Published online Aug 15, 2004. doi: 10.3748/wjg.v10.i16.2455
Revised: March 26, 2004
Accepted: March 4, 2004
Published online: August 15, 2004
We report a case of a 61-year-old man who presented with fatigue, abdominal pain and hepatomegaly. Computed tomography (CT) of the abdomen showed hepatomegaly and multiple hepatic lesions highly suggestive of metastatic diseases. Due to the endoscopic finding of colon ulcer, colon cancer with liver metastases was suspected. Biochemically a slight increase of transaminases, alkaline phosphatase and gammaglutamyl transpeptidase were present; α - fetoprotein, carcinoembryogenic antigen and carbohydrate 19-9 antigen serum levels were normal. Laboratory and instrumental investigations, including colon and liver biopsies revealed no signs of malignancy. In the light of spontaneous improvement of symptoms and CT findings, his personal history was revaluated revealing direct contact with pigs and their tissues. Diagnosis of leptospirosis was considered and confirmed by detection of an elevated titer of antibodies to leptospira. After two mo, biochemical data, CT and colonoscopy were totally normal.
- Citation: Granito A, Ballardini G, Fusconi M, Volta U, Muratori P, Sambri V, Battista G, Bianchi FB. A case of leptospirosis simulating colon cancer with liver metastases. World J Gastroenterol 2004; 10(16): 2455-2456
- URL: https://www.wjgnet.com/1007-9327/full/v10/i16/2455.htm
- DOI: https://dx.doi.org/10.3748/wjg.v10.i16.2455
Leptospirosis is a zoonosis caused by spirochetes of the genus Leptospira. Humans are infected only occasionally by direct contact with infected animals or through contaminated water and soil. The clinical presentation ranges from occult infection to Weil’s disease with fatal complications as hepatorenal failure. It remains underdiagnosed largely due to the broad spectrum of symptoms and signs.
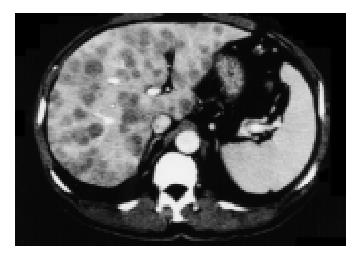
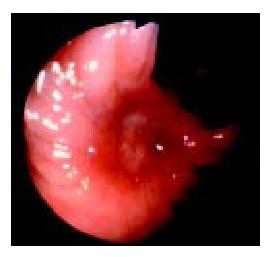
A 61 year-old male farmer, non-smoker without a history of alcohol abuse or cancer, was admitted to a local hospital due to fatigue and pain in the right upper abdominal quadrant with discovery of enlarged liver over the past three days, Ultrasonography (US) showed many hypoechoic lesions scattered in all hepatic segments. A computed tomography (CT) scan of the abdomen showed substitution of the whole liver by multiple low-density lesions with mild ring enhancement highly suggestive of metastatic disease (Figure 1) and retroperitoneal small ( < 1 cm) lymph nodes. Upper gastrointestinal endoscopy was negative and colonoscopy disclosed an ulcer of the transverse colon which hystologically revealed edema and necro-inflammatory damage without signs of malignancy.
Ultrasound guided liver biopsy of one of the lesions taken 10 d after admission excluded malignancy and was consistent with mild portal hepatitis and cholestasis. Laboratory tests showed alanine aminotransferase (ALT) 130 IU/l (normal < 40), aspartate aminotransferase (AST) 76 IU/l (normal < 37), alkaline phosphatase (ALP) 359 MU/mL (normal < 280), gammaglutamyl transpeptidase (γ -GT) 252 MU/mL (normal < 50). Normal serum levels of α -fetoprotein, carcinoembryogenic antigen (CEA) and carbohydrate 19-9 antigen (CA 19-9) were present. The patient refused further investigations and was discharged with the suspicion of misdiagnosed neoplastic disease. Four wk later, on admission to our Unit, the patient was in good general condition and denied a weight loss and gastrointestinal symptoms. Physical examination revealed only a mild indolent hepatomegaly. Laboratory investigations showed only ALP 443 MU/mL and γ -GT 77 MU/mL. Ultrasonography and abdominal CT scan (Figure 2) revealed a dramatic decrease both in number and volume of the hepatic lesions with unmodified vascularization pattern. Chest X-ray was unremarkable. Colonoscopy revealed an ulcer of the right colon (Figure 3) characterized under histological profile by edema and necro-inflammatory cells. Viral, autoimmune and metabolic liver diseases were excluded by appropriate tests as well as metastatic tumors, primary hepatoma, pyogenic liver abscess, parasitic liver and colon lesions and colon cancer. Due to spontaneous improvement of symptoms and CT findings, his personal history was revaluated. A direct contact with pigs and their tissues three days before the onset of symptoms was reported (the patient, living in rural areas, butchered a domestic pig). On specific request, transient hematuria before admittance was reported. The hypothesis of leptospirosis was considered and confirmed by the positive result of indirect immunofluorescence on cultured leptospires (Leptospira interrogans serovar icterohaemorraghiae), which showed a high titer of antibodies to leptospira (titer 1:1024). No cross-reaction with other spirochetes (Treponema and Borrelia) was seen. In two wk’ time biochemical alterations were almost subsided. Despite spontaneous recovery, treatment with tetracyclines was started and the patient was dismissed. Two mo later US, CT and colonoscopy were totally normal and after a 2-year follow-up the patient has been fine.
Leptospirosis is a worldwide zoonotic infection that commonly occurs in tropical and subtropical regions and in both urban and rural contexts. Human disease is acquired by contact with urine or tissues of an infected animal or through contaminated water and soil, whereas human-to-human transmission is rare. Diagnosis of leptospirosis is based either on isolation of the organism from the patient or on seroconversion. Antibodies generally do not appear until the second week of illness. The pathogenesis of leptospirosis is incompletely understood but it is well known that all forms of leptospires can damage small blood vessels, lead to vasculitis and spread to all organs[1]. The clinical presentation ranges from occult infection to Weil’s disease with fatal complications as hepatorenal failure. The severity of disease reflects the severity of the underlying vasculitis. As a result of its protean clinical manifestations and non-specific presentations, leptospirosis has been underdiagnosed and frequently misdiagnosed as other diseases such as influenza, viral hepatitis, encephalitis, pneumonitis and acute renal failure[1-3]. The great majority of cases, as in this patient, were of mild severity (anicteric leptospirosis) and resolution coincided with the appearance of antibodies. Icteric leptospirosis, occurring between 5 and 10 % of patients, was a severe disease and often very rapidly progressive with multi-organ failure[4,5]. Treatment of leptospirosis depends on the severity of infection. Anicteric leptospirosis often requires hospital admission and close observation. Streptomycin, penicillins, cephem and tetracyclines are all effective anti-leptospiral antibiotics[4,5]. Radiological abnormalities, in particular pulmonary localization on high resolution CT (nodular densities, ground glass opacities, areas of consolidation) possibly related to haemorrhage, have been described in severe forms[6-8]. Although hepatomegaly is usual, CT evidence of multiple hepatic lesions, to our knowledge, has not yet been described in patients with leptospirosis. The histopathology of the liver in the course of leptospirosis was characterized by intrahepatic cholestasis, centrilobular necrosis with hypertrophy and hyperplasia of Kupffer cells but the architecture of parenchyma was not significantly disrupted and severe hepatic necrosis was not usual[4]. The presence of multiple hypoattenuated nodules in the liver was the most interesting feature of this case. The differential diagnosis of this CT appearance included hypovascular metastases, abscess, especially by angioinvasive organisms or lymphoma. However, the absence of a mass effect on the surrounding hepatic structures would be helpful in suggesting the possibility of an abscess correlated with damage of small blood vessels. The pathologic basis for this hypoattenuation may be correlated with a coagulative necrosis of the hepatic tissues caused by vasculitis of the hepatic vessels.
Gastrointestinal involvement with haemorrhage has been reported, mainly in the severe form of leptospirosis[2]. Interestingly, in this patient a colon ulcer was found at two different sites without any symptoms and signs of bleeding. The endoscopic and histological patterns of these colon lesions were consistent with ischemic colitis. Vascular disease of diverse etiologies and in particular vasculitis could be a cause of ischemic colitis[8].
In this patient, according to our experience, liver lesions were correlated with the endoscopic findings of colon ulcer therefore primary colon cancer with liver metastases was suspected initially. On the other hand, the CT pattern when seen in the appropriate clinical setting reduced the diagnostic suppositions of infectious disease.
In conclusion, this case, initially misdiagnosed as colon cancer with liver metastases, confirms clinical polymorphism of leptospirosis and high lights the role of a good knowledge of personal history and epidemiological data in the diagnosis of leptospirosis, especially in areas of relatively low endemicity as in western countries, where domestic animal contact is prominent sources of infection. This report also suggests that a diagnosis of leptospirosis should be considered in patients with laboratory and CT findings of liver involvement and a relevant history.
| 1. | Plank R, Dean D. Overview of the epidemiology, microbiology, and pathogenesis of Leptospira spp. in humans. Microbes Infect. 2000;2:1265-1276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 187] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 2. | Lecour H, Miranda M, Magro C, Rocha A, Gonçalves V. Human leptospirosis--a review of 50 cases. Infection. 1989;17:8-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Katz AR, Ansdell VE, Effler PV, Middleton CR, Sasaki DM. Assessment of the clinical presentation and treatment of 353 cases of laboratory-confirmed leptospirosis in Hawaii, 1974-1998. Clin Infect Dis. 2001;33:1834-1841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 146] [Article Influence: 5.8] [Reference Citation Analysis (1)] |
| 4. | Levett PN. Leptospirosis. Clin Microbiol Rev. 2001;14:296-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1940] [Cited by in RCA: 1889] [Article Influence: 75.6] [Reference Citation Analysis (0)] |
| 5. | Kobayashi Y. Clinical observation and treatment of leptospirosis. J Infect Chemother. 2001;7:59-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Lee RE, Terry SI, Walker TM, Urquhart AE. The chest radiograph in leptospirosis in Jamaica. Br J Radiol. 1981;54:939-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. |
Henk CB, Kramer L, Schoder M, Bankier AA, Ratheiser K, Mostbeck GH; Weil disease: importance of imaging findings for early diagnosis. |
| 8. | Yiu MW, Ooi GC, Yuen KY, Tsang KW, Lam WK, Chan FL. High resolution CT of Weil's disease. Lancet. 2003;362:117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
Edited by Zhu LH Proofread by Xu FM