©The Author(s) 2003.
World J Gastroenterol. Apr 15, 2003; 9(4): 813-817
Published online Apr 15, 2003. doi: 10.3748/wjg.v9.i4.813
Published online Apr 15, 2003. doi: 10.3748/wjg.v9.i4.813
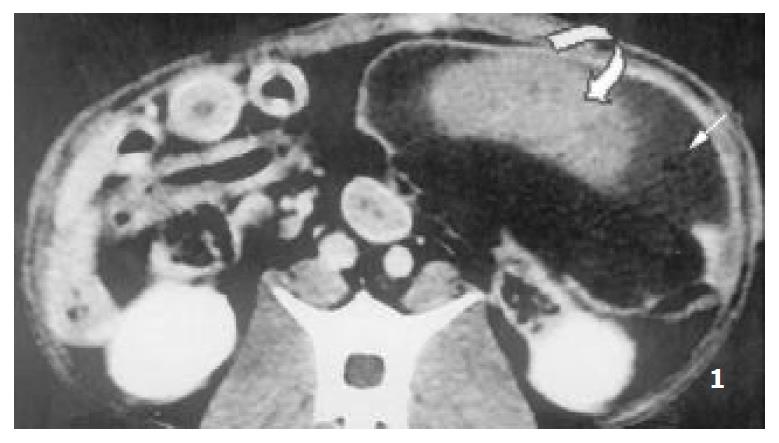
Figure 1 Enhanced CT demonstrated multiple segmental ab-lated lesion at the end of 2nd week after RFA, the splenic cap-sule was continuous, the thermal lesion included 2 zones, namely hyperintense zone of coagulative necrosis and periph-eral hypointense infarcted zone; no perisplenic or splenic abcess was seen.
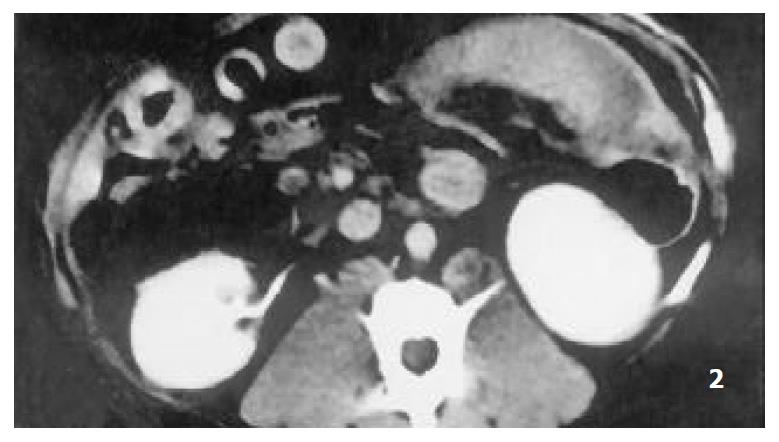
Figure 2 The lesion of infarcted zone was mostly absorbed at the end of 6th week after RFA.
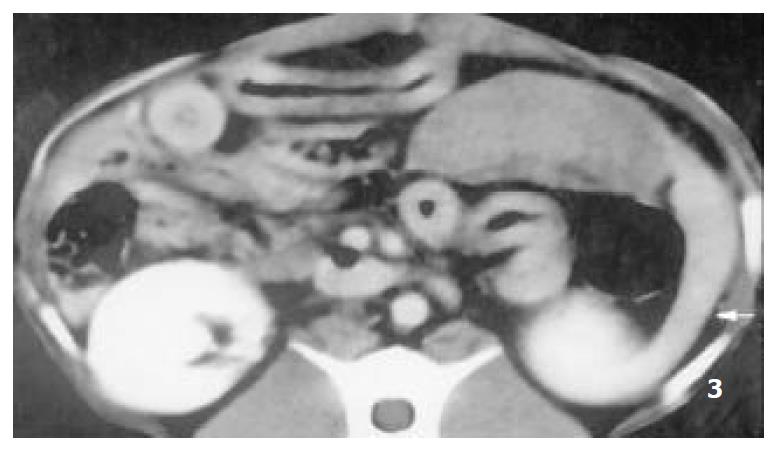
Figure 3 The lesion of infarcted zone was absorbed absolutely at the end of 9th week after RFA, however, the lesion of coagu-lative necrosis hardly altered, the remnant spleen shrinked sig-nificantly (arrow).
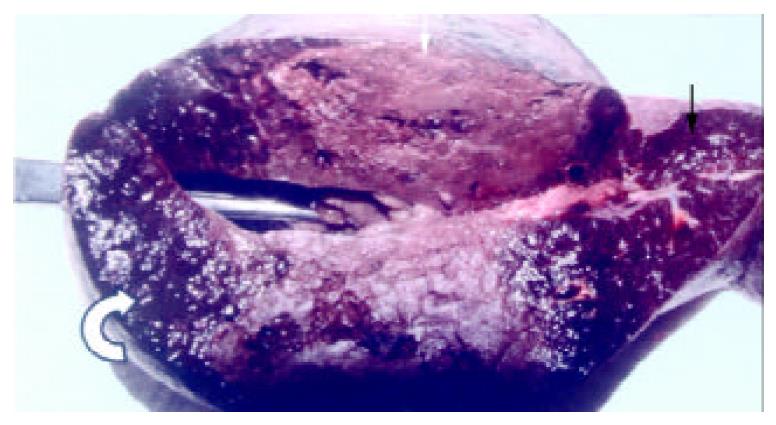
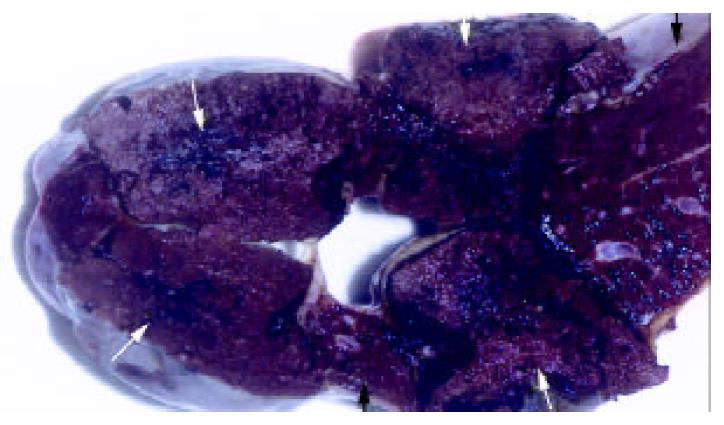
Figure 4 The appearance of the spleen the day after RFA, showed the lesion included the zone of soid-yellow dry necrosis (white arrow) and dark-red zone of thrombotic infarction (curve arrow), and the bright red normal spleen (black arrow); each ablation created a lesion with maximum diameter of 9 cm.
Figure 5 The lesion of infarcted zone was absorbed absolutely at the end of 9th week after RFA, however, the lesion of coagu-lative necrosis hardly altered (arrow).
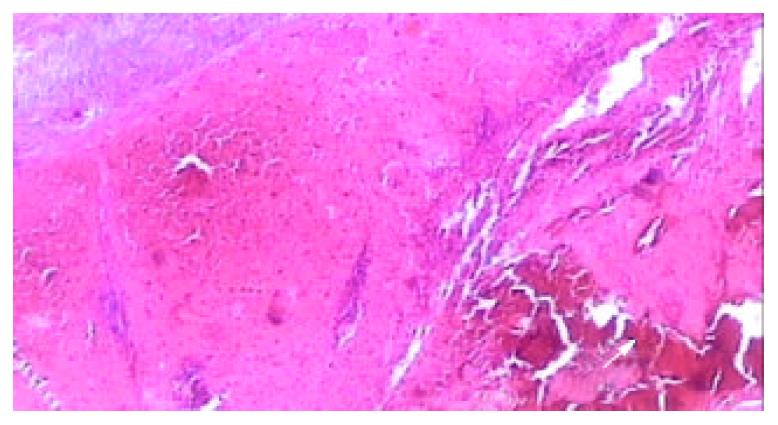
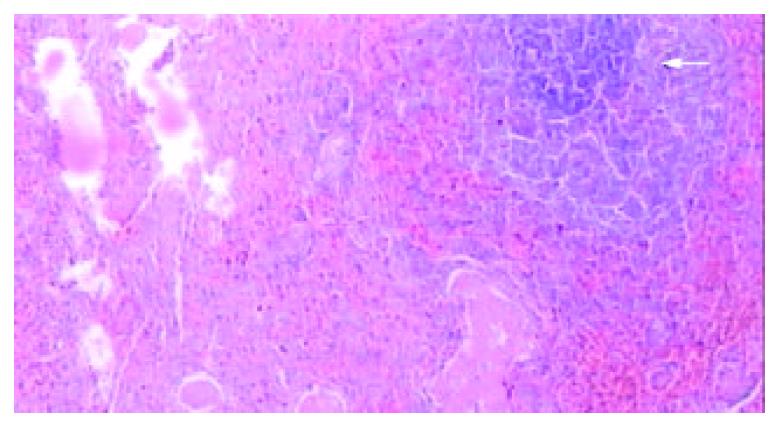
Figure 6 Light microscopic appearance of the coagulative ne-crosis at the end of 2nd week after RFA, the intrasplenic hemor-rhage at the probe insertion site could see (arrow), the splenic capsule thickened (HE.
× 40).
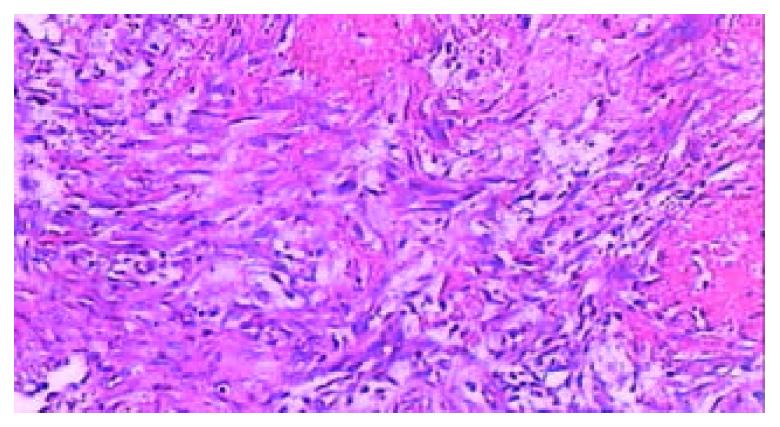
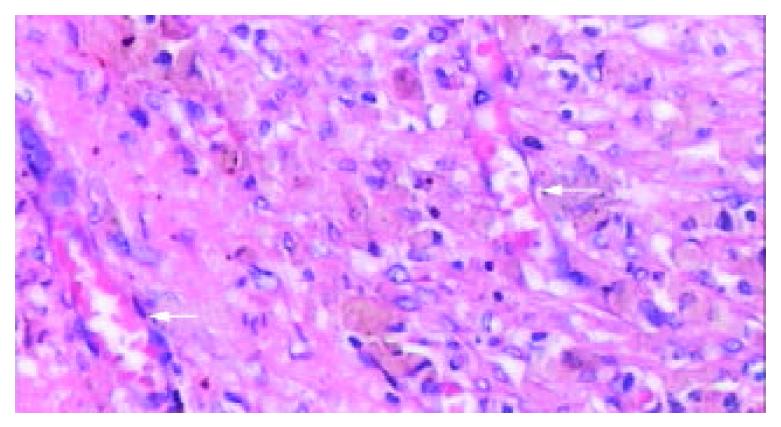
Figure 7 Microscopic examination at the junction of the ne-crotic region and infarcted region at the end of 2nd week after RFA, massive fibroblasts and inflammatory cells aggregated, the microthrombus dissolved (HE.
× 200).
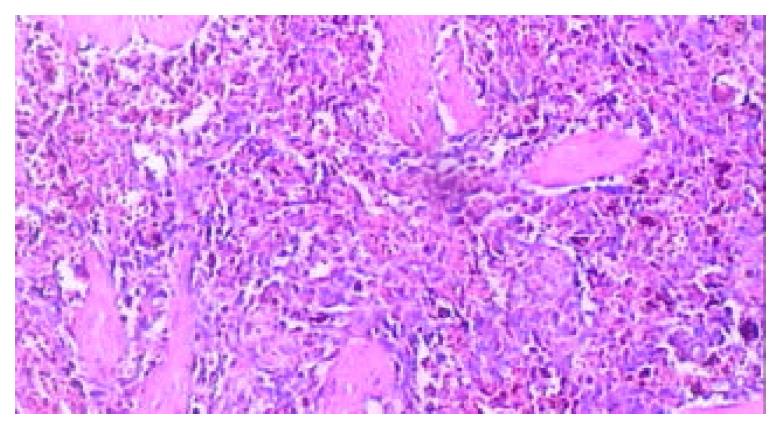
Figure 8 Microscopic examination of the thrombotic infarc-tion at the end of 4th week after RFA, the microthrombus dissolved, and extensive macrophages with hemosiderin depo-sition presented (HE.
× 100).
Figure 9 Microscopic appearance of “plenic carnification”of the normal viable splenic tissue distant form ablative lesion at the end of 9th week after RFA, the tissue structure consolidated, larger vessels occluded, extensive fibrous protein deposited, and the congestive splenic sinusoid disappeared; however, the struc-ture of splenic lymphoid nodule was intact (arrow) (HE.
× 40).
Figure 10 The typical appearance of poorly vascularized splenic tissue due to “plenic carnification” after RFA.
The splenic sinusoid disappeared, tissue structure consolidated, granular hemosiderin deposition and sparsely neovascularized vessels (arrow) presented clearly (HE. × 200).
- Citation: Liu QD, Ma KS, He ZP, Ding J, Huang XQ, Dong JH. Experimental study on the feasibility and safety of radiofrequency ablation for secondary splenomagely and hypersplenism. World J Gastroenterol 2003; 9(4): 813-817
- URL: https://www.wjgnet.com/1007-9327/full/v9/i4/813.htm
- DOI: https://dx.doi.org/10.3748/wjg.v9.i4.813