Copyright
©The Author(s) 2019.
World J Gastroenterol. Mar 28, 2019; 25(12): 1457-1464
Published online Mar 28, 2019. doi: 10.3748/wjg.v25.i12.1457
Published online Mar 28, 2019. doi: 10.3748/wjg.v25.i12.1457
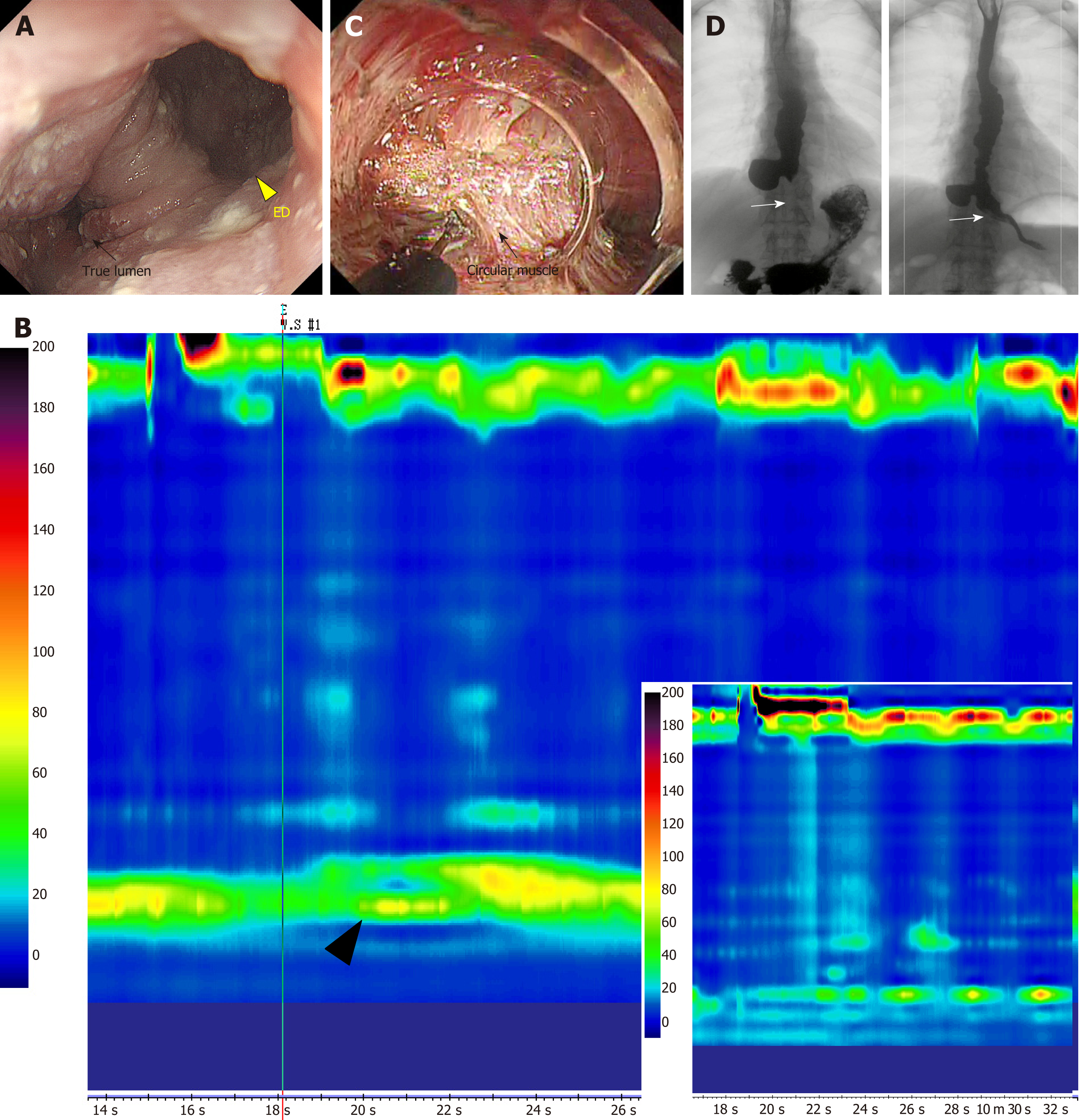
Figure 1 Epiphrenic diverticulum with achalasia treated using salvage peroral endoscopic myotomy.
A: A giant epiphrenic diverticulum (yellow triangle) is visible in the right anterior wall through gastrointestinal endoscopy. The true lumen is compressed and never opens (black arrow); B: On high resolution manometry (HRM), the mean lower esophageal sphincter (LES) pressure is elevated (black triangle) and no normal peristalsis is observed. The patient is diagnosed with type I achalasia. The right lower insert shows the HRM findings after salvage peroral endoscopic myotomy (s-POEM), showing decreased LES pressure; C: s-POEM: Posterior wall myotomy (of the side opposite to the diverticulum, black arrow) is performed longitudinally from the oral terminus of the diverticulum to the gastric terminus, through the LES; D: Preoperative esophagography (left) showing barium inflow into the diverticulum. Some stagnant barium is observed in the mid to lower esophagus. After s-POEM (right), barium flow through the true lumen shows significant improvement and pathologic muscle contraction in the LES area is relieved (white arrow). ED: Epiphrenic diverticulum.
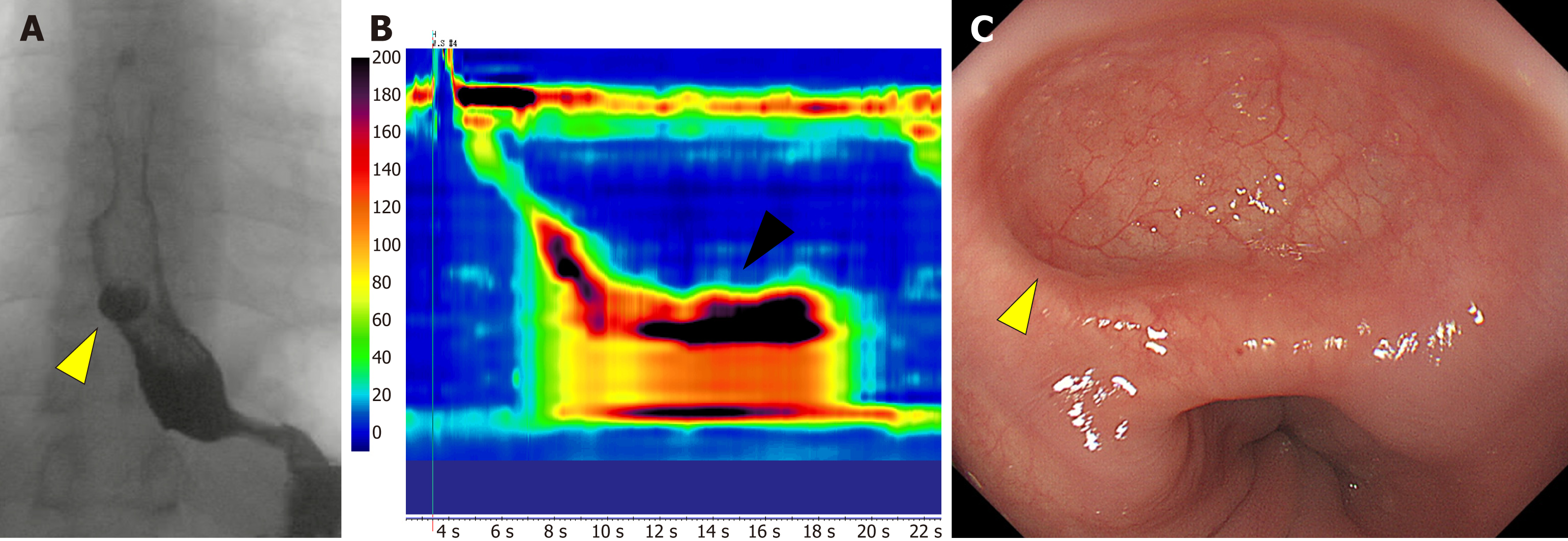
Figure 2 A case of iatrogenic diverticulum after peroral endoscopic myotomy.
A: An iatrogenic diverticulum (yellow triangle) is visible on the anterior right wall in the lower esophagus on barium swallow; B: Hypercontractions on high resolution manometry persisted after peroral endoscopic myotomy, causing pulsion of the esophageal wall; C: Endoscopic view of the iatrogenic diverticulum of the esophagus that developed on the side where peroral endoscopic myotomy was performed, which lacks a muscle layer.
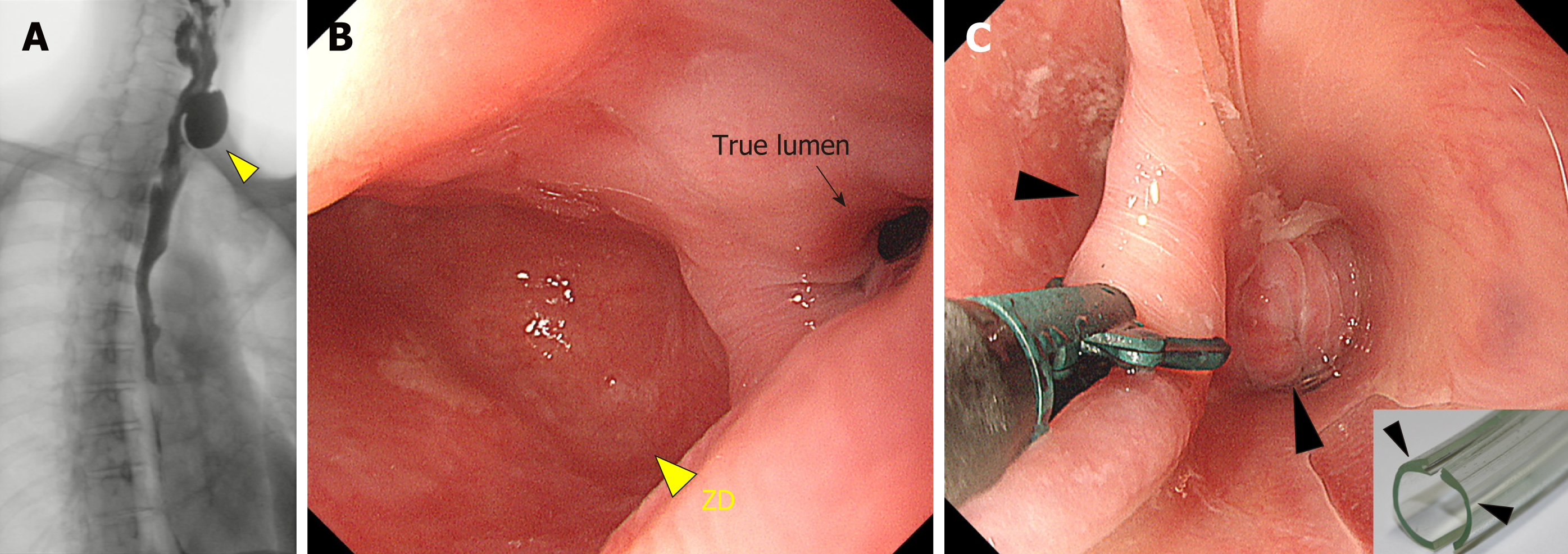
Figure 3 Zenker’s diverticulum treated using endoscopic diverticulectomy.
A: Zenker’s diverticulum (ZD, yellow triangle) visible on a barium swallow; B: On endoscopy, the ZD (yellow triangle) is easily visible and is bigger than the true esophageal lumen (black arrow); C: Endoscopic diverticulectomy is performed with a diverticuloscope (insert) straddled across the septum, with one flap inserted into the bottom of the ZD and the other in the esophageal lumen (black arrow) for a clear visualization of the septum and safe diverticulectomy[34]. ZD: Zenker’s diverticulum.
- Citation: Sato H, Takeuchi M, Hashimoto S, Mizuno KI, Furukawa K, Sato A, Yokoyama J, Terai S. Esophageal diverticulum: New perspectives in the era of minimally invasive endoscopic treatment. World J Gastroenterol 2019; 25(12): 1457-1464
- URL: https://www.wjgnet.com/1007-9327/full/v25/i12/1457.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i12.1457