MATERIALS AND METHODS
Main reagents
RPMI1640 was produced by Gibco, fetal bovine serum was produced by Hyclone, and 96-well plates by Costa. Dimethyl sulfoxide (DMSO), ethylenediaminetetra-aceticacid (EDTA), 3-(4,5-dimethy1-thiazol-2-yl), 2,5-diphenyl tetrazlium bromide (MTT), N-2-Hydroxyethlpiperazine-N’-2-ehtane sulfonine acid (HEPES), and trypin were all products of Sigma. Rat desmin monoclonal antibody and rat α-SMA monoclonal antibody were bought from DAKO, rat synapsin monoclonal antibody was bought from Santa Cruz. Rat collagen I and III monoclonal antibodies, rat TIMP and PDGF as well as TGF-β1 monoclonal antibodies, ABC and DAB test kits were all bought from Beijing Zhongshan Biotechnology Inc.
SD rat HSC line
The HSC line was established in our laboratory and prepared after long-term generation.
Preparation of SD rat serum[
8]
Normal SD rat serum A normal rat weighting 350 g fasted for 12 h was injected with diethylether for anesthesia. Under the sterile condition, 10 mL blood was obtained from abdominal aorta, then held for 2 h at room temperature. Blood serum was made by centrifugation at 427 g for 10 min, inactivated at 56 °C for 60 min, and frozen at -60 °C.
Hepatic fibrosis model SD rat serum Adapted Hernandez-Munoz method was used to establish animal model of hepatic fibrosis[9], 0.2 mL CCl4 (Olive oil, 1:6 dilution) was injected into abdominal cavity, three times each week for 7 wk. Serum preparation and preservation were the same as those of the normal SD rat serum.
Drug serum With 3.5, 7 and 14 times of human body dosage as low, medium and high dosage groups respectively, CBJRGC was perfused into rat stomach 3 times at 12 h intervals. Rats were fasted for 12 h before the third perfusion and blood sampling was conducted from abdominal aorta 2 h after the third perfusion. Serum preparation and preservation were the same as those of the normal SD rat serum.
Cell culture and grouping
Rat HSCs were inoculated in RPMI1640 with 100 g/L fetal bovine serum, and cultivated at 37 °C in an incubator containing 50 mL/L CO2 to logarithm growth time. After treatment with digestive fluid, HSCs were suspended by adding D-Hank’s fluid, deposited by centrifugation at 190 g with 5 min, and then counted. Using RPMI1640 containing 100 g/L fetal bovine serum, HSCs were adjusted to a density of 5 × 104/mL and added to a 24-well plate containing flying sheet, 0.2 mL each well. According to intervening factors, HSCs were divided into 5 groups, i.e. control group, model group, high dosage serum group, medium dosage serum group and low dosage serum group. Each group had 4 wells. Upper culture medium was removed after cultivated for 12 h. Control group serum, model group serum, high dosage group serum, medium dosage group serum and low dosage group serum were accordingly added. Flying sheets were taken out respectively at 24 h, 48 h and 72 h, fixed with cold acetone for 10 min, dried and preserved at -60 °C.
Using MTT method to detect effect of drug serum on proliferation of HSC
HSCs with a density of 5 × 104/mL were added to a 96-well plate, 0.2 mL each well. Each group contained 8 wells. Upper medium was removed after cultivated for 12 h. Control group serum, model group serum, high dosage group, medium dosage group serum and low dosage group serum were accordingly added. 50 μL cultivating fluid was taken out respectively at 24 h, 48 h and 72 h. A 50 μL of MTT (50 μg MTT) was then added and the culture continued for 4 h at 37 °C. After upper fluid was removed, 150 μL DMSO was added to each well. After concussed and dissolved, Absorbency value with wave-length of 450 nm was detected by enzyme labeled instrument (BioRad 2250, Japan). The test was repeated 5 times.
Immunohistochemical staining
α-SMA staining Preserved cell flying sheets were immersed with PBC for 5 min, blocked with 10 mL/L H2O2 for 10 min, washed 3 times with PBC, 5 min each time, and then incubated with 10% goat serum for 30 min. Rat α-SMA, desmin, synapsin collagens I and II, TIMP, TGFβ1 and PDGF antibodies were diluted at a concentration of 1:100 and added as the first antibodies, staying overnight at 4 °C. After washed 3 times with PBC, 5 min each time, biotin goat anti-rat IgM was added, staying overnight at 4 °C, washed with PBC 3 times, 5 min each time. Streptavidin was added for 30 min, stained with DAB. The first antibody was replaced with fetal bovine serum as negative control, α-SMA male staining Absorbency value and relative area occupied by α-SMA male cells in the reference system were detected with TN-8502 image analysis system (Tractor Northern Co, USA). Data were treated with SPSS for ANOVA test. Results were presented mean ± SD. P < 0.05 was considered statistically significant.
DISCUSSION
In past studies about traditional Chinese medicine, the method of adding directly coarse extract of the medicine to environment of cells was adopted in most experiments in vitro. Because of the complicated components of traditional Chinese medicine, it could not effectively reflect its pharmacological role. Therefore, we adopted the blood serum pharmacological method in our experiment[8]. After giving the drug to the animal orally, we took the drug serum as the drug source to add to the response system in vitro. This method could not only present the biotransformation in vivo, but also overcome confusion of other substances, aiding to makea pharmacokinetic study by finding the effective locus and the activity of components of traditional Chinese medicine. To avoid influence of different species animal sera on cells, animals were adopted in our experiment which were the same species with cultivated HSCs. Considering that the tested object of the drug was cells and the drug with biological reactivity in organism, we gave the drug to the animal orally with an equivalent dosage, to assure the maximum homeostasis concentration of the drug after bioconversion in vivo. The results of our experiment indicated that our experiment method was effective, stable and reliable.
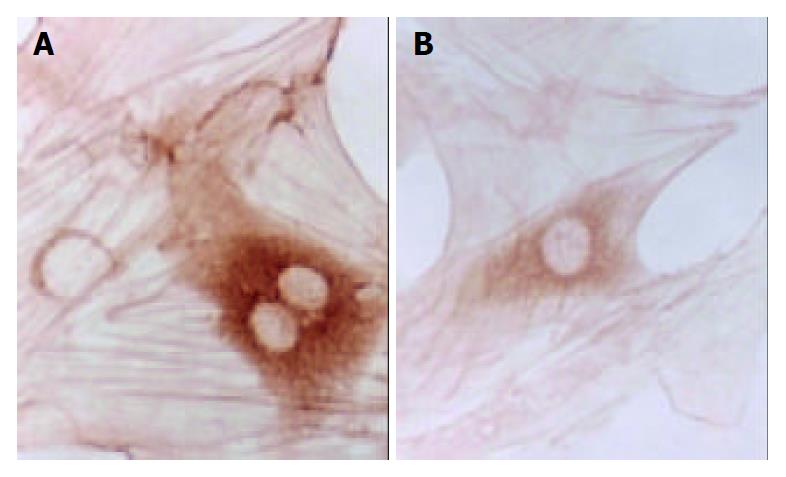
A recent investigation has shown that proliferation and activation of HSCs are not only the central link of hepatic fibrosis, but also the cytological background of hepatic fibrosis[10,11]. Therefore, inhibiting the proliferation and activation of HSC has important significance in prevention and treatment of chronic liver disease and anit-hepatic fibrosis. Cultivated in a non-coating plastic Petri dish, HSC could be automatically activated, thus possessing the biological characteristics of activation in vivo, and becoming an ideal anti-hepatic fibrosis cell model[12]. Just as shown by the results of our experiment, with elongation of cultivating time, HSC showed multi-angle pseudopodium and typical star form. Cell proliferation and collagen synthesis were two important behaviors in activation of HSC. MTT chromatometry methods could be employed to detect cell ability of proliferation, which was based on the principle that succinic dehydrogenase in mitochondria of living cells could make ectogenical MTT recover to non-dissoluable blue and purple crystals and deposit in cells. DMSO could dissolve blue and purple crystals in cells. Adopting enzyme labled instruments to detect the Absorbency value at some wave-length, the quantity of cells could be reflected indirectly.
The results of our experiment showed that there was no significant difference (P > 0.05) between all the groups 24 h after serum was added. It means that adding serum to cultivate for 24 h did not exert any effective influence and HSCs still proliferated at its original rate, suggesting that intervention in proliferation of HSCs needs a time process, which from accepting excitation of cell signal to changing proliferation quantity of HSC, is undoubtedly longer than 24 h. Thus, how to restrain the activation of HSC at earlier time to hold back quick proliferation of HSC, has undoubtedly important significance in prevention and cure of hepatic fibrosis. Our results showed that proliferation of HSC in model group in 48 h and 72 h had a significant difference compared with other groups, indicating that the model group might contain substances which could promote quick proliferation of HSC. The reason may be that after cultivated for 48 h and 72 h, the PDGF of HSC in the model group increased to the effective content, leading to excessive proliferation of HSC. But a 24 h cultivation was not enough for PDGF to increase to the effective content. This could explain our results that there was no significant proliferation of HSC in the model group after 24 h serum culture. The results of our experiment also showed that after cultivated for 48 h and 72 h, there were significant differences among the high, medium and low dosage drug serum groups and the model group (P < 0.05), and between the high and medium dosage drug serum groups and the control group (P < 0.05), indicating that different dosage drug sera could inhibit the proliferation of HSC, and had an especially significant effect on the high and medium dosage groups. CBJRGC serum could significantly decrease and inhibit the proliferation of HSC. Its mechanism may be related to the inhibition of self-excretion or para-excretion of PDGF and TGF-β1[13], thus inhibiting the proliferation of HSC by decreasing the conversion from HSC to α-SMA.
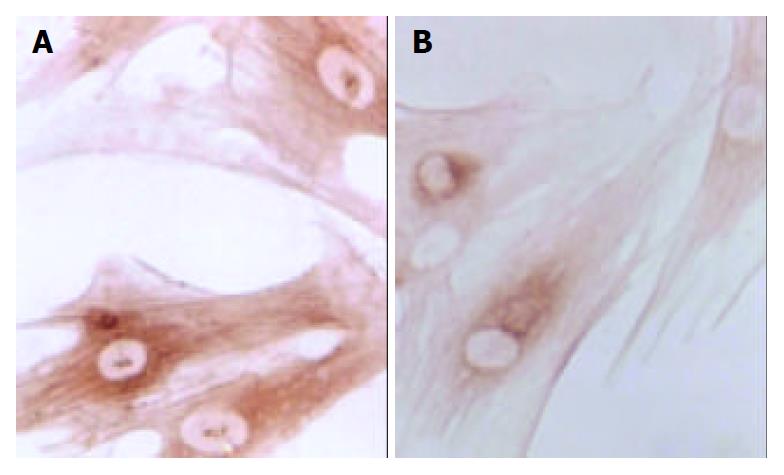
Changes in form and function after HSC is activated could lead to production increase and degradation decrease of ECM, eventually resulting in deposition of hepatic collagens and hepatic fibrosis. Desmin could be regarded as a marker of HSC[14], and α-SMA as the marker of activation of HSC[15]. α-SMA is a kind of filament protein which is about 7 nm in diameter and mainly exists in smooth muscle cells as a portion of cytoplasm framework and a functional unit of cell contraction. Under normal conditions, this protein mainly exists in smooth muscle cells and myofibroblasts. There is a very small amount of this protein in HSCs of rats. In the animal model of liver diseases, HSC lost desmin expression and was changed to the expression of α-SMA in its activation process. So, α-SMA could be regarded as the marker of activation of HSC[16]. In the process of inducing rat hepatic fibrosis by CCl4[17], the dynamic change of desmin male cells was a mono-cusp curve, increasing in number in the earlier period, reaching the peak in 12 wk and then gradually decreasing. A foreign study has found that increase of expression of synapsin could be regarded as another marker of activation of HSC[18]. Our results showed that the dynamic changes in A value of male staining of α-SMA, desmin and synapsin and in the area occupied by α-SMA and synapsin male cells were almost synchronical. The area occupied by desmin male cells showed a tendency to decrease with elongation of cultivating time. This result was consistent with that reported by Li et al[19] that HSC lost the expression of desmin in its activation process, suggesting that in the process of hepatic fibrosis, α-SMA, desmin and synapsin all can be regarded as the markers of activation of HSC, but each has its own characteristics. The expression of desmin in the earlier period of activation was significant, but weakened with elongation of activating time, while the expression of α-SMA and synapsin developed with elongation of activating time. It is estimated that activation and proliferation of HSC can synchronically occur. Our results also showed that after cultivated for 24 h, the expression of α-SMA had no significant difference among all groups, and after cultivated for 48 h, α-SMA male cell area was smaller than that of desmin, indicating that in the period of cultivation for 24 h and 48 h, proliferation was the main form of HSC growth, but with elongation of cultivating time, HSC began to be partly activated and changed to expression of α-SMA. Seventy-tow h after cultivation, α-SMA male cell area was bigger than desmin male cell area, the amount of activated HSCs was more than that of silent HSCs and lots of HSCs altered in phenotype, further indicating that the activation of HSC could be synchronically expressed as proliferation and transformation of HSC. The results of our experiment showed that CBJRGC serum could inhibit the expressions of α-SMA, desmin and synapsin in HSC and inhibit the activation of HSC, whose drug effect was closely related to the concentration of drug serum.
Synapsin can be regarded as a new marker of activation of HSC. Its significance is to provide an important theoretic and testing basis for neuroregulation in the process of hepatic fibrosis. So far, no such study has been found in China. Our experiment firstly showed that after cultivated for 24 h, synapsin could express in HSC, and after cultivated for 48 h and 72 h, synapsin could continue to express. Expression of synapsin occurred before it was cultivated for 24 h and continued to maintain a high level. CBJRGC serum could significantly inhibit expression of synapsin in HSC. Nevertheless, further studies such as the precise time of synapsin expression, the essential significance of the increase in its lasting expression, whether the nervous system involves regulation of stress condition of liver, and whether CBJRGC serum takes part in nervous regulation in hepatic fibrosis, are still needed.
Under normal conditions, liver contains collagen of types I, III, IV, V, and VI. Collagens I and III take the most proportion of collagen, accounting for about 60% of total collagen in liver. When hepatic fibrosis occured, the proportion of collagens I and III might reach 95% of total collagen in liver[20]. Thus, in hepatic fibrosis, deposited ECM mainly consists of collagens I and III.
Synthesis of collagen could reflect alterative ability of individual fiber hyperplasia of cells[21]. Our experiment showed that after cultivated for 24 h, there was no significant difference of collagens I and III among all groups, indicating that within 24 h after acceptance of activating signal, HSC did not yet achieve enough time to excrete collagen. The outcome of our experiment showed that activated time should be longer than 24 h, so that activated HSC and transcription of collagen and cytokine could be altered. In further investigations we should observe and analyze changes in collagen-mRNA in this time process to test whether CBJRGC serum can influence collagen-mRNA. The results also suggested that to inhibit collagen in its transcriptional stage might have important significance in clinical treatment. In our experiment, collagen III began to markedly express after cultivated for 48 h, but collagen I started to markedly express after cultivated for 72 h, showing that expression of collagen III was earlier than that of collagen I, and that in the early time of hepatic fibrosis, collagen III expression took the most part of expression of collagen. Therefore collagen III can be the testing index of earlier hepatic fibrosis. The outcome of our experiment also showed that high and medium dosage groups could significantly inhibit the expression of collagen III in 48 h and 72 h and the expression of collagen I in 72 h. It means CBJRGC serum could play a role in anti-hepatic fibrosis at the earlier time when collagen was significantly expressed. It further suggested that CBJRGC serum could help quickly recover equilibration of synthesis and degradation of ECM in hepatic fibrosis, thus helping to cure hepatic fibrosis. Besides, low dosage group could only significantly inhibit the expression of collagen III in 48 h, but there was no significant difference compared with control group in 72 h. It is estimated that the effect of CBJRGC serum in inhibiting collagen III expression is related to the serum concentration of the drug.
MMP and TIMP mainly take part in regulation of equilibration in synthesis and degradation of collagen[22]. Among numerous MMPs, MMP1 is the chief MMP, decomposing collagens I and III in liver[23]. TIMP1 is an inhibiting factor of MMP, which plays its role by irreversibly binding to activated MMP1. Therefore, the imbalance of ratio of MMP/TIMP 1 plays a very important role in hepatic fibrosis. MMP can be inhibited by many specific or non-specific inhibitors, which at present, mainly include TIMP and α2- macroglobulin. TIMP 1 is the most important inhibitor of MMP and is negatively correlated to the activity of MMP.
TIMP is a kind of coding protein of multigene family[24]. It could irreversibly bind to activated MMP and inhibit the degradation of ECM[25]. So far, there are four kinds of TIMP isolated from tissues and cloned[26]. TIMP-1 is a kind of 28.5 ku glycoprotein, mainly inhibiting the activity of MMPs-1 and MMP-9. As the specific inhibitor of MMP, TIMP plays a very important role in hepatic fibrosis. TIMP could inhibit MMP, which is the important reason for specific descent of degradation of ECM[27]. HSC is the main source cell of TIMP and MMP.
The results of our experiment showed that after cultivated for 24 h, there was no significant expression of TIMP in all groups, indicating that HSC did not have enough time to excrete excessive TIMP. The activated time should be longer than 24 h, and within this time, transcription of TIMP of activated HSC might be altered. In further studies, we should observe and analyze the change of TIMP-mRNA within this time, so as to find whether CBJRGC serum can influence TIMP-mRNA. It is also suggested that to inhibit TIMP in transcriptional stage might have important significance in clinical treatment. In this experiment, TIMP of the model group maintained high expression in 48 h and 72 h, indicating that there was some substance to promote high expression of TIMP in the model group. Further study on the precise characteristics of the substance is suggested.
Researches have found that HSC is the key cell in hepatic fibrosis. Under the stimulation of chronic injury and inflammation, HSC can be activated from normal silent behavior to MFB, and meanwhile can secrete and synthetize excessive ECM, forming the foundation of hepatic fibrosis. Previous studies have indicated that activation and phenotype conversion of HSC are closely related to TGF-β1. TGF-β is a kind of polypeptide molecule of hormone activity, which is produced from kupffer cells by self-excretion and para-excretion and could take part in many pathological and physiological processes[28]. TGF-β has at least 5 sub-types, but there are only TGF-β1,TGF-β2 and TGF-β3 in human tissue cells. After binding to the recipient on the membrane, TGF-β could phosphorate and activate its signal transduction molecule (SMAD protein) of intracytoplasmic downstream, which could subsequently enter the nucleus, regulating the transcription of related target gene[29]. TGF-β1 exhibits the significant biological activity of TGF-β and is the main cytokine inducing the production of collagen. Through the mechanism of para-excretion and self-excretion, TGF-β1 could start and maintain the activation of HSC, regulating cell proliferation, accelerating transcription of collagen and proliferation of ECM[30].
The results of our experiment showed that after cultivated for 24 h, there was no significant expression of TGF-β1 among all groups. It showed that it was not enough for HSC to secrete TGF-β1 24 h after it received the activated signal. It is suggested that in further studies we should observe and analyze the change in TGF-β1-mRNA within this time, so as to find whether CBJRGC serum can influence TGF-β1-mRNA. Our results also showed that after cultivated for 48 h and 72 h, TGF-β1 in the model group maintained high expression, suggesting that it could continuously stimulate activated HSC to produce collagen and accelerate hepatic fibrosis. There might be some substance in the model group which could promote high expression of TGF-β1. Study on the precise characteristics of this substance is still needed. The results also showed that the high and medium dosage groups could markedly inhibit the expression of TGF-β1 in 48 h and 72 h, but the low dosage group did not obviously inbibit the expression of TGF-β1 in 48 h and 72 h, suggesting that CBJRGC serum can inhibit the expression of TGF-β1 and its effectiveness is related to the concentration of the drug serum.
PDGF is a kind of splitting agent and can promote activation and proliferation of HSC. It has been found PI3-K is the important pathway of intramembrane signal transduction[31]. The outcome of our experiment showed that after cultivated for 24 h, the A value and male cell area of PDGF were not completely consistent. In 24 h, the A value of PDGF in the model group was significantly higher than that in the other groups, but the male cell area did not show any significant difference compared with the other groups. Although PDGF in the model group achieved significant expression, the PDGF might not entirely come from the excretion of HSC and might include original PDGF existing in the model group. While PDGF bound to PDGF recipient of HSC and accelerated the proliferation of HSC, the absolute proportion of HSC in the situation of excretion of PDGF did not significantly increase. The outcome of our experiment showed that the high, medium and low dosage groups all could obviously inhibit the excretion of PDGF by HSC.
In summary, we suggest that further studies on the mechanism of anti-hepatic fibrosis of CBJRGC serum should focus on mRNA expression of TIMP1, collagens I, III and TGF-β1 and signal transduction within the cell.