©The Author(s) 2025.
World J Gastroenterol. Jul 14, 2025; 31(26): 108375
Published online Jul 14, 2025. doi: 10.3748/wjg.v31.i26.108375
Published online Jul 14, 2025. doi: 10.3748/wjg.v31.i26.108375
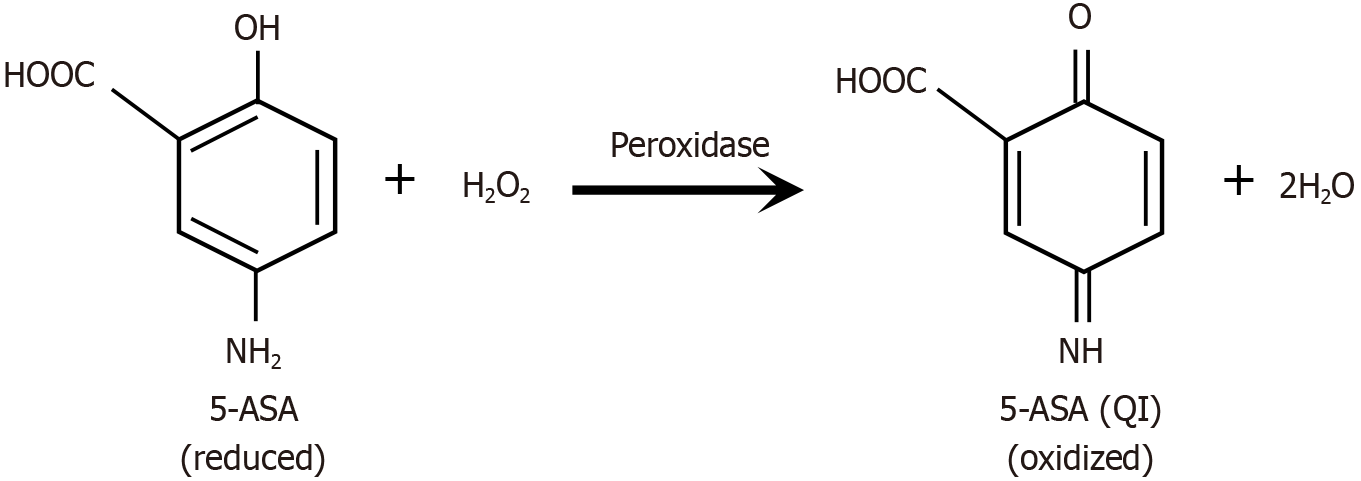
Figure 1 The redox-mediated reaction between 5-aminosalicylic acid, functioning as a reducing agent, and hydrogen peroxide, an oxidizing agent, involves the transfer of electrons.
In this process, a single molecule of reduced 5-aminosalicylic acid (5-ASA) donates two electrons, accompanied by two protons, to reduce one molecule of hydrogen peroxide into two molecules of water. In the process, 5-ASA is oxidized to the corresponding 5-ASA quinone imine. The reaction is spontaneous but enhanced by peroxidase enzymes found in the inflammatory field or colonic bacteria. 5-ASA: 5-aminosalicylic acid; H2O2: Hydrogen peroxide; H2O: Water; QI: Quinone imine.
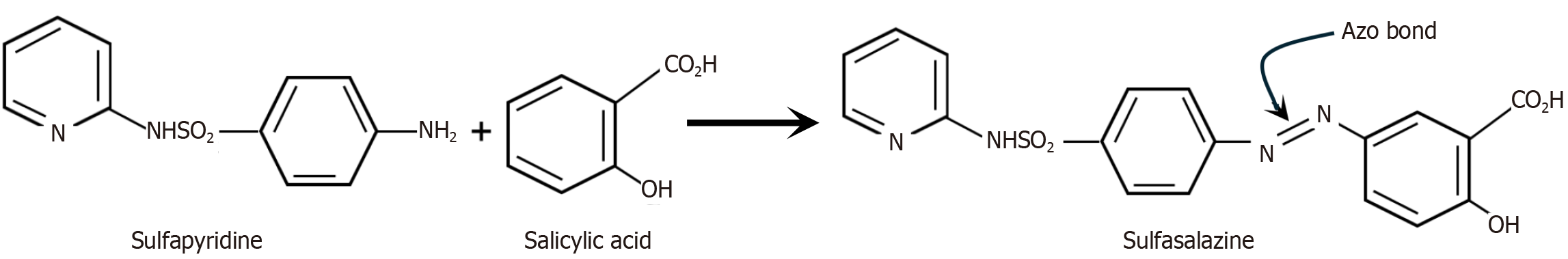
Figure 2 The reaction of the antibiotic sulfapyridine with salicylic acid to create sulfasalazine.
The sulfonamide antibiotic sulfapyridine was chemically combined with salicylic acid to synthesize the prodrug sulfasalazine. This synthesis involved the formation of an azo bond, which linked the two molecules into a single compound, sulfasalazine. Synthesis of the larger molecule sulfasalazine, and the incorporation of the azo bond proved to be pivotal in ensuring the clinical efficacy of sulfasalazine in the treatment of ulcerative colitis.
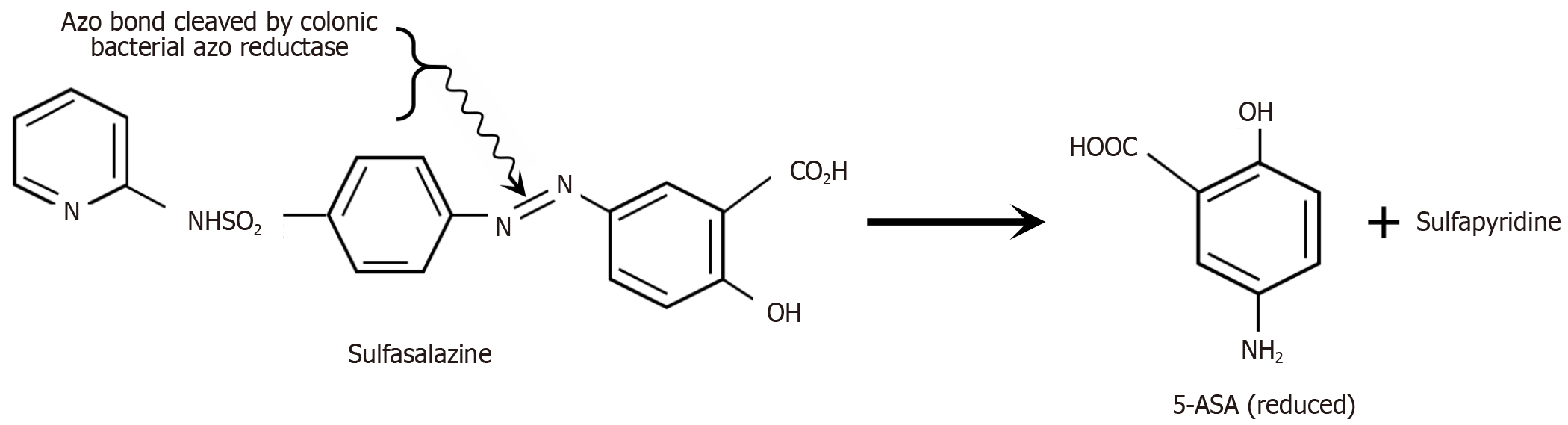
Figure 3 The reduction of the azo bond in sulfasalazine produces 5-aminosalicylic acid and sulfapyridine.
While unconjugated 5-aminosalicylic acid (5-ASA) is predominantly absorbed in the small intestine before it can reach the colon, sulfasalazine largely remains unabsorbed during its transit through the small intestine. Upon reaching the colon, bacterial azo reductases reduce the azo bond, releasing free reduced 5-ASA and sulfapyridine. This reduction reaction introduces an amino group to the No. 5 carbon in the aromatic ring of salicylic acid, resulting in the formation of reduced 5-ASA. Reduction of the azo bond enhances the electron density of the resulting 5-ASA, enabling it to function as a reducing agent and effectively neutralize hydrogen peroxide in the colonic lumen. 5-ASA: 5-aminosalicylic acid.
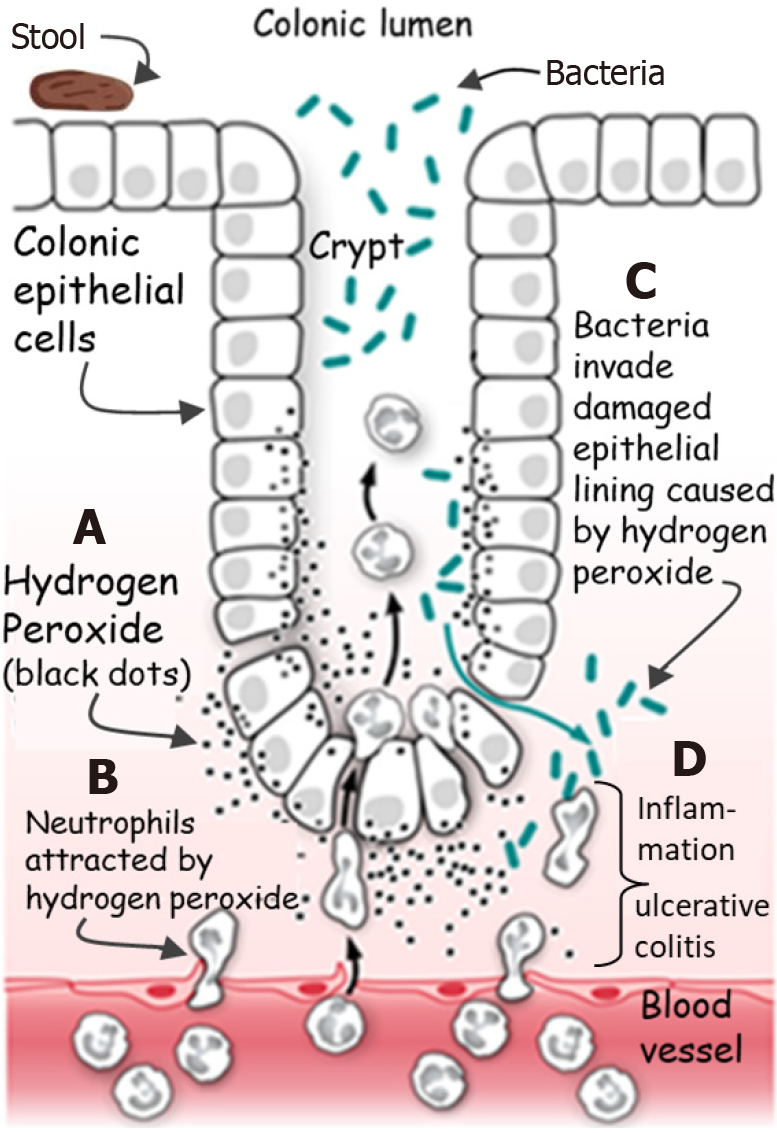
Figure 4 Evidence-based pathogenesis of ulcerative colitis.
A: Hydrogen peroxide (H2O2) diffuses from colonic epithelial cells into the extracellular space and lamina propria; B: The neutrophilic chemotactic effect of H2O2 attracts neutrophils into the colonic epithelium; C: H2O2 disintegration of tight junctional proteins facilitates bacterial invasion into the sub-epithelial tissues; D: The ensuing mucosal inflammation leads to ulcerative colitis.
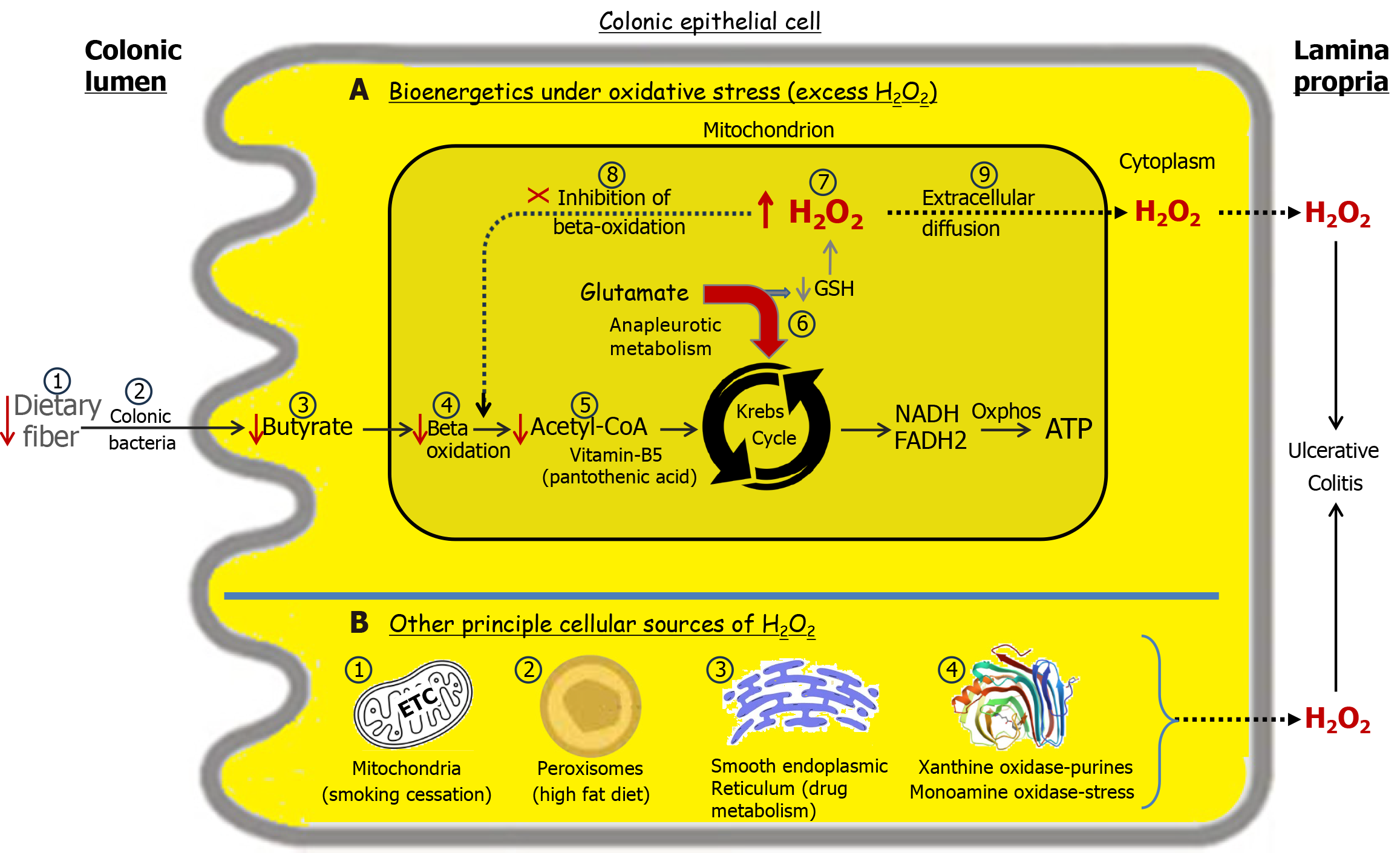
Figure 5 Transduction of environmental stimuli increases cellular hydrogen peroxide levels, elevating the risk of ulcerative colitis[27].
Normal energy flux in the colon begins with luminal soluble fiber, which is fermented by bacteria into n-butyrate, a key short-chain fatty acid. Butyrate is absorbed by colonic epithelial cells, where it undergoes beta-oxidation, generating acetyl-CoA. Subsequently, acetyl-CoA enters the Krebs cycle, producing the reducing equivalents NADH, nicotinamide adenine dinucleotide (reduced form) and FADH2, flavin adenine dinucleotide (reduced form) that drive oxidative phosphorylation to generate ATP, adenosine triphosphate. Panel A: Bioenergetics under oxidative stress. A deficiency in dietary soluble fiber (A1) results in inadequate butyrate production (A3) and reduced acetyl-CoA levels (A5). To offset the energy shortfall, the Krebs cycle engages in anaplerotic metabolism of glutamate (A6)[32,33]. This redirection of glutamate for energy production compromises glutathione synthesis required for hydrogen peroxide (H2O2) neutralization leading to elevated cellular H2O2 levels (A7). With sufficient accumulation, mitochondrial H2O2 can diffuse into the cytoplasm and across the cell membrane into the lamina propria, contributing to the development of ulcerative colitis (UC) (A9). A reduction in acetyl-CoA due to deficiencies in any factors involved in its synthesis, starting with luminal fiber, can lead to elevated cellular H2O2 levels, increasing the risk of UC. This is exemplified by a deficiency of vitamin B5, required for the synthesis of coenzyme A, which leads to a colitis in pigs analogous to human UC[34]. Initially, H2O2 accumulates within mitochondria, impairing beta oxidation, and is followed by relapse weeks later[21]. This delay reflects the time needed for mitochondrial H2O2 to establish a sufficient concentration gradient for cytoplasmic and extracellular diffusion. This explains why butyrate enemas are ineffective in resolving UC as H2O2 inhibits beta oxidation (A8)[26]. Sufficient damage to the colonic microbiota (A2) may increase the risk of developing or exacerbating UC. Panel B: The source of H2O2 production is influenced by the nature of the environmental stimuli[27]. B1: Disinhibition of the mitochondrial electron transport chain following smoking cessation can result in elevated H2O2 production, contributing to the development of ulcerative colitis[35]. B2: A diet rich in fats promotes increased peroxisomal beta-oxidation of long-chain fatty acids, leading to heightened H2O2 production, which predisposes individuals to UC. B3: The metabolism of certain drugs, such as nonsteroidal anti-inflammatory drugs, via cytochrome P450 enzymes in the smooth endoplasmic reticulum generates H2O2[36], which may contribute to the onset or relapse of UC. B4: Xanthine oxidase metabolizes purines found in red meat, producing significant amounts of H2O2[37]. Monoamine oxidase-A metabolizes serotonin released by enterochromaffin cells in the colon under stress, generating significant amounts of H2O2[38]. Oxidative stressors are stimuli that increase H2O2 in the body. More than one can be present simultaneously and contribute to UC development or relapse. H2O2: Hydrogen peroxide; NADH: Nicotinamide adenine dinucleotide (reduced); FADH2: Flavin adenine dinucleotide (reduced); ATP: Adenosine triphosphate; GSH: Glutathione.
- Citation: Pravda J. Ulcerative colitis: Timeline to a cure. World J Gastroenterol 2025; 31(26): 108375
- URL: https://www.wjgnet.com/1007-9327/full/v31/i26/108375.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i26.108375