Copyright
©The Author(s) 2020.
World J Gastroenterol. Apr 7, 2020; 26(13): 1427-1438
Published online Apr 7, 2020. doi: 10.3748/wjg.v26.i13.1427
Published online Apr 7, 2020. doi: 10.3748/wjg.v26.i13.1427
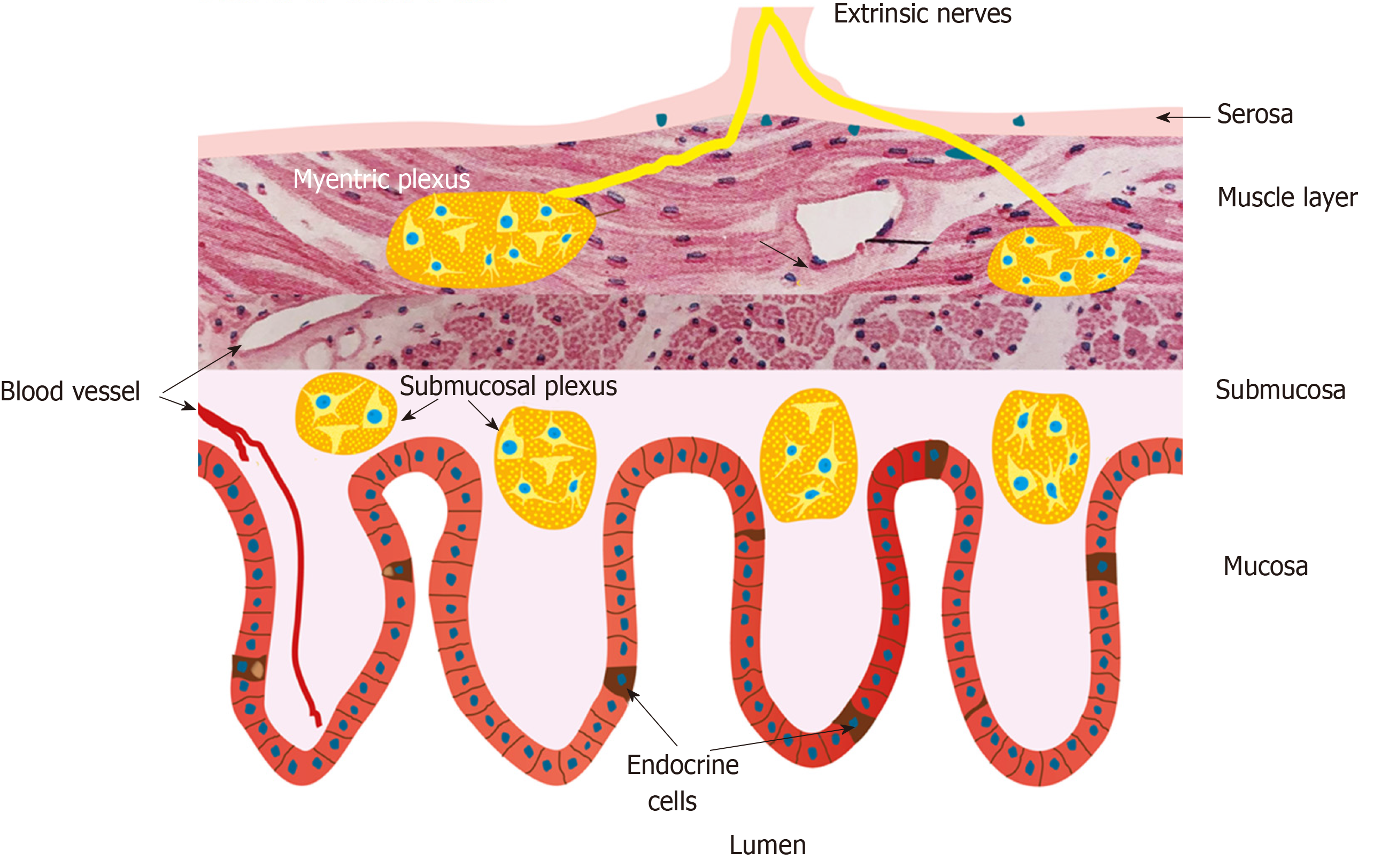
Figure 1 Schematic illustration of the enteroendocrine cells and their anatomic relation to the enteric nervous system.
The enteroendocrine cells are scattered among the epithelial cells lining the intestinal lumen. They interact and intergrade with each other’s and with enteric nervous system. Reproduced from El-Salhy et al[54] by permission of the authors and the publisher.
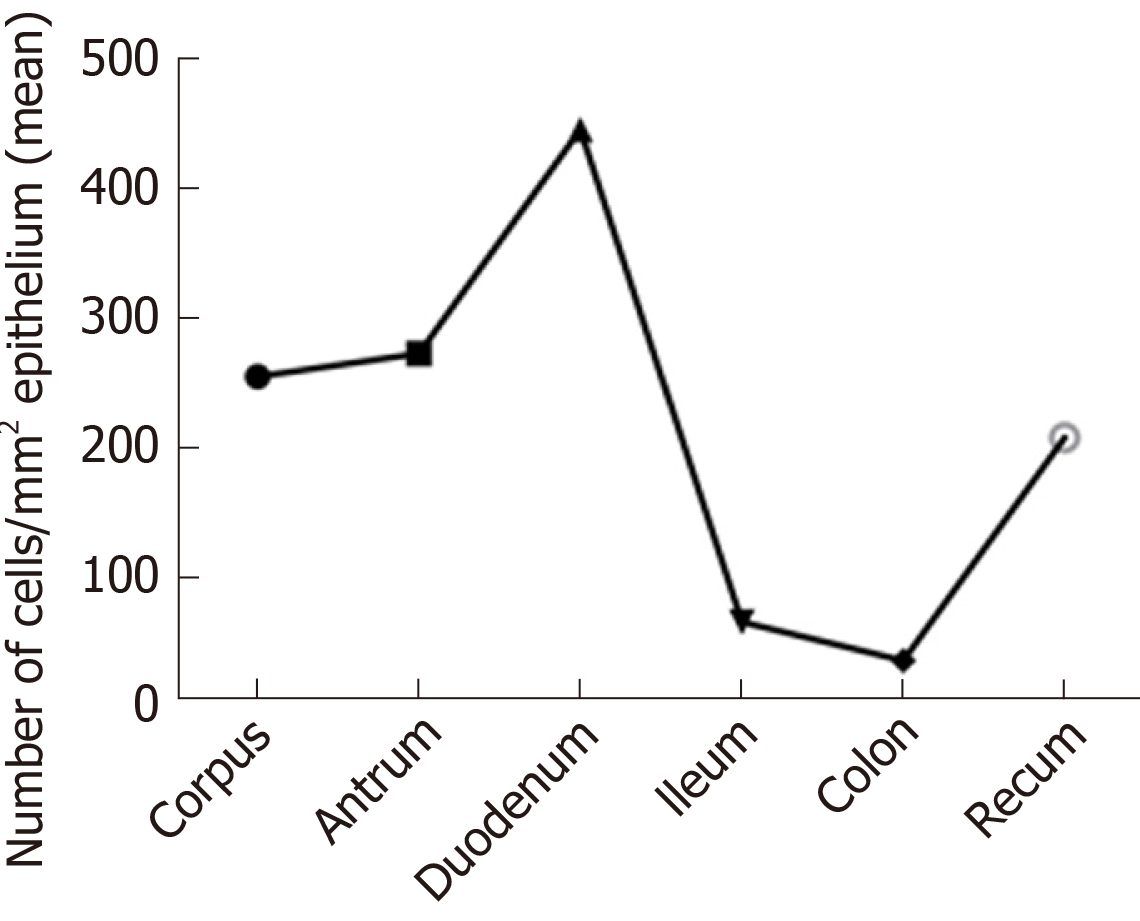
Figure 2 The density of gut endocrine cells as detected by chromogranin a immunoreactivity.
Reproduced from El-Salhy et al[25] by permission of the authors and the publisher.
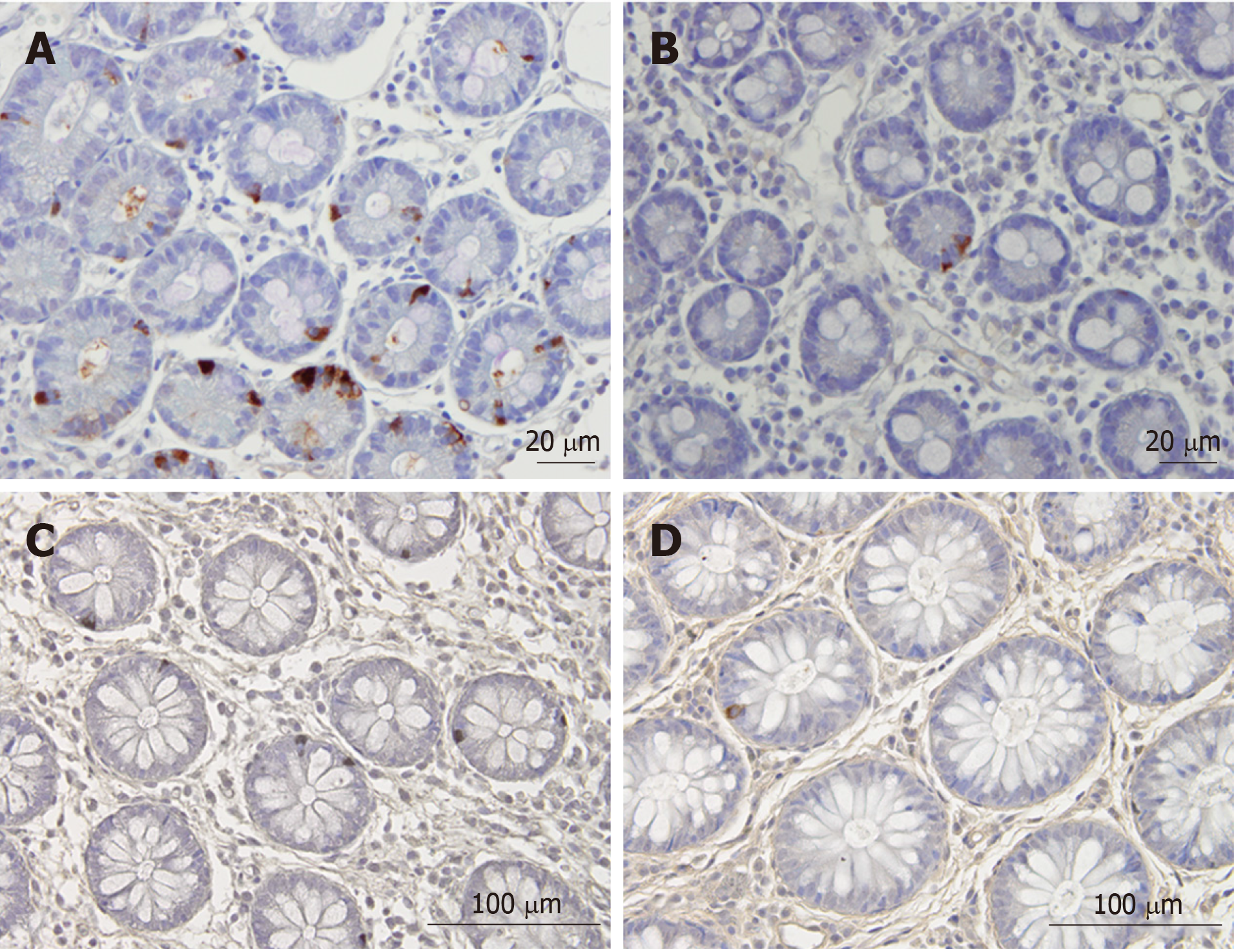
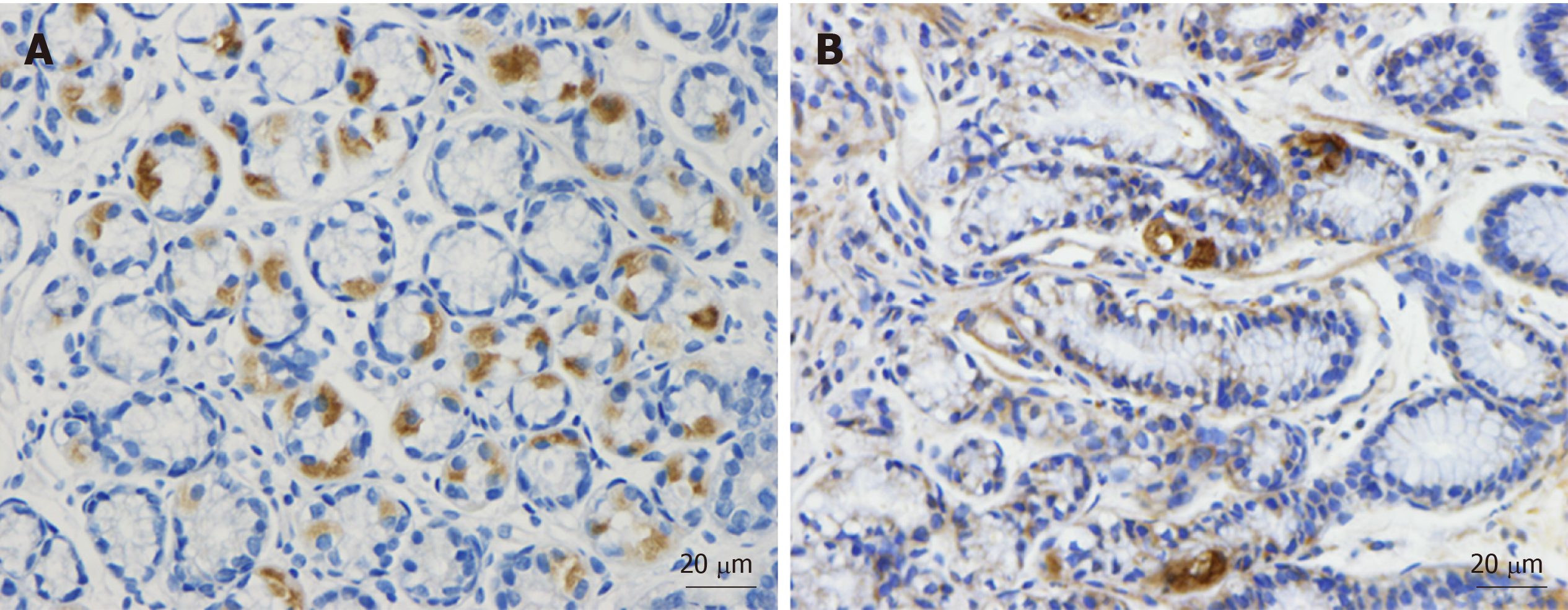
Figure 3 Chromogranin immunoreactive cells in the duodenum of a healthy subject and of a patient with irritable bowel syndrome.
A: Chromogranin immunoreactive cells in the duodenum of a healthy subject; B: Chromogranin immunoreactive cells in the duodenum of a patient with irritable bowel syndrome (IBS); C: Chromogranin A cells in the colon of a healthy control; D: Chromogranin A cells in the colon of a patient with IBS. Chromogranin A is a common marker for enteroendocrine cells. The density of Chromogranin A in the duodenum and colon of patients with IBS is lower than that of healthy subjects.
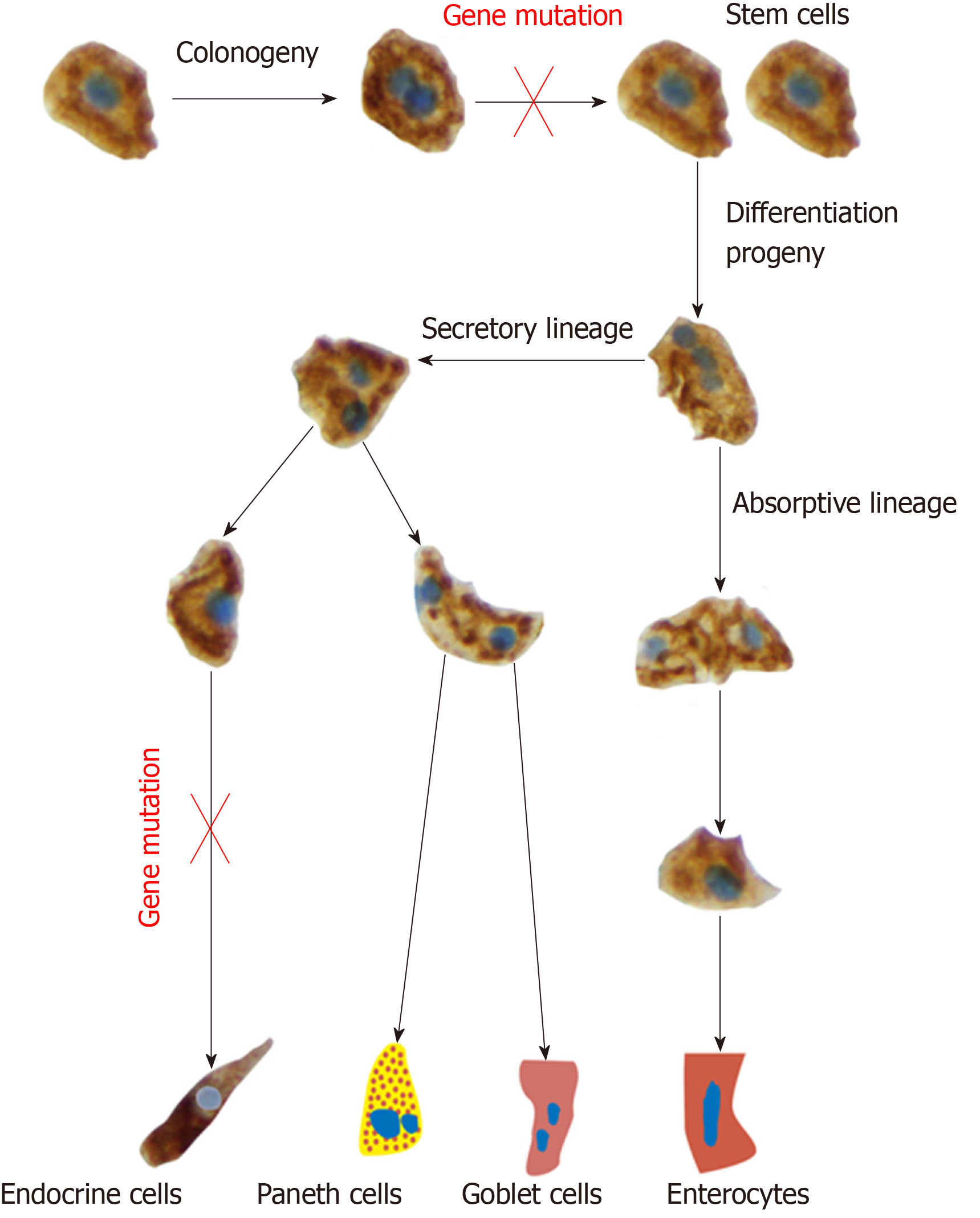
Figure 4 The intestinal stem cell divides into 2 identical cells (clonogeny).
One of these cells remain inactive, while the other stem cell differentiates into all cell types of the villus epithelium through 2 cell lineages: The secretory lineage giving raise to goblet cells, endocrine cells and Paneth cells, and the absorptive lineage giving raise to absorptive enterocytes. This differentiation occurs through a series of progenitors. The observations that the density of stem cells and progenitors for enteroendocrine cells, led to the assumption of gene mutations affecting the stem cell and neurogenin 3 gene.
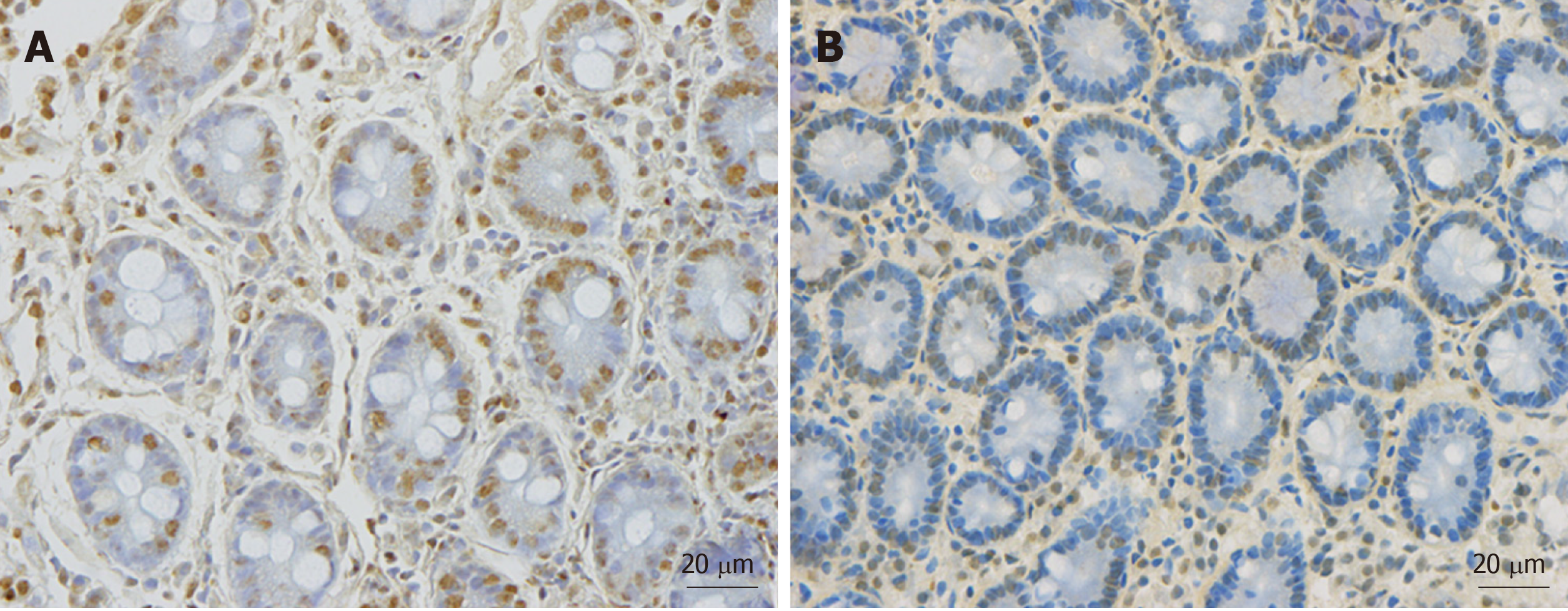
Figure 5 Musashi 1 immunoreactive cells in duodenum.
A: A healthy subject; B: A patient with irritable bowel syndrome (IBS). Musashi 1 is a marker for intestinal stem cells and their early progeny. The density of Musahi 1 cells in healthy subjects is higher than that of the IBS patients. Furthermore, Musashi 1 cells in healthy subjects appear to have more proliferation activity than that of IBS patients.
Figure 6 Neurogenin 3 immunoreactive cells in the duodenum.
A: A healthy control; B: A patient with irritable bowel syndrome. Neurogenin 3 is expressed in the nuclei (brown) of early intestinal endocrine cell progenitors. The healthy subjects have higher density of neurogenin 3 than irritable bowel syndrome patients.
Figure 7 Schematic drawing to illustrate the hypothesis that intestinal stem cells play a central role in the pathophysiology of irritable bowel syndrome.
The abnormalities in the intestinal stem cells can be caused by gene mutation or by environmental factors such as diet, intestinal microbiota, stress and low-grade inflammation.
- Citation: El-Salhy M. Possible role of intestinal stem cells in the pathophysiology of irritable bowel syndrome. World J Gastroenterol 2020; 26(13): 1427-1438
- URL: https://www.wjgnet.com/1007-9327/full/v26/i13/1427.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i13.1427