©The Author(s) 2021.
World J Gastroenterol. Jul 7, 2021; 27(25): 3693-3704
Published online Jul 7, 2021. doi: 10.3748/wjg.v27.i25.3693
Published online Jul 7, 2021. doi: 10.3748/wjg.v27.i25.3693
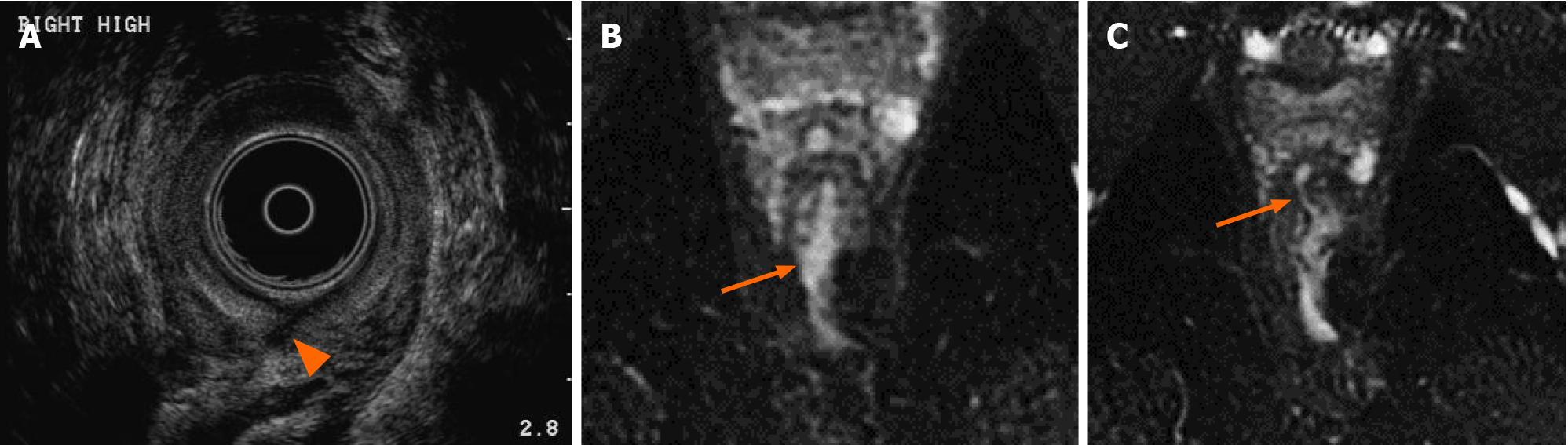
Figure 1 A 37-year-old-man with history of Crohn’s disease.
A: Transrectal ultrasound identifies a defect in the internal anal sphincter posteriorly (arrowhead); B: Axial T2 weighted, fat saturated image of the anal canal obtained 6 d later more clearly show a transsphincteric perianal fistula arising at 6 o’clock with a fluid filled sinus tract extending posteriorly to exit at the skin surface; C: Magnetic resonance imaging (MRI) image also demonstrates an additional transsphincteric fistula which arises at the 1 o’clock position extending anteriorly and communicating with a complex branching tract which also exited to the skin surface (not shown). MRI provides comprehensive multiplanar imaging of fistulizing disease, allowing visualization of the full extent of disease including supralevator disease and more complete classification of branching or complex fistulas. Additionally, post contrast sequences allow differentiation between fluid containing tracts from granulation tissue seen following healing.
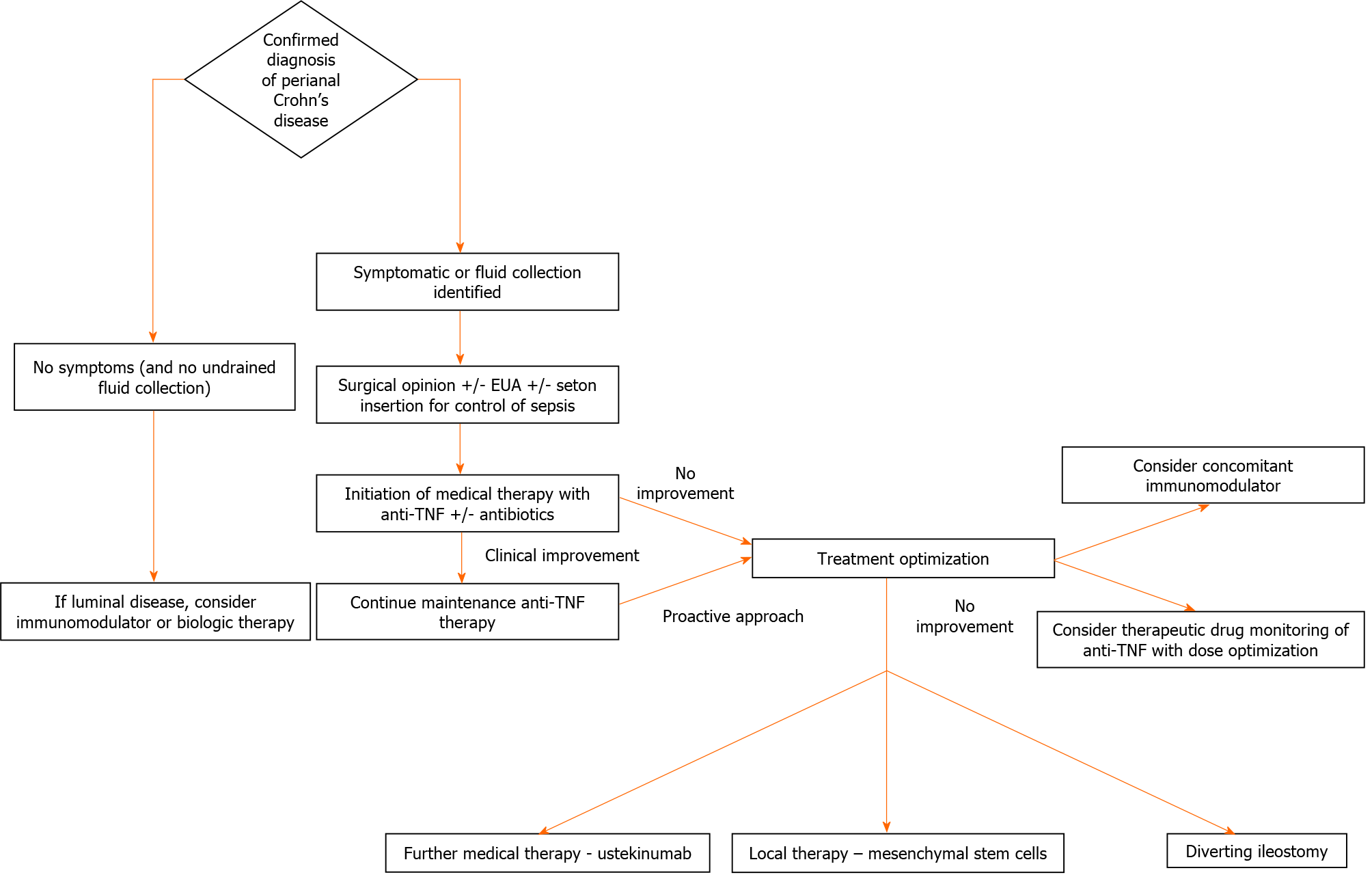
Figure 2 A suggested approach to treatment in perianal Crohn’s disease.
Anti-TNF: Anti-tumor necrosis factor; EUA: Examination under anesthesia.
- Citation: Vasudevan A, Bruining DH, Loftus EV Jr, Faubion W, Ehman EC, Raffals L. Approach to medical therapy in perianal Crohn’s disease. World J Gastroenterol 2021; 27(25): 3693-3704
- URL: https://www.wjgnet.com/1007-9327/full/v27/i25/3693.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i25.3693