©The Author(s) 2026.
World J Gastroenterol. Jan 21, 2026; 32(3): 114226
Published online Jan 21, 2026. doi: 10.3748/wjg.v32.i3.114226
Published online Jan 21, 2026. doi: 10.3748/wjg.v32.i3.114226
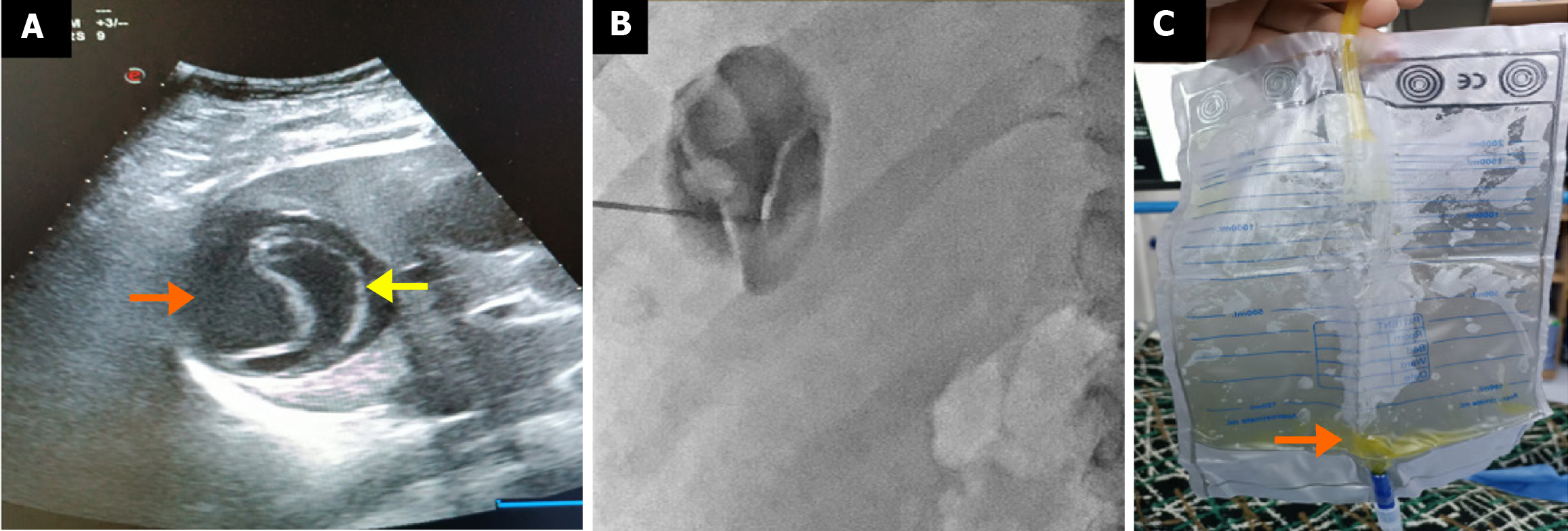
Figure 1 Ultrasound images before and after secondary catheterization in a 21-year-old patient treated percutaneously for a cystic echi
Figure 2 Symptomatic recurrent hydatid cyst in a patient previously treated percutaneously one year earlier.
A: Ultrasound shows fluid accu
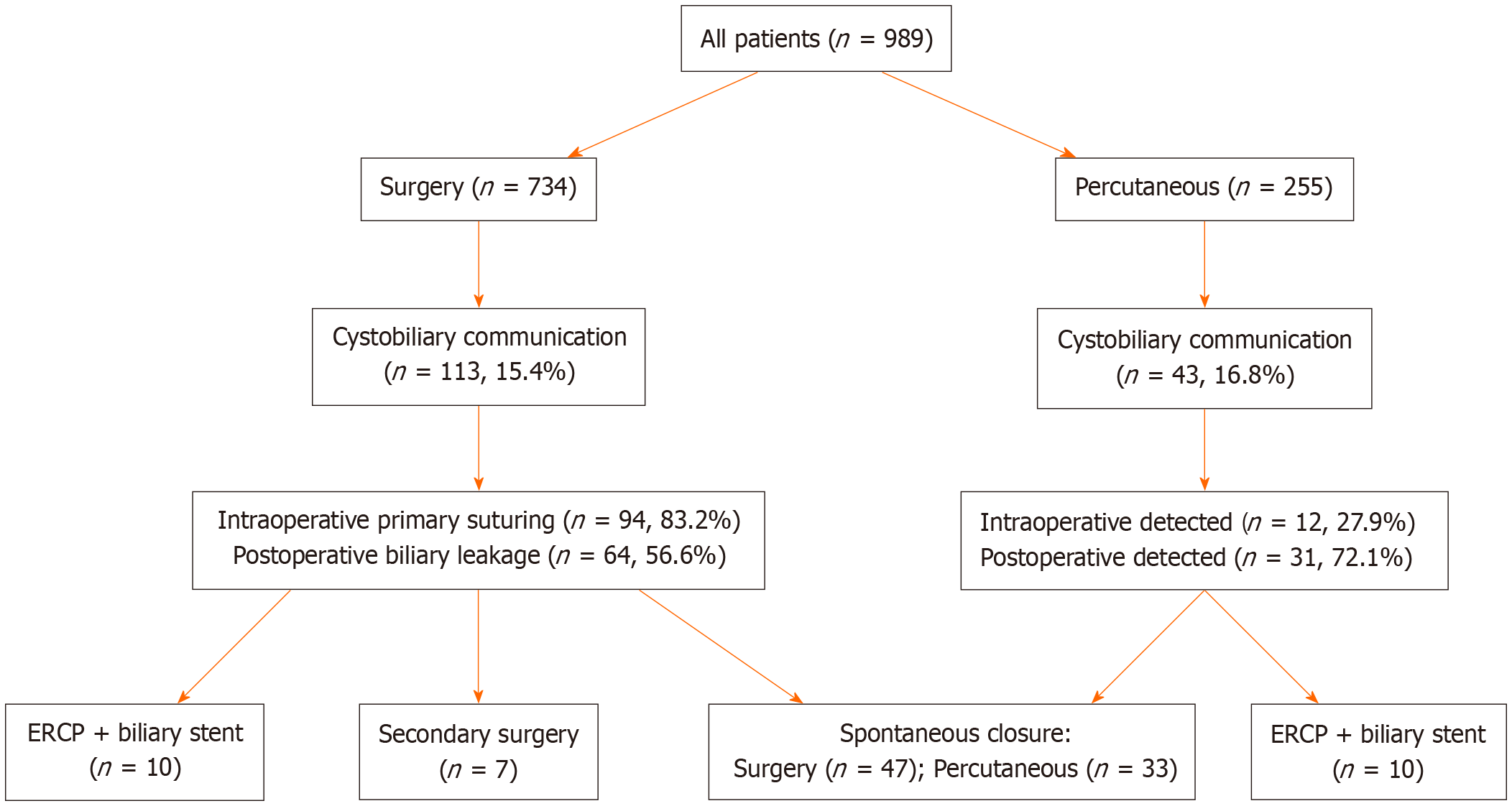
Figure 3 Management of patients with cystobiliary fistulas.
ERCP: Endoscopic retrograde cholangiopancreatography.
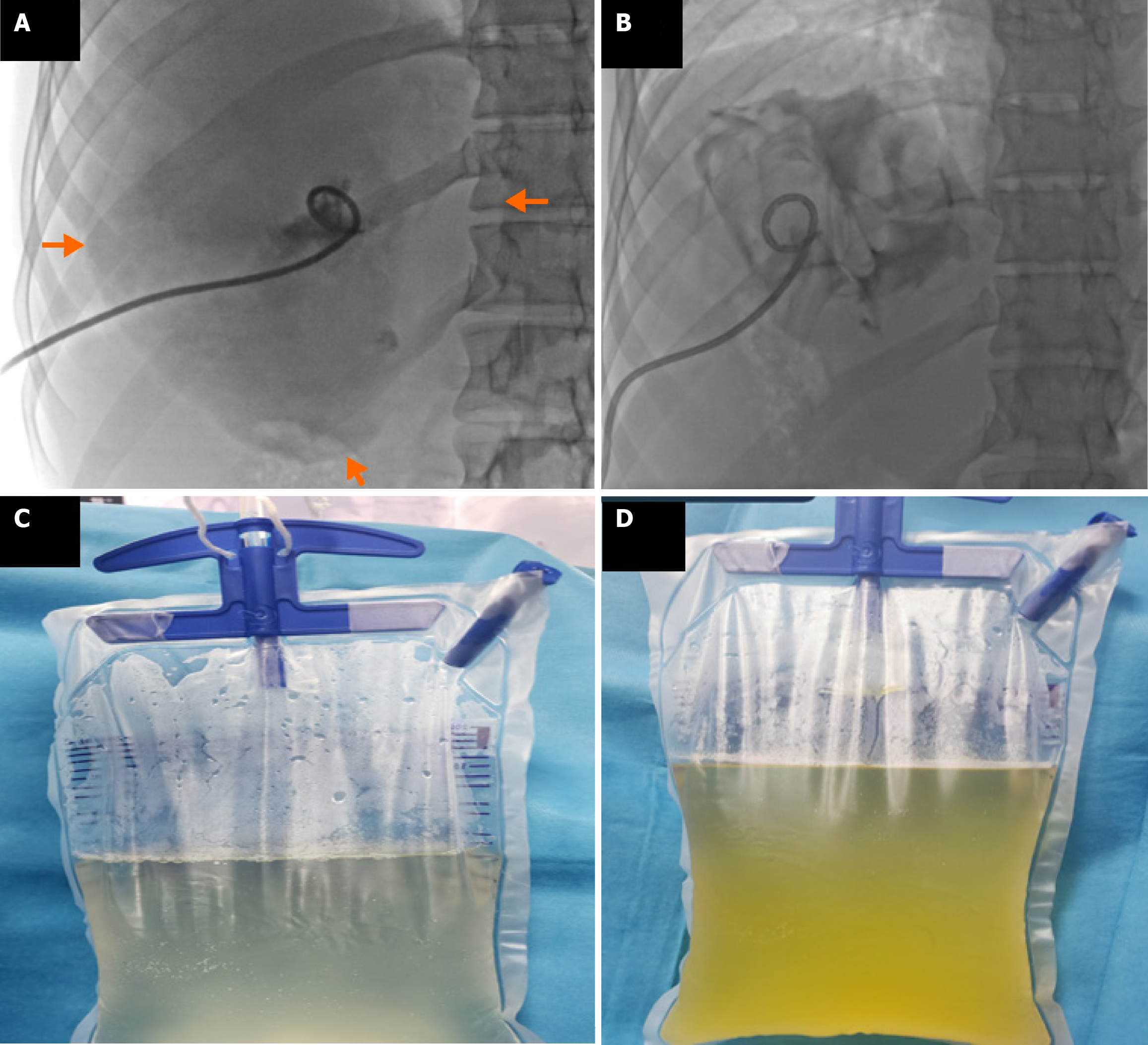
Figure 4 Fluoroscopy and cyst fluid findings during percutaneous treatment of a 29-year-old male with a giant cystic echinococcosis 1 liver cyst (volume: 2318 mL).
A and B: Fluoroscopy showing catheter placement and drainage of cyst contents with germinative membrane; C and D: Fluid initially clear, later bilious due to opening of occult bile ducts.
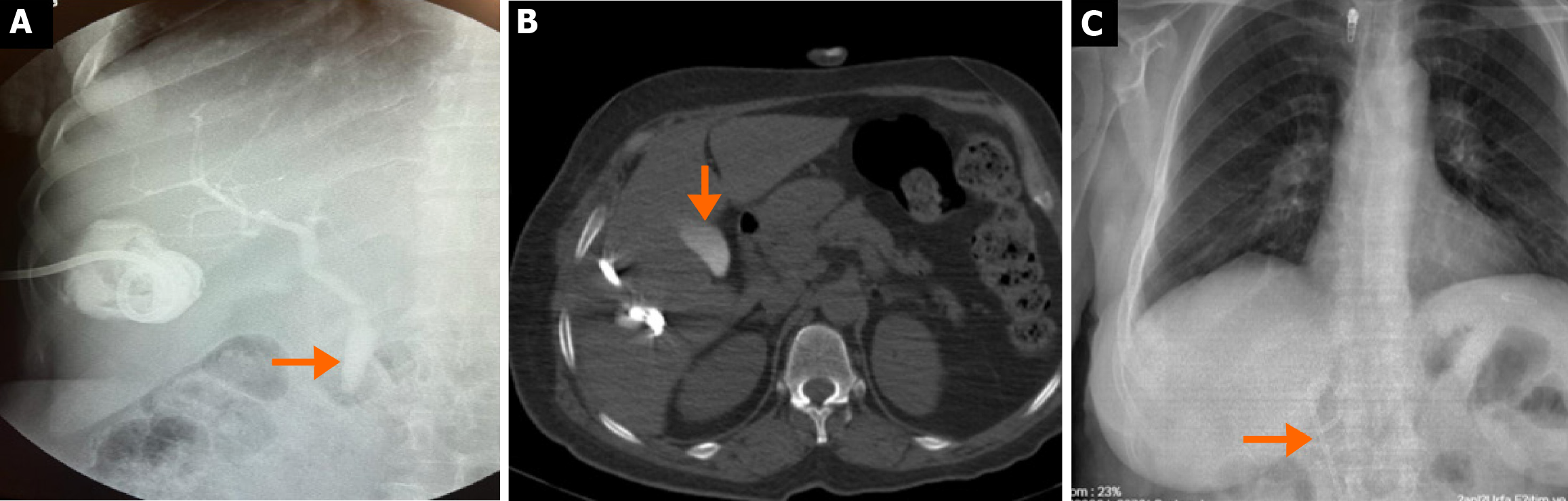
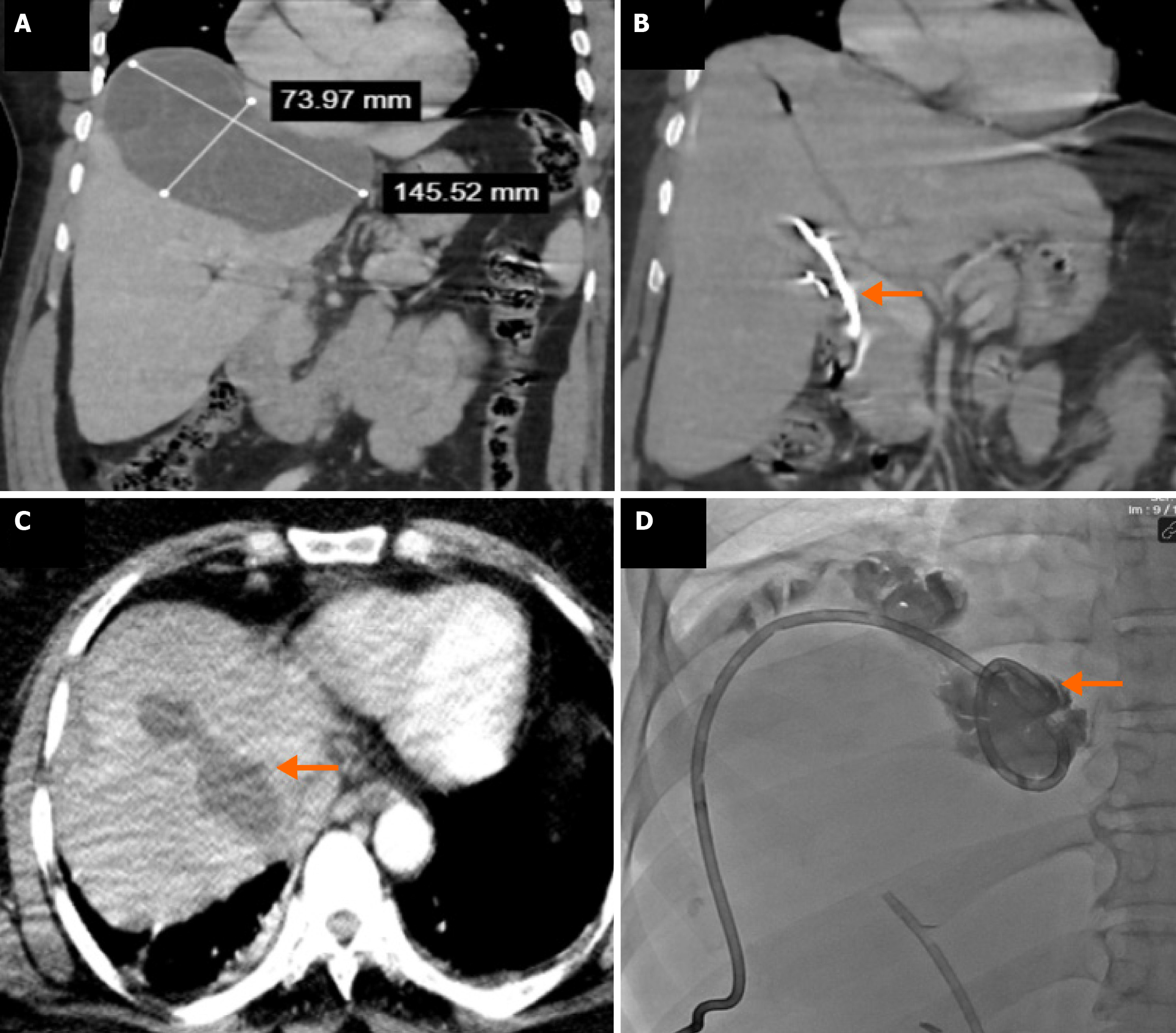
Figure 5 Images of a 54-year-old female patient with cystobiliary fistula development.
A: The cystography image of the patient with the presence of bile in drainage fluid on the second day after percutaneous treatment, shows that the contrast medium having passed into the biliary tract (arrow) and the presence of a cystobiliary fistula; B: Computed tomography image taken on the third day shows that opaque material has accumulated in the gallbladder (arrow); C: Due to increased fistula flow, papillotomy and common bile duct stenting (arrow) were performed.
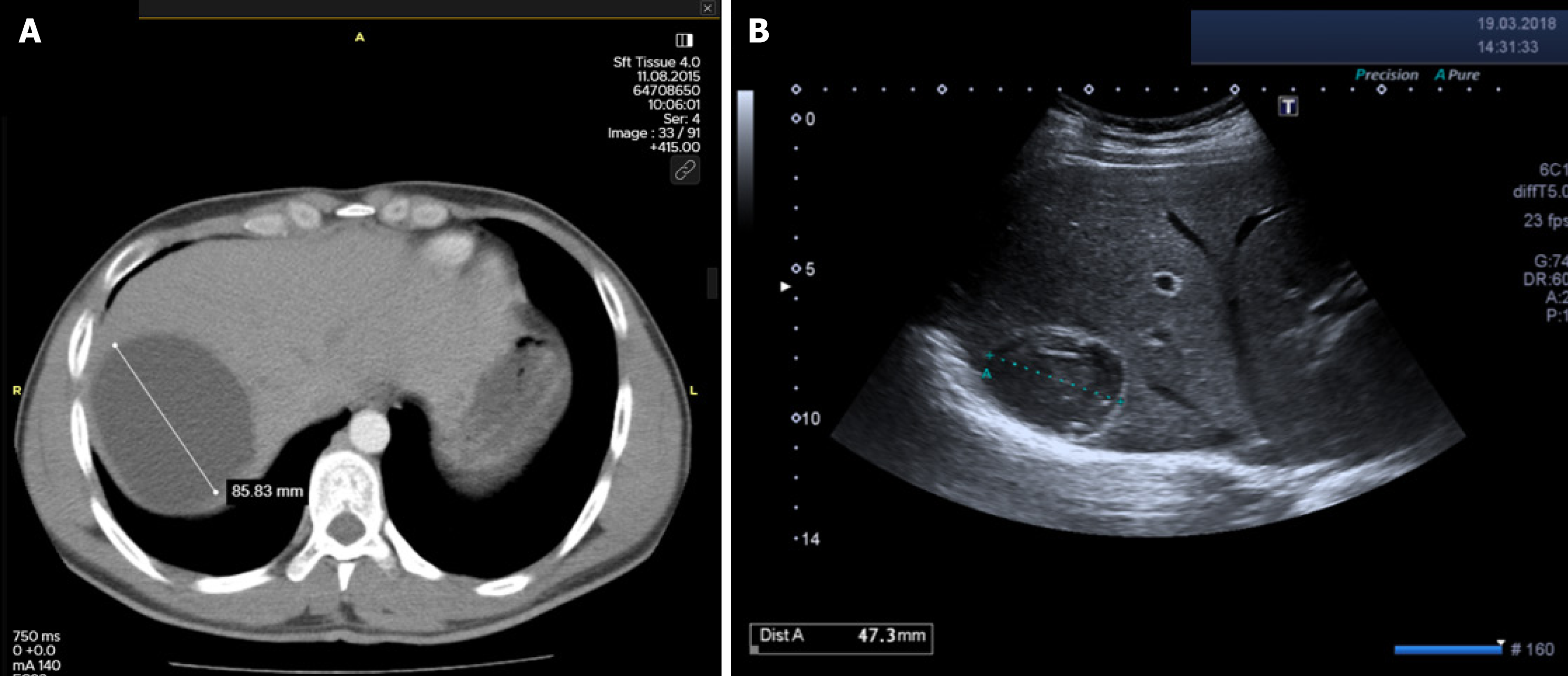
Figure 6 Radiological images of a 21-year-old male patient with a cystic echinococcosis 1 liver cyst.
A: Abdominal computed tomography image shows an untreated cystic echinococcosis 1 cyst of 85 mm in diameter located in the right lobe of the liver; B: Ultrasound image at 30 months after percutaneous treatment shows that the cyst is inactive, solidified, and reduced in size (Paired-Samples T test, P < 0.001, volumetric reduction rate: 83.6%).
Figure 7 Pre- and postoperative computed tomography and fluoroscopy images of a 40-year-old female patient with a cystic echi
- Citation: Tahtabasi M, Kaya E, Yalcin M, Kaya V. Percutaneous vs surgical management of World Health Organization cystic echinococcosis 1 and 3a liver hydatid cysts. World J Gastroenterol 2026; 32(3): 114226
- URL: https://www.wjgnet.com/1007-9327/full/v32/i3/114226.htm
- DOI: https://dx.doi.org/10.3748/wjg.v32.i3.114226