©The Author(s) 2018.
World J Gastroenterol. Jun 28, 2018; 24(24): 2640-2646
Published online Jun 28, 2018. doi: 10.3748/wjg.v24.i24.2640
Published online Jun 28, 2018. doi: 10.3748/wjg.v24.i24.2640
Figure 1 May 1984 computed tomography scan revealed a giant, heterogeneous tumor in the right liver with internal calcifications, but the nature of the tumor was not clarified.
This may be an examination conducted by the first computed tomography scan machine in China.
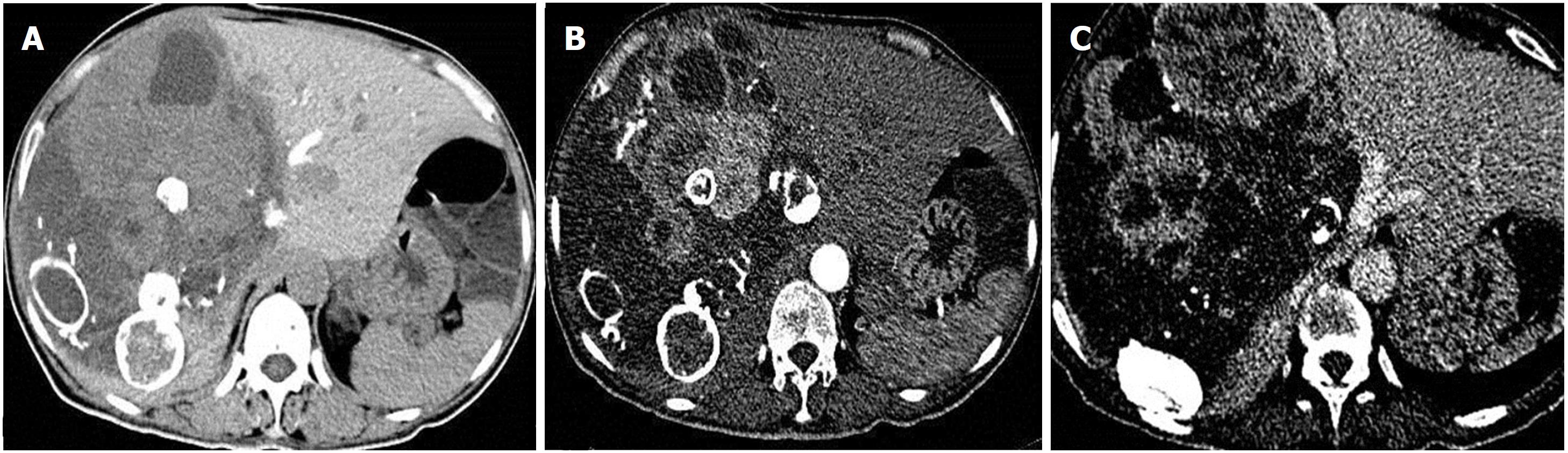
Figure 2 Computed tomography images of the patient in 1985, 2004, and 2010, respectively.
Figure 3 Enhanced computed tomography scan after admission in 2010.
A: Routine (noncontrast) scan: A huge space-occupying lesion of the right liver, with a size 20 cm × 16 cm × 11 cm. The internal density was heterogeneous, and liquid density and multiple enveloped calcifications could be observed; B: Arterial phase: the tumor parenchyma showed substantial and uniform enhancement; C: Portal vein phase: the tumor parenchyma did not show rapid subsidence and still showed higher densities.
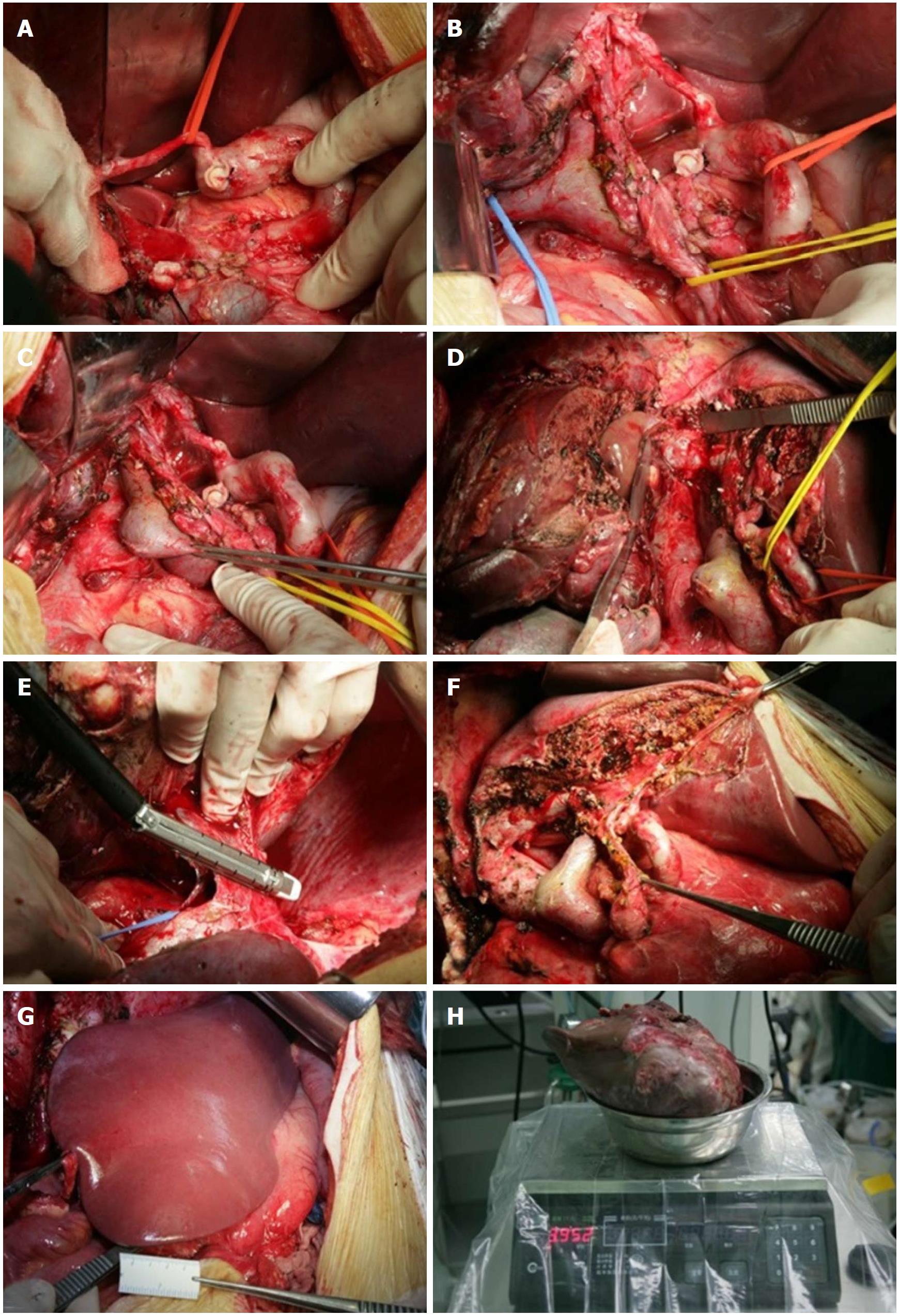
Figure 4 Surgical procedures.
A: Separation of the hepatic artery, suspension of the left hepatic artery, and the right hepatic artery was ligated and transected; B: Separation of the portal vein and bile duct. The right hepatic duct was transected and sutured; C: Separation of the right portal vein; D: Splitting the liver parenchyma to the inferior vena cava; E: Severing of the right hepatic vein using the stapler; F: Condition after surgical resection, showing that the left hepatic artery, left portal vein, and left hepatic duct were structurally intact; G: The remaining liver after resection was ruddy in color, with no ischemia or blood stasis; H: The specimen weight was 3952 g.
- Citation: Meng XF, Pan YW, Wang ZB, Duan WD. Primary hepatic neuroendocrine tumor case with a preoperative course of 26 years: A case report and literature review. World J Gastroenterol 2018; 24(24): 2640-2646
- URL: https://www.wjgnet.com/1007-9327/full/v24/i24/2640.htm
- DOI: https://dx.doi.org/10.3748/wjg.v24.i24.2640