©The Author(s) 2025.
World J Gastroenterol. Feb 28, 2025; 31(8): 99036
Published online Feb 28, 2025. doi: 10.3748/wjg.v31.i8.99036
Published online Feb 28, 2025. doi: 10.3748/wjg.v31.i8.99036
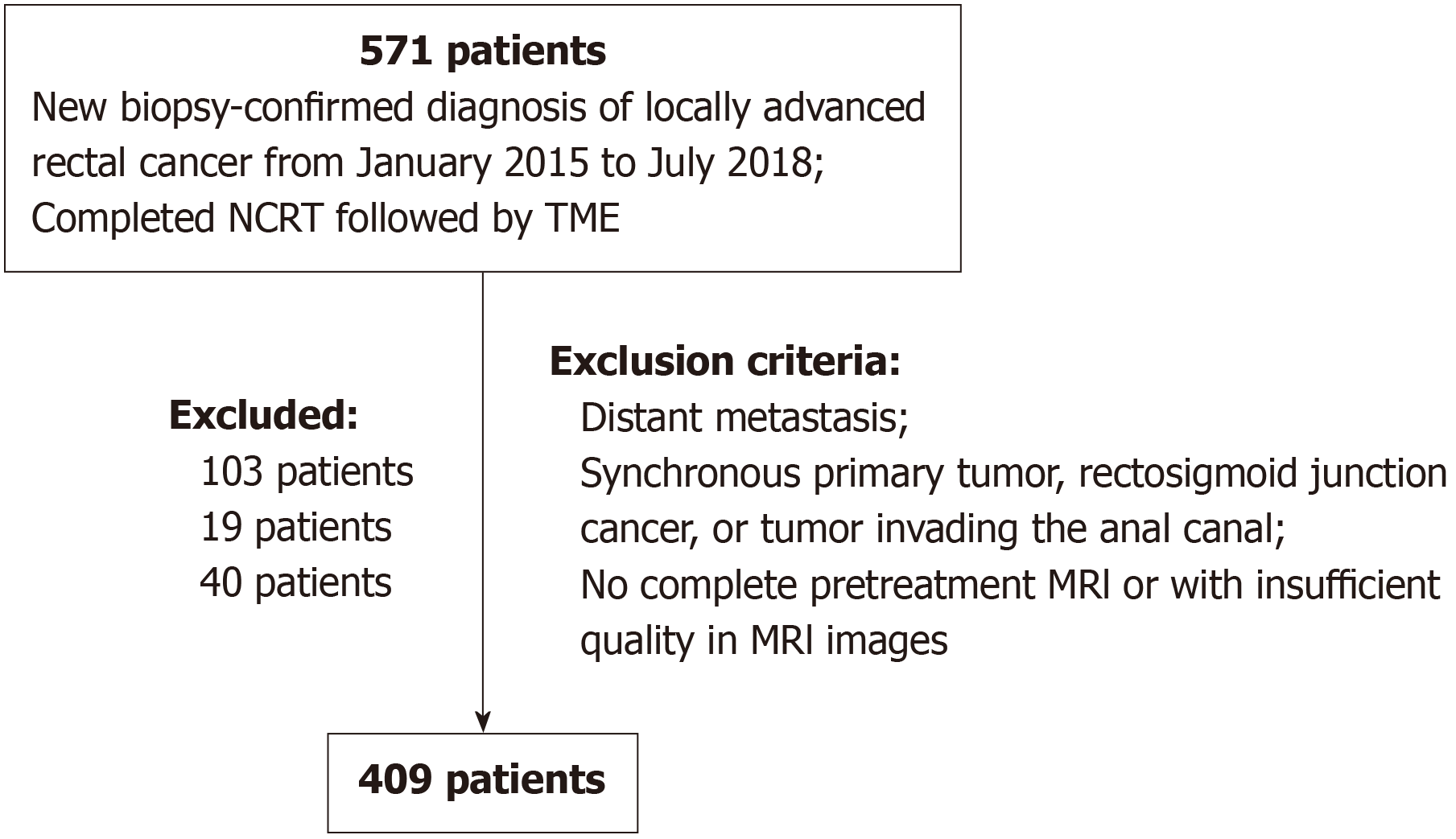
Figure 1 Patient-selection flow diagram.
MRI: Magnetic resonance imaging; NCRT: Neoadjuvant chemoradiotherapy; TME: Total mesorectal excision.
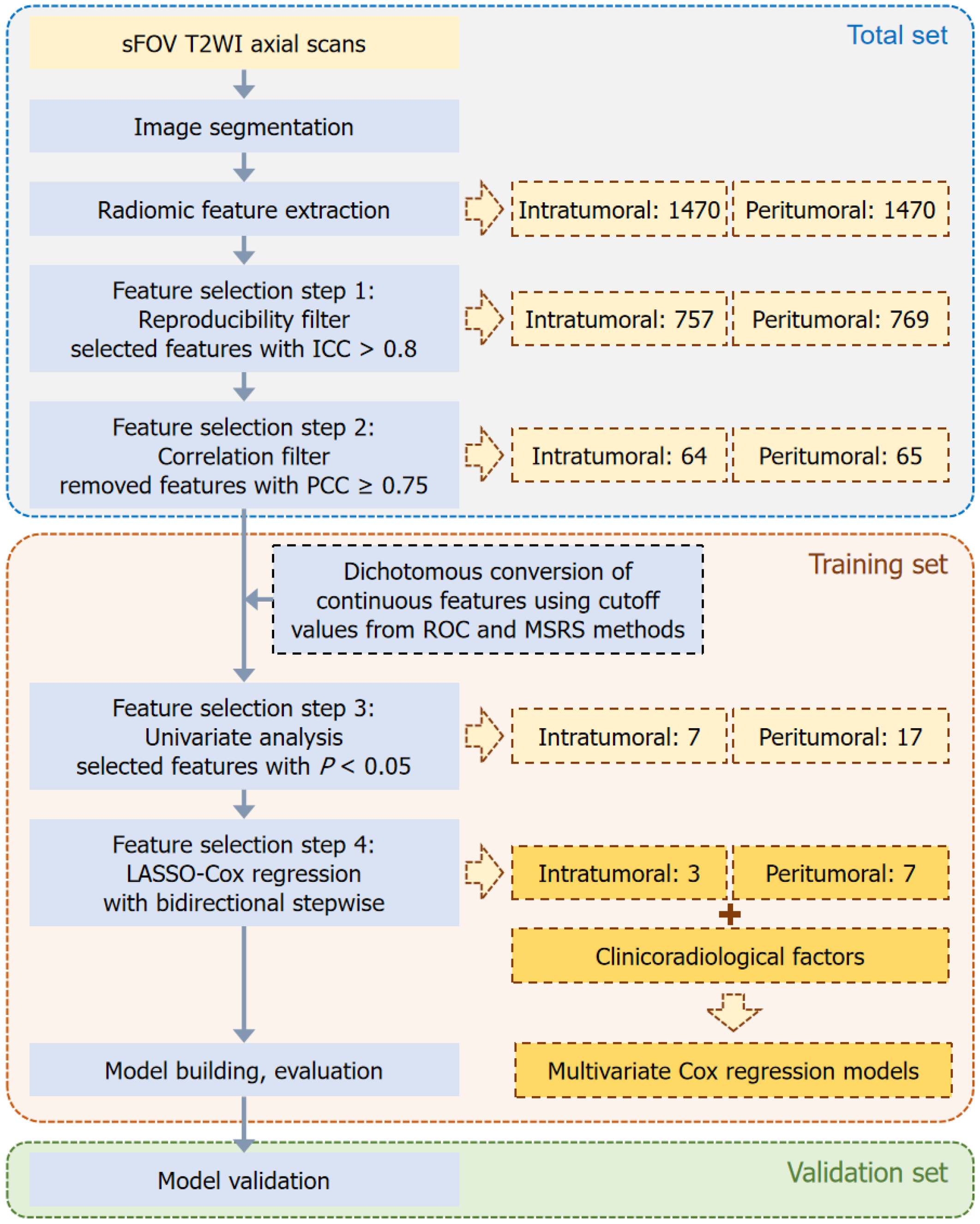
Figure 2 Radiomics workflow.
ICC: Intra-class correlation coefficient; LASSO: Least absolute shrinkage and selection operator; MSRS: Maximum selected rank statistic; PCC: Pearson’s correlation coefficient; ROC: Receiver operating characteristic; sFOV: Small-field-of-view; T2WI: T2-weighted imaging.
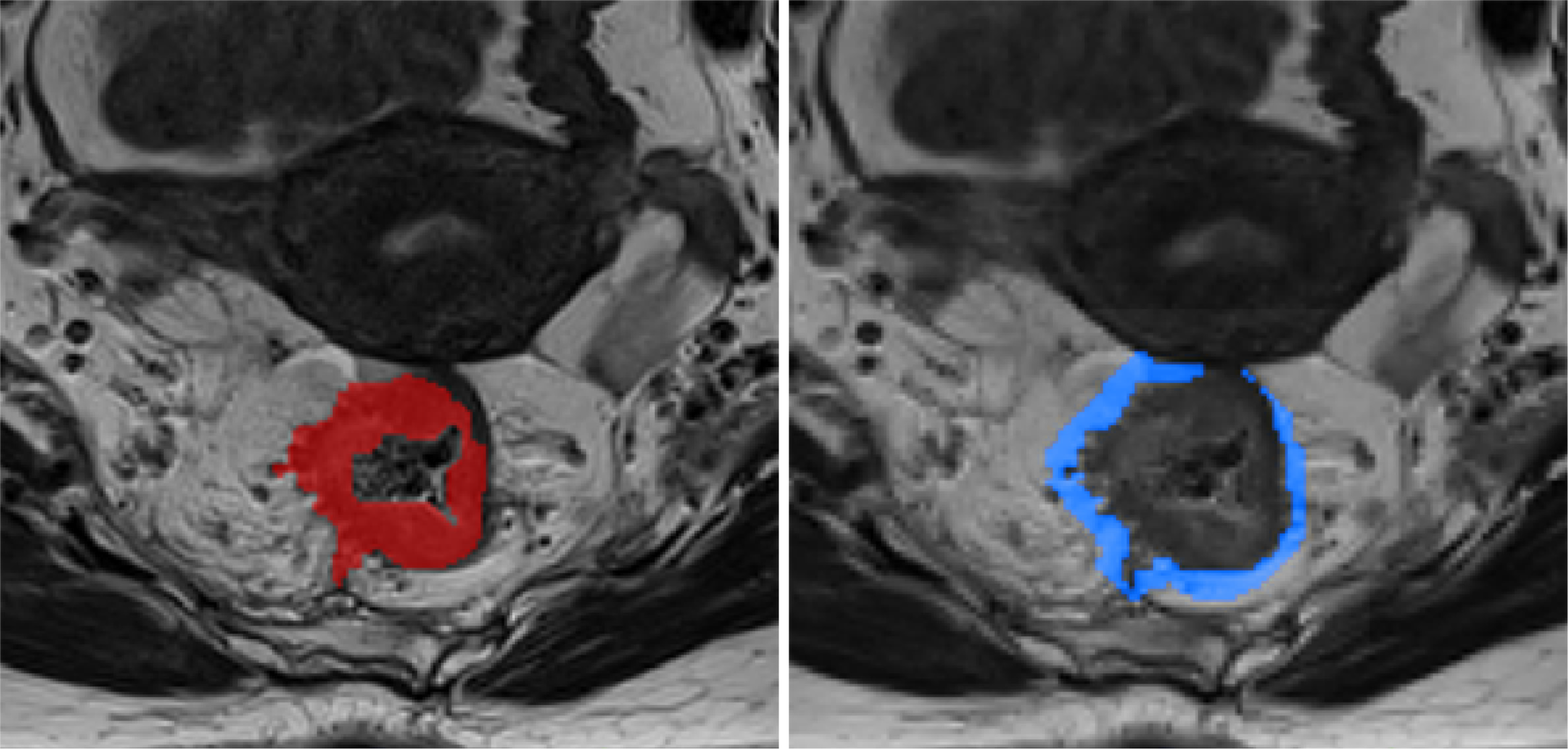
Figure 3 Example of intratumoral and peritumoral segmentation.
The intratumoral region of interest (ROI) (left, red) is manually delineated, while the peritumoral ROI (right, blue) is automatically generated. On axial high-resolution small-field-of-view T2-weighted imaging slices, the intratumoral ROI is meticulously delineated to cover the entire rectal tumor, whereas the tube ROI is drawn to encompass both the rectal tube area and tumor. Subsequently, the peritumoral ROI, representing the area surrounding the tumor, is automatically generated by the overlapping region resulting from a 5-mm dilation of both the intratumoral ROI and tube ROI.
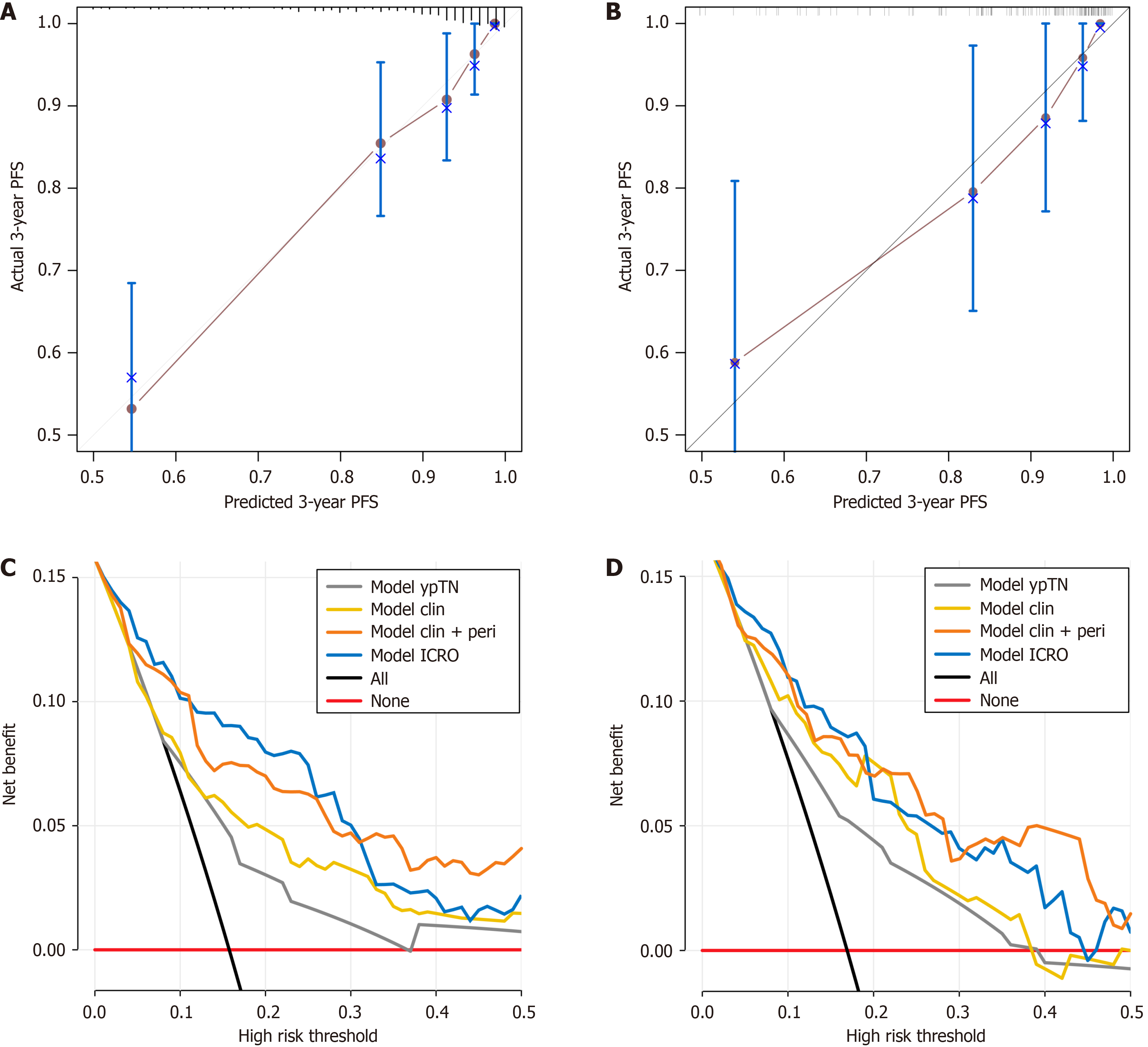
Figure 4 Calibration and decision curves of the prognostic models.
Calibration curves of integrated clinical-radiological-omics model (ModelICRO) showing a robust calibration between the predicted 3-year progression-free survival (X-axis) and the actual 3-year progression-free survival (Y-axis). A: In the training; B: Validation sets; Decision curves of model based on the pathological T stage and pathological N stage (grey line), model based on body mass index, pathological N stage, tumor regression grade, and mesorectal fascia status (Modelclin) (yellow line), Modelclin+peri (orange line), and ModelICRO (blue line) showing the net benefit across a range of threshold probabilities; C: In the training; D: Validation sets. ModelICRO shows the highest net benefit across most threshold probabilities. ICRO: Integrated clinical-radiological-omics; Clin: Clinicoradiological; PFS: Progression-free survival; Intra: Intratumoral; peri: Peritumoral; ypTN: Pathological T and N stages after neoadjuvant chemoradiotherapy.
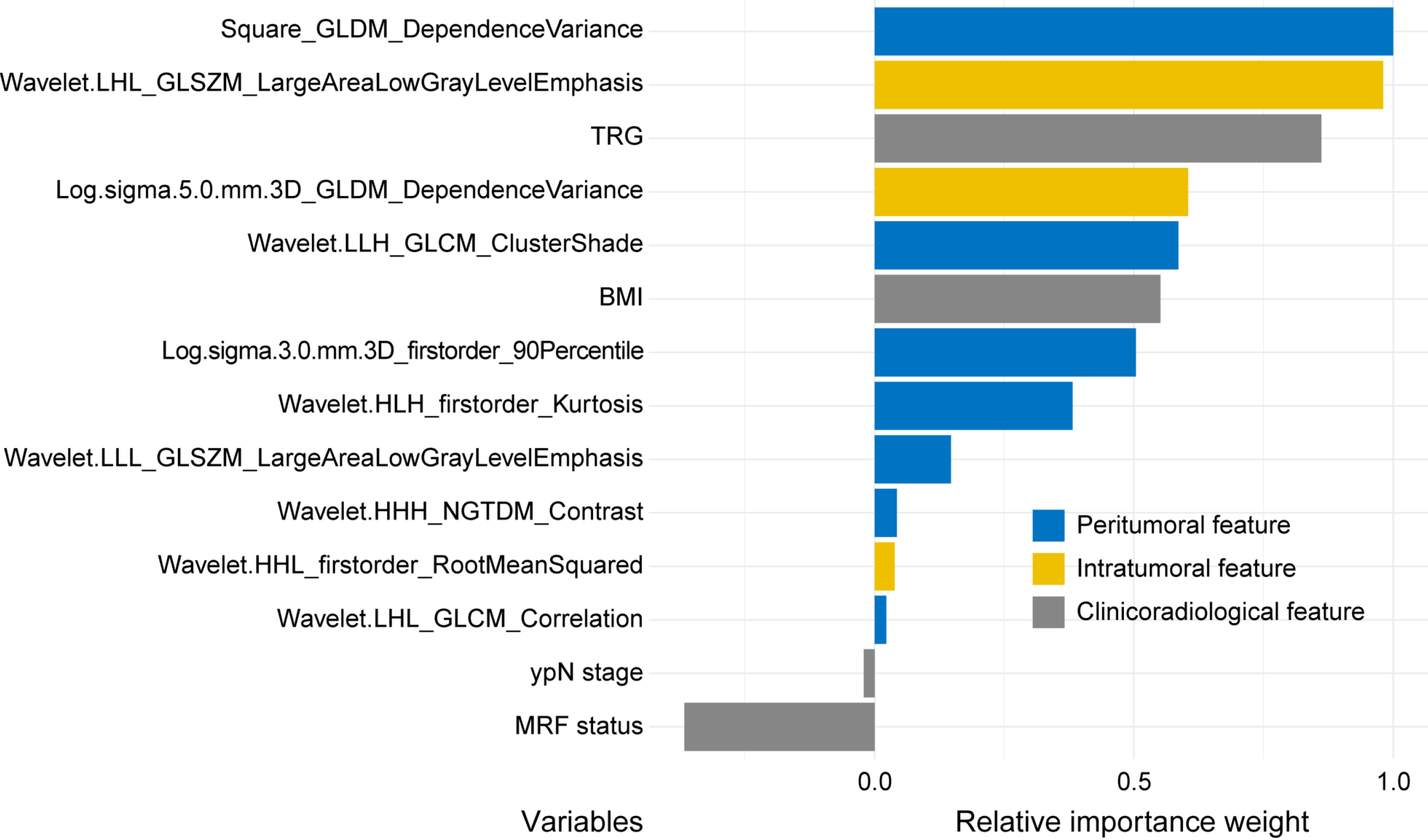
Figure 5 Relative importance weight of variables in integrated clinical-radiological-omics model.
The relative importance weight of a variable was calculated using the permutation feature importance by measuring the change in the model’s C-index after random shuffling of each feature value, with the importance scaled relative to the maximum observed change. BMI: Body mass index; GLCM: Grey level co-occurrence matrix; GLDM: Grey level dependence matrix; GLSZM: Grey level size zone matrix; HHH: High-high-high; HHL: High-high-low; HLH: High-low-high; LHL: Low-high-low; LLH: Low-low-high; LLL: Low-low-low; MRF: Mesorectal fascia; NGTDM: Neighboring grey tone difference matrix; TRG: Tumor regression grade; ypN stage: Pathological N stage after neoadjuvant chemoradiotherapy.
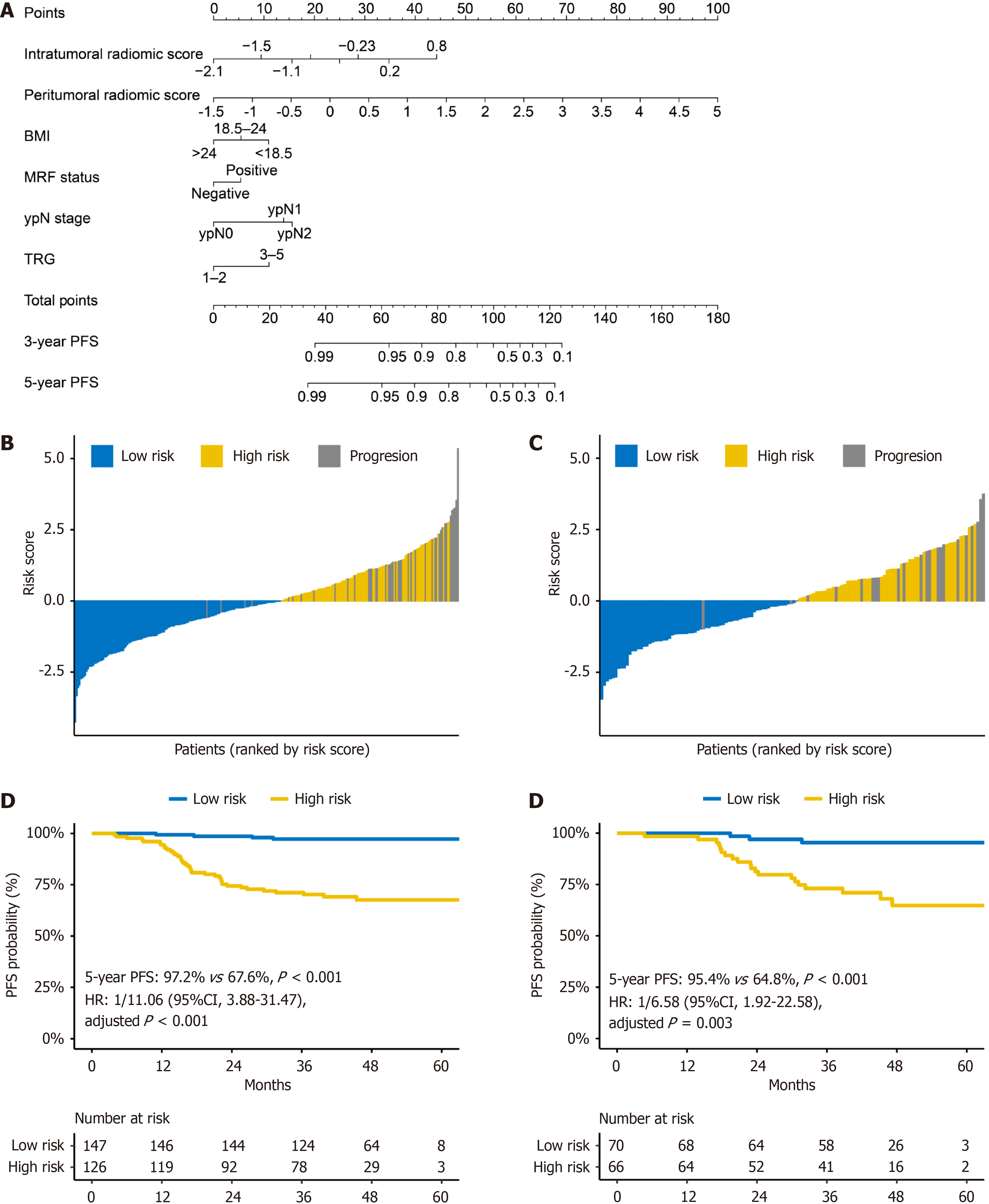
Figure 6 Nomogram, risk score, and survival analysis using the comprehensive model.
A: Nomogram of the integrated clinical-radiological-omics model for predicting 3-year progression-free survival (PFS); The progression status, risk scores, and risk stratification for each patient; B: In the training; C: Validation sets. The Kaplan-Meier survival curves for PFS for patients in the high- and low-risk groups; D: In the training; E: Validation sets. BMI: Body mass index; CI: Confidence interval; PFS: Progression-free survival; HR: Hazard ratio; MRF: Mesorectal fascia; TRG: Tumor regression grade; ypN stage: Pathological N stage after neoadjuvant chemoradiotherapy.
- Citation: Liang ZY, Yu ML, Yang H, Li HJ, Xie H, Cui CY, Zhang WJ, Luo C, Cai PQ, Lin XF, Liu KF, Xiong L, Liu LZ, Chen BY. Beyond the tumor region: Peritumoral radiomics enhances prognostic accuracy in locally advanced rectal cancer. World J Gastroenterol 2025; 31(8): 99036
- URL: https://www.wjgnet.com/1007-9327/full/v31/i8/99036.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i8.99036