells, which was consistent with a CHFC (Figure 1F).
The histogenesis of CHFC is still unclear, but most authors consider that it arises from the embryonic foregut in the liver[1,2,5]. CHFC is usually a benign, solitary cyst consisting of a ciliated pseudostratified columnar epithelium, a subepithelial connective tissue layer, a smooth muscle layer and an outer fibrous capsule[2,6]. It is often smaller than 3 cm in diameter and found most commonly in the medial segment of the left hepatic lobe, just beneath the hepatic surface[5,7]. CHFC is not actually a neoplasm and usually found incidentally on radiologic imaging during surgical exploration or autopsy. It is mostly asymptomatic and surgical resection should be avoided[5]. However, on the other hand, it was reported recently that one case causes portal vein compression and the other shows malignant transformation through squamous metaplasia (it is not surprising to find squamous mucosa because tracheobronchial tree derives from the embryologic foregut), which warns to examine CHFC cautiously[8,9], and suggests that a large-sized symptomatic CHFC should be excised, especially when radiologic studies yield equivocal results[10].
Generally CHFC is a well-delineated anechoic or slightly hypoechoic small mass on ultrasonography. Because CHFC can contain various elements ranging from clear serous material to milky white to brown mucoid material, and these have variable viscosities, and the different CT attenuation numbers can be shown[5]. The lesion can be hypoattenuating as our case or isoattenuating relative to surrounding liver parenchyma at unenhanced CT. Even it has very high attenuation numbers because the lesion contains calcium[5]. All the CHFCs have no enhancement after injection of contrast materials, which is one of the characteristics of CHFC and has significance in the differential diagnosis. On MR imaging, all lesions are hyperintense on T2-weighted sequences. However, on T1-weighted images, they may be hypointense, isointense, or hyperintense according to the various elements the lesions contain, including clear serous material or milky white or brown mucous with abundant protein and lipid sometimes[5,11,12].
When a CHFC appears hypoechoic at US and the attenuation at CT ranges from that of soft tissue to very high attenuation, it is hard to differentiate the CHFC from a solid lesion. However, MR imaging is found to be useful in differential diagnosis, especially on T2-weighted imaging. When a CHFC is demonstrated as anechoic lesion at US, cystadenoma may be included in the differential diagnosis because the lesion may be malignant. Differential points are that cystadenomas are usually multilocular and sometimes reveal mural nodules, and these features are well revealed on radiologic imaging[5].
CHFC occurs more frequently in men and is found most commonly in the medial segment of the left hepatic lobe just beneath the hepatic surface, unlike most other solitary cysts that show a female predominance and greater occurrence in the right hepatic lobe[7]. Therefore, this location is also one of the characteristics of CHFC and probably an important diagnostic consideration. Meanwhile, MRI is helpful to differentiate CHFC from other solitary cysts that usually show markedly homogeneously hypointense on T1-weighted imaging.
In conclusion, when a well-demarcated subcapsular lesion of the left hepatic lobe with the varied internal appearance as we described above is demonstrated, CHFC should be considered.
| 1. | Horii T, Ohta M, Mori T, Sakai M, Hori N, Yamaguchi K, Fujino H, Oishi T, Inada Y, Nakamura K. Ciliated hepatic foregut cyst. A report of one case and a review of the literature. Hepatol Res. 2003;26:243-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Bogner B, Hegedûs G. Ciliated hepatic foregut cyst. Pathol Oncol Res. 2002;8:278-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Hirata M, Ishida H, Konno K, Nishiura S. Ciliated hepatic foregut cyst: case report with an emphasis on US findings. Abdom Imaging. 2001;26:594-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Wu ML, Abecassis MM, Rao MS. Ciliated hepatic foregut cyst mimicking neoplasm. Am J Gastroenterol. 1998;93:2212-2214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Kadoya M, Matsui O, Nakanuma Y, Yoshikawa J, Arai K, Takashima T, Amano M, Kimura M. Ciliated hepatic foregut cyst: radiologic features. Radiology. 1990;175:475-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 48] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Rosai J. Liver. Ackerman's surgical pathology. 8th ed. St Louis: Mosby 1996; 898-899. |
| 7. | Vick DJ, Goodman ZD, Deavers MT, Cain J, Ishak KG. Ciliated hepatic foregut cyst: a study of six cases and review of the literature. Am J Surg Pathol. 1999;23:671-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 62] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Harty MP, Hebra A, Ruchelli ED, Schnaufer L. Ciliated hepatic foregut cyst causing portal hypertension in an adolescent. AJR Am J Roentgenol. 1998;170:688-690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Furlanetto A, Dei Tos AP. Squamous cell carcinoma arising in a ciliated hepatic foregut cyst. Virchows Arch. 2002;441:296-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 63] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | de Lajarte-Thirouard AS, Rioux-Leclercq N, Boudjema K, Gandon Y, Ramée MP, Turlin B. Squamous cell carcinoma arising in a hepatic forgut cyst. Pathol Res Pract. 2002;198:697-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Murakami T, Imai A, Nakamura H, Tsuda K, Kanai T, Wakasa K. Ciliated foregut cyst in cirrhotic liver. J Gastroenterol. 1996;31:446-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Shoenut JP, Semelka RC, Levi C, Greenberg H. Ciliated hepatic foregut cysts: US, CT, and contrast-enhanced MR imaging. Abdom Imaging. 1994;19:150-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
Science Editor Wang XL and Guo SY Language Editor Elsevier HK