Published online May 7, 2005. doi: 10.3748/wjg.v11.i17.2684
Revised: March 14, 2004
Accepted: April 13, 2004
Published online: May 7, 2005
AIM: To assess the effectiveness of and complications associated with polyvinyl alcohol (PVA) and gelatin sponge particles embolization of splenic artery pseudoaneurysm complicating chronic alcoholic pancreatitis.
METHODS: A 42-year-old man with splenic artery pseudo-aneurysm formation secondary to chronic alcoholic pancreatitis was admitted. We used PVA and gelatin sponge particles embolization of splenic artery pseudoaneurysm by superselective embolization techniques.
RESULTS: The splenic artery pseudoaneurysm was successfully controlled with splenic embolization. The patient was discharged in 9 d with complete recovery.
CONCLUSION: This case confirms that superselective transcatheter embolization by PVA and gelatin sponge particles may represent an effective treatment for pseudoaneurysm caused by chronic alcoholic pancreatitis in the absence of other therapeutic alternatives.
- Citation: Guan YS, Sun L, Zhou XP, Li X, Fei ZJ, Zheng XH, He Q. Polyvinyl alcohol and gelatin sponge particle embolization of splenic artery pseudoaneurysm complicating chronic alcoholic pancreatitis. World J Gastroenterol 2005; 11(17): 2684-2686
- URL: https://www.wjgnet.com/1007-9327/full/v11/i17/2684.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i17.2684
Chronic pancreatitis is known to cause vascular complications including pseudoaneurysm of peripancreatic arteries. Splenic artery pseudoaneurysms are the most common of visceral artery pseudoaneurysms[1]. Splenic pseudoaneurysms appear to develop as a consequence of inflammatory processes adjacent to splenic artery, particularly acute and chronic pancreatitis with associated pseudocysts. They are often asymptomatic and picked up on abdominal examination during ultrasound or CT scan for other conditions. Complications include rupture with retroperitoneal or intraperitoneal hemorrhage[2,3]. The initial imaging work-up included sonography, angiography and helical computed tomography with multiplanar and 3D reformations. This enabled comprehensive evaluation of the pseudo-aneurysm and associated pathology in the majority of cases. Bleeding splanchnic artery pseudo-aneurysm is a rare but frequently fatal complication that can be successfully managed by angiographic embolization. However, certain patients because of hemodynamic instability, non-availability of technique or angiographic failure may require primary surgical intervention[4,5]. We report a 42-year-old man with splenic artery pseudo-aneurysm formation secondary to chronic alcoholic pancreatitis. The splenic artery pseudoaneurysm was successfully controlled by superselective polyvinyl alcohol (PVA) and gelatin sponge particle embolization without splenic preservation.
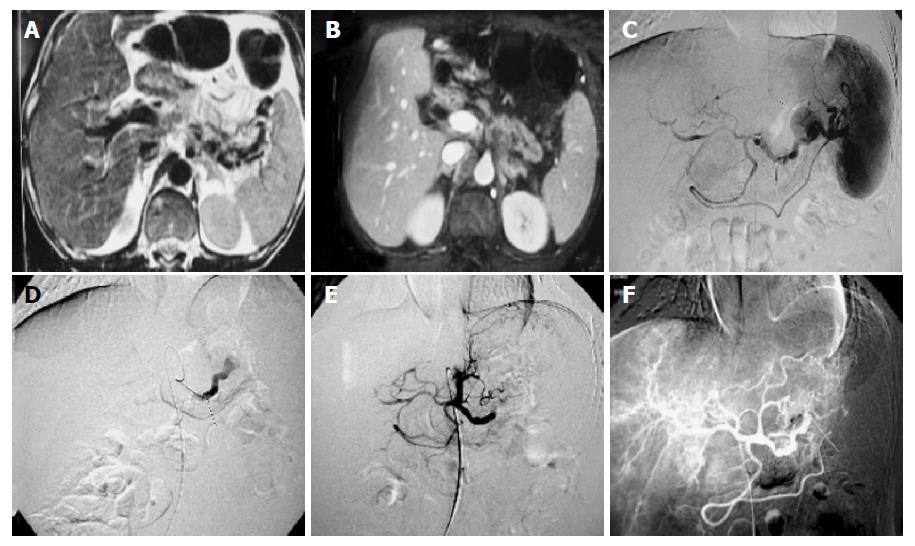
A 42-year-old male was admitted with a 2-year history of chronic alcoholic pancreatitis, unusual type diabetes mellitus, vitiligo, and weight loss. Abdominal MRI scans 5-mo ago showed chronic pancreatitis and varicosis of the hilum of spleen vein (Figure 1A). Abdominal CT scan suggested a pseudoaneurysm at the body of pancreas (Figure 1B). A celiac trunk arteriogram revealed a pseudoaneurysmal sac originating from the splenic artery (Figure 1C). The patient refused to receive splenectomy and distal pancreatectomy, and he was also a surgically high-risk patient because of unusual type diabetes mellitus.
To obliterate the pseudoaneurysm, the first transcatheter embolization with steel coils was attempted, but failed. Splenic artery was twisted severely and the tunica intima of vessel was uneven. The second transcatheter embolization was performed by more experienced interventional radiologists 14 d later. We chose 5-F RH and 3-F SP catheters (Cook) to realize superselective intubation. PVA (250-355 μm, 2 Rami) and microgelatin (d = 1 mm, 150 Granulation) were used to embolize splenic artery pseudoaneurysm and distal splenic artery through the 3-F SP catheter (Figure 1D). After embolization procedures were completed, angiography of splenic artery showed the pseudoaneurysm has disappeared (Figures 1E-1F). The patient recovered and was discharged from the hospital 9 d later. He had no subsequent bleeding episodes and was doing well 2 mo following discharge.
Peripancreatic pseudoaneurysm is a rare but life-threatening complication of chronic pancreatitis[6]. Pseudoaneurysms have been found to result from a variety of mechanisms, including infection, trauma, and surgical procedures[6]. All have in common disruption of arterial continuity with extravasation of blood into the surrounding tissues. This ultimately results in the formation of a fibrous tissue capsule that progressively would enlarge due to the unrelenting arterial pressure[7]. Pancreatitis causing splanchnic arterial aneurysm is more likely to affect the splenic artery than the gastroduodenal artery. The incidence of pseudoaneurysm in patients who undergo angiography for pancreatitis is about 10%. Hemorrhage occurs in 50% of cases[8]. Clinically, pseudoaneurysm is hard to discover until rupture occurs. Pseudoaneurysm can be diagnosed approximately by using various imaging modalities including computer tomography, ultrasound, and angiography and should be entertained in any patient with a history of pancreatitis[9].
Because of the high mortality of a pseudoaneurysm, surgical resection or interventional radiology should be done as early as possible. When an intra-abdominal pseudoaneurysm is suspected, angiography is the best useful means for determining the exact location of the pseudoaneurysm. In addition, it could save time and prevent the danger of an emergency laparotomy to locate the source of bleeding without angiography[10]. In our case, emergent angiography demonstrated a pseudoaneurysm arising from the splenic artery. Many authors have recommended transcatheter occlusion or selective embolization as a useful method in high-risk patients. Pilleul et al[11], Matsumoto et al[12], and Rokke et al[13], reported successful transcatheter arterial embolization in patients who developed splenic artery pseudoaneurysm secondary to chronic alcoholic pancreatitis. Metallic coils and gelatin sponge are the most commonly employed agents in embolotherapy for splenic artery pseudoaneurysm. Stent-grafting and detachable balloon are also used[14,15]. At the first operation, we tried transcatheter arterial embolization by microcoils, but failed to make the microcatheter tip through the aneurysm neck. At last, the pseudoaneurysm and distal splenic artery were occluded by PVA and gelatin sponge through the 3F-SP microcatheter. The procedure was performed safely. Five days later, celiac artery angiogram showed that the splenic artery pseudoaneurysm disappeared, and no acute pancreatitis occurred.
Our review of the literature revealed no reported cases of embolization of splenic artery pseudoaneurysm and distal splenic artery by PVA and gelatin sponge. Usually, embolization of distal splenic artery may deduce splenic embolization and acute pancreatitis. In this case, continuous observation did not show rapid increase of serum amylase and urine amylase after the treatment.
This report describes the successful management of a pseudoaneurysm of the splenic artery following chronic alcoholic pancreatitis, by embolization of the pseudoaneurysm and distal splenic artery.
| 1. | Tessier DJ, Stone WM, Fowl RJ, Abbas MA, Andrews JC, Bower TC, Gloviczki P. Clinical features and management of splenic artery pseudoaneurysm: case series and cumulative review of literature. J Vasc Surg. 2003;38:969-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 234] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 2. | Cirocchi R, De Leo S, Covarelli P, Goracci G, Lauro A, Gerardi GA, Bisacci R, Fabbri C. Splenic pseudoaneurysms following acute pancreatitis. Minerva Chir. 1999;54:277-282. [PubMed] |
| 3. | Maleux G, van Steenbergen W, Stockx L, Vanbeckevoort D, Wilms G, Marchal G. Multiple small pseudoaneurysms complicating pancreatitis: angiographic diagnosis and transcatheter embolization. Eur Radiol. 2000;10:1127-1129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Negi SS, Sachdev AK, Bhojwani R, Singh S, Kumar N. Experience of surgical management of pseudo-aneurysms of branches of the coeliac axis in a North Indian Hospital. Trop Gastroenterol. 2002;23:97-100. [PubMed] |
| 5. | Balsarkar DJ, Joshi MA. Rupture of splenic artery pseudoaneurysm presenting with massive upper gastrointestinal bleed. Am J Surg. 2002;183:197-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | de Perrot M, Berney T, Bühler L, Delgadillo X, Mentha G, Morel P. Management of bleeding pseudoaneurysms in patients with pancreatitis. Br J Surg. 1999;86:29-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 114] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 7. | Carr JA, Cho JS, Shepard AD, Nypaver TJ, Reddy DJ. Visceral pseudoaneurysms due to pancreatic pseudocysts: rare but lethal complications of pancreatitis. J Vasc Surg. 2000;32:722-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 111] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | Sreedharan VK, Shenoy KR, Shenoy MG. Upper gastrointestinal bleeding in tropical pancreatitis due to pseudoaneurysm rupture. Trop Doct. 2003;33:57. [PubMed] |
| 9. | Flati G, Andrén-Sandberg A, La Pinta M, Porowska B, Carboni M. Potentially fatal bleeding in acute pancreatitis: pathophysiology, prevention, and treatment. Pancreas. 2003;26:8-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 150] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 10. | de Perrot M, Buhler L, Schneider PA, Mentha G, Morel P. Do aneurysms and pseudoaneurysms of the splenic artery require different surgical strategy? Hepatogastroenterology. 1999;46:2028-2032. [PubMed] |
| 11. | Pilleul F, Dugougeat F. Transcatheter embolization of splanchnic aneurysms/pseudoaneurysms: early imaging allows detection of incomplete procedure. J Comput Assist Tomogr. 2002;26:107-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 27] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Matsumoto Y, Yamashita S, Aso M, Kawasaki A, Kajihara E, Iwai K, Aoyagi K, Sadoshima S, Onoyama K. A case of colonic hemorrhage caused by splenic artery pseudoaneurysm penetrating into the colon: management by transcatheter arterial embolization. Nihon Shokakibyo Gakkai Zasshi. 1998;95:916-920. [PubMed] |
| 13. | Røkke O, Søndenaa K, Amundsen SR, Bjerke Larssen T, Jensen D. Successful management of eleven splanchnic artery aneurysms. Eur J Surg. 1997;163:411-417. [PubMed] |
| 14. | Tsang LL, Lee TY, Chen TY, Cheng YF. Microcoils embolization of splenic artery pseudoaneurysm complicated with chronic pancreatitis. Hepatogastroenterology. 2002;49:842-843. [PubMed] |
| 15. | Brountzos EN, Vagenas K, Apostolopoulou SC, Panagiotou I, Lymberopoulou D, Kelekis DA. Pancreatitis-associated splenic artery pseudoaneurysm: endovascular treatment with self-expandable stent-grafts. Cardiovasc Intervent Radiol. 2003;26:88-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
Science Editor Zhu LH Language Editor Elsevier HK