©The Author(s) 2018.
World J Gastroenterol. Nov 21, 2018; 24(43): 4950-4958
Published online Nov 21, 2018. doi: 10.3748/wjg.v24.i43.4950
Published online Nov 21, 2018. doi: 10.3748/wjg.v24.i43.4950
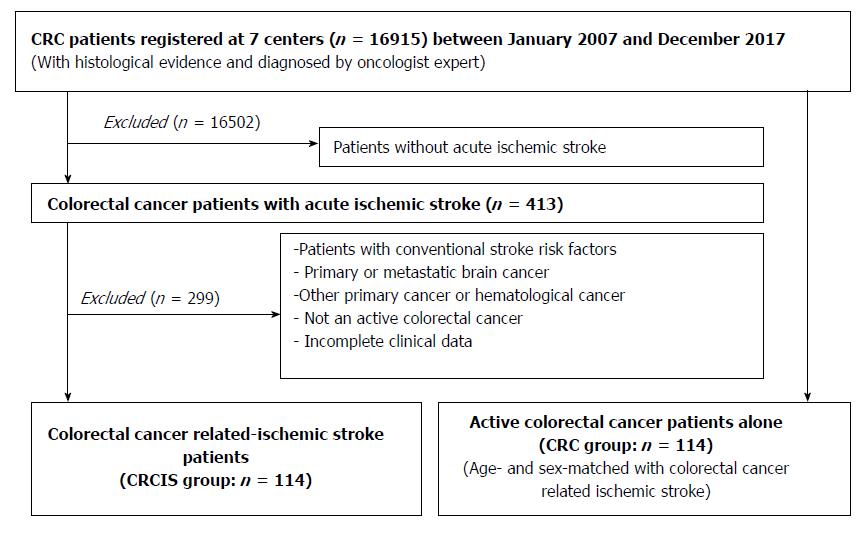
Figure 1 Patient selection.
CRC: Colorectal cancer.
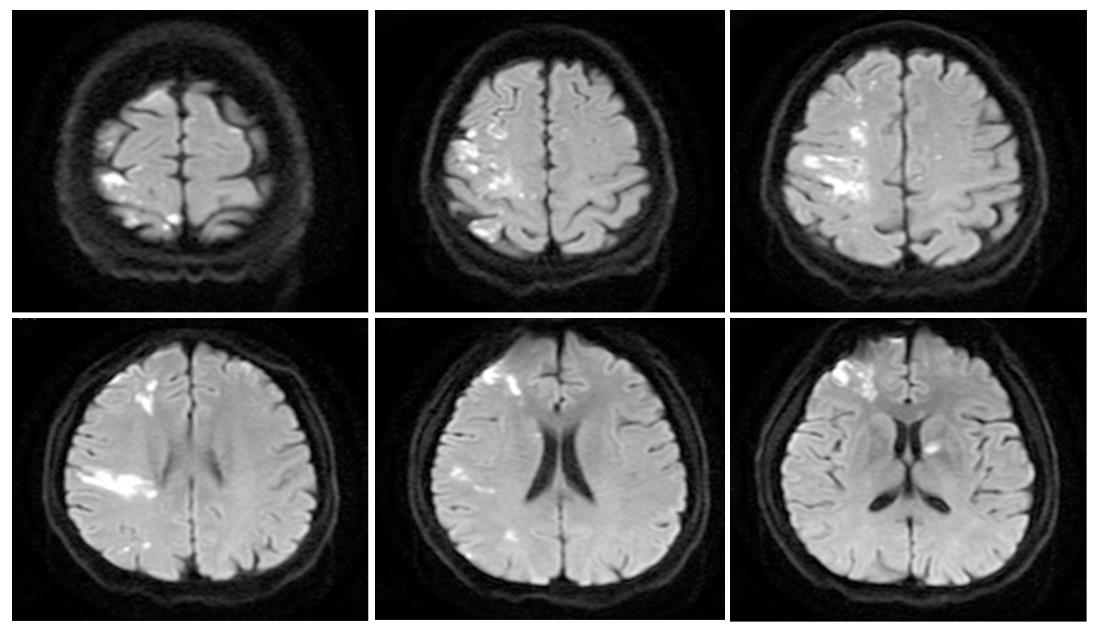
Figure 2 Typical presentation of ischemic stroke in a colorectal cancer patient without conventional stroke mechanism.
A 47-year-old male patient experienced acute ischemic stroke in the first 3 mo after diagnosis of colorectal cancer. Diffusion-weighted magnetic resonance imaging showed high signal changes in the middle cerebral and anterior cerebral and anterior choroidal arteries. Echocardiography results were normal.
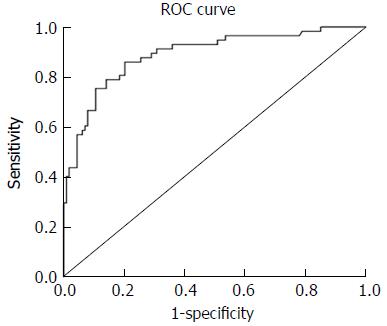
Figure 3 Receiver operator characteristic curve analysis of the product of D-dimer, carcinoembryonic antigen, and neutrophil count.
The area under the curve of the products was 0.889 ± 0.022 (95%CI: 0.847-0.932, P < 0.001). The optimum cut-off point was 252.06. At this cut-off value, the sensitivity was 86.0% and the specificity was 79.8%. CI: Confidence interval; ROC: Receiver operator characteristic.
- Citation: Qin QX, Cheng XM, Lu LZ, Wei YF, Wang DC, Li HH, Li GH, Liang HB, Li SY, Chen L, Liang ZJ. Biomarkers and potential pathogenesis of colorectal cancer-related ischemic stroke. World J Gastroenterol 2018; 24(43): 4950-4958
- URL: https://www.wjgnet.com/1007-9327/full/v24/i43/4950.htm
- DOI: https://dx.doi.org/10.3748/wjg.v24.i43.4950