©The Author(s) 2022.
World J Gastroenterol. Feb 28, 2022; 28(8): 775-793
Published online Feb 28, 2022. doi: 10.3748/wjg.v28.i8.775
Published online Feb 28, 2022. doi: 10.3748/wjg.v28.i8.775
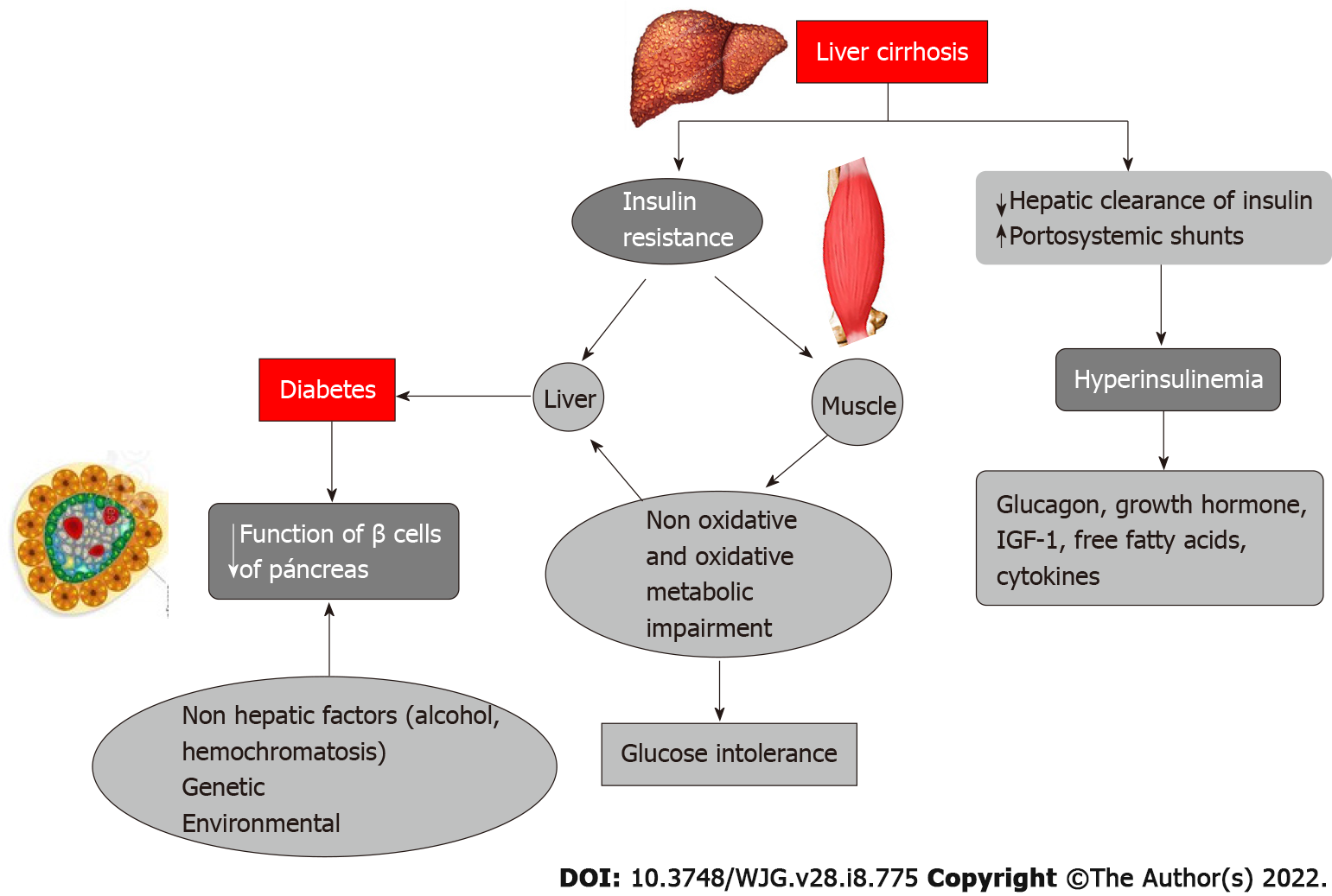
Figure 1 Pathophysiology of hepatogenous diabetes in cirrhotic liver.
Hepatogenous diabetes develops directly from insulin resistance in the liver, and indirectly from impaired glucose metabolism due to insulin resistance in muscle. Hyperinsulinemia can result from reduced insulin clearance by the damaged liver and the presence of portosystemic shunts. With progression of diabetes, there is a reduction in the sensitivity of pancreatic b cells due to glucotoxicity, and reduced production of insulin. IGF: Insulin-like growth factor.
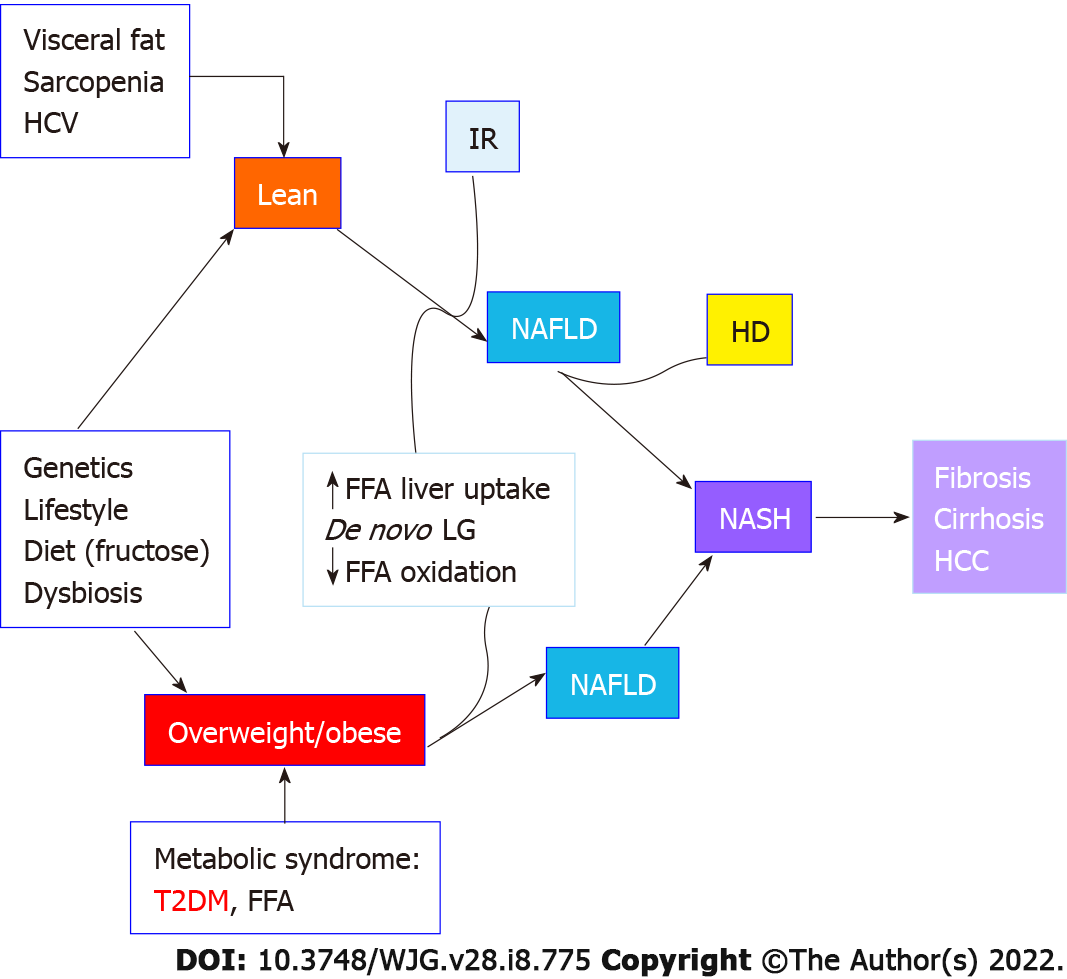
Figure 2 The pathophysiological relationship between diabetes mellitus and nonalcoholic fatty liver disease.
This is bidirectional: On the one hand, type 2 diabetes mellitus (T2DM) is a strong risk factor (alone or as part of metabolic syndrome) for nonalcoholic fatty liver disease (NAFLD), liver cirrhosis and hepatocellular carcinoma. On the other hand, NAFLD in the absence of metabolic disorders is a risk factor for incidental DM as it has been demonstrated in lean subjects with NAFLD. In both cases genetics, [PNPLA3 rs738409 polymorphism (G allele), SREBF-2 rs133291 C/T polymorphism, TM6SF2 rs58542926 C>T and CETP rs12447924 and rs1259700 polymorfisms], as well as sedentary life style, diet and dysbiosis may also play an important role. HCV: Hepatitis C virus; IR: Insulin resistance; NAFLD: Nonalcoholic fatty liver disease; HD: Hepatogenous diabetes; FFA: Free fatty acids; LG: Lactoglobulin; T2DM: Type 2 diabetes mellitus; NASH: Non-alcoholic steatohepatitis; HCC: Hepatocellular carcinoma.
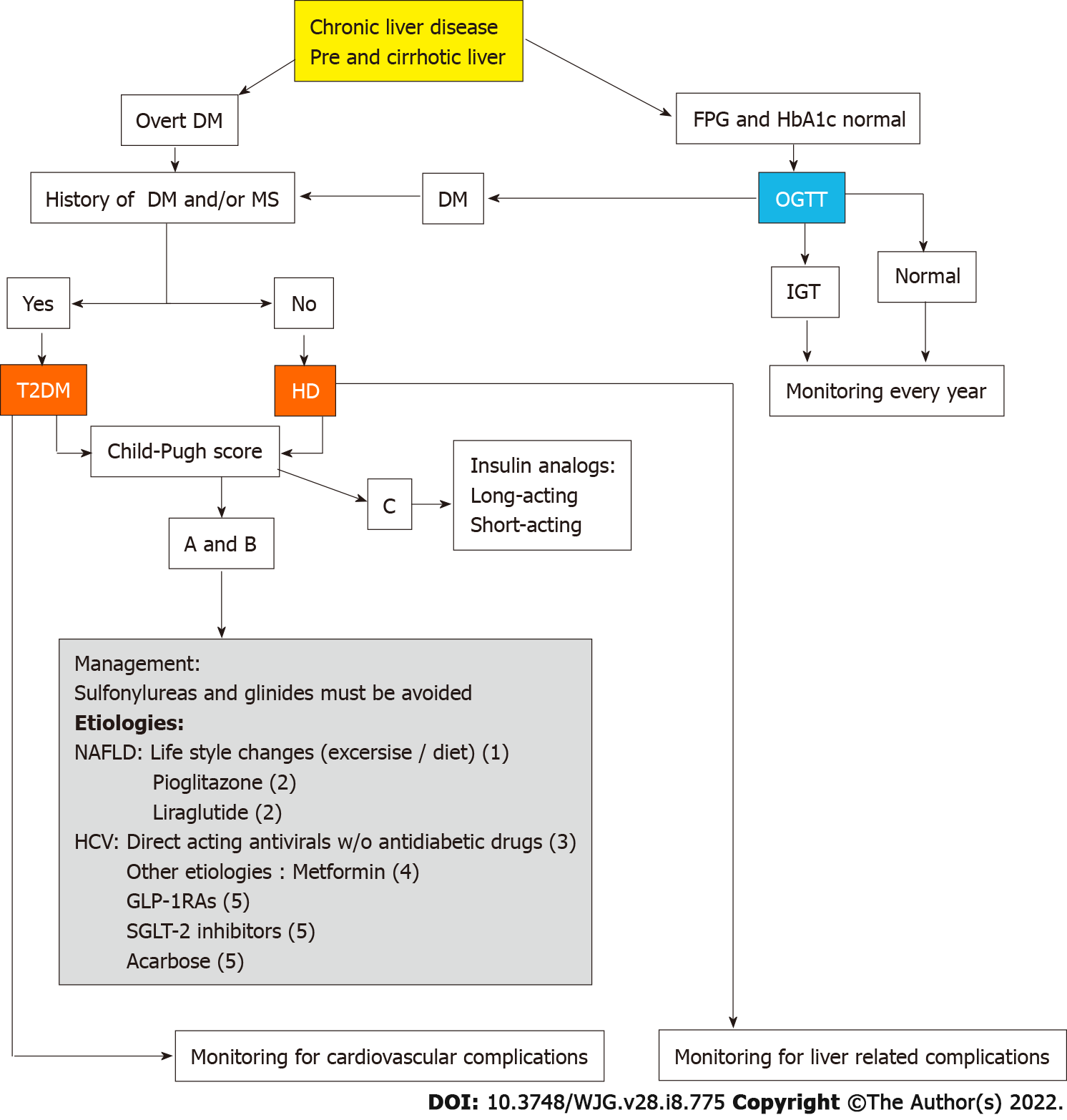
Figure 3 Algorithm for diagnosis and management of diabetes mellitus and nonalcoholic fatty liver disease based on the published evidences.
As follows: (1) This treatment has been evaluated only in nonalcoholic fatty liver disease (NAFLD); (2) These drugs have been evaluated in NAFLD showing improvement of non-alcoholic steatohepatitis and fibrosis; (3) Direct-acting antiviral have demonstrated improvement of short and long term glycemic control after hepatitis C virus eradication; (4) Long term administration of metformin has demonstrated association to significant reduction of liver related complications, hepatocellular carcinoma and mortality; and (5) GLP-1 receptor agonists and sodium-glucose co-transporter-2 inhibitor drugs have demonstrated effectiveness for glycemic control and good tolerance in liver cirrhosis patients. NAFLD: Nonalcoholic fatty liver disease; DM: Diabetes mellitus; GLP-1Ras: GLP-1 receptor agonists; SGLT-2: Sodium-glucose co-transporter-2; HCV: Hepatitis C virus; FPG: Fasting plasma glucose; HbA1c: Glycated hemoglobin; HD: Hepatogenous diabetes; MS: Metabolic syndrome; OGTT: Oral glucose tolerance test; IGT: Impaired glucose tolerance.
- Citation: García-Compeán D, Orsi E, Kumar R, Gundling F, Nishida T, Villarreal-Pérez JZ, Del Cueto-Aguilera ÁN, González-González JA, Pugliese G. Clinical implications of diabetes in chronic liver disease: Diagnosis, outcomes and management, current and future perspectives. World J Gastroenterol 2022; 28(8): 775-793
- URL: https://www.wjgnet.com/1007-9327/full/v28/i8/775.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i8.775