©The Author(s) 2018.
World J Gastroenterol. Jun 14, 2018; 24(22): 2406-2412
Published online Jun 14, 2018. doi: 10.3748/wjg.v24.i22.2406
Published online Jun 14, 2018. doi: 10.3748/wjg.v24.i22.2406
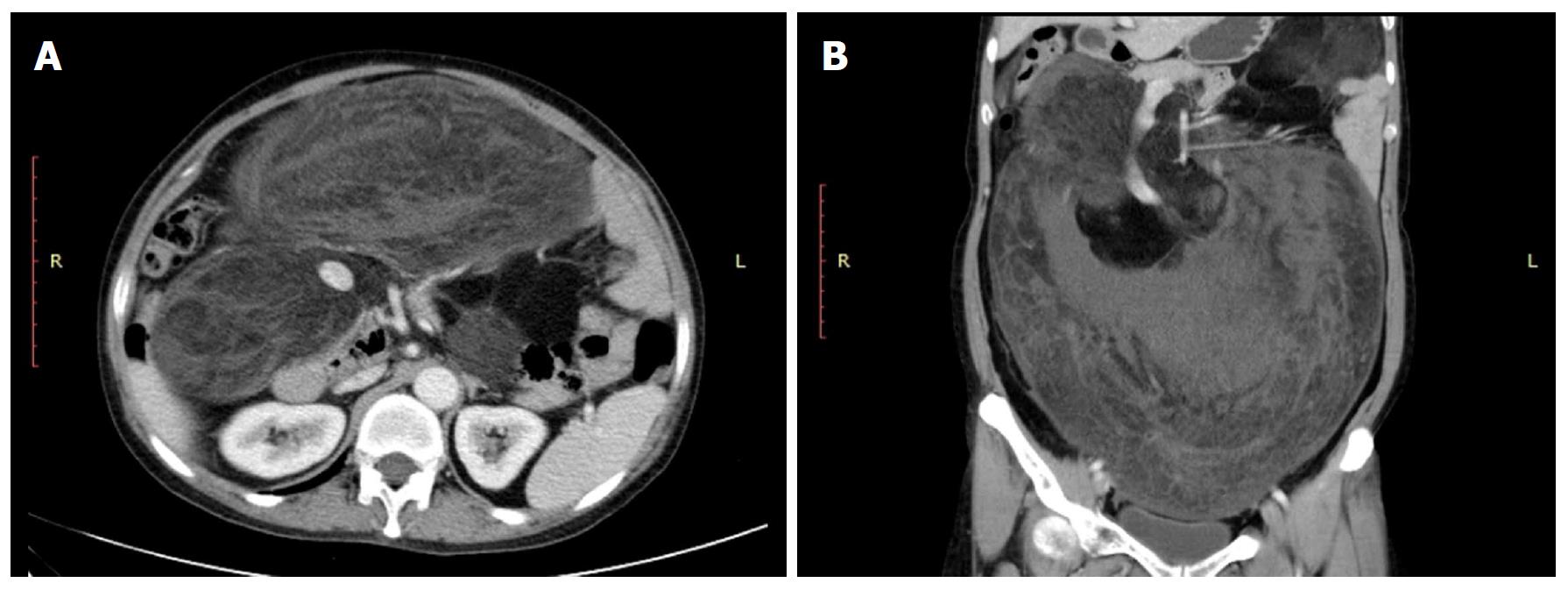
Figure 1 Preoperative computed tomography scan.
A: Abdominal contrast-enhanced computed tomography showing a large tumor (118 mm × 258 mm × 303 mm) in the abdomen. B: Coronal multiplanar reformation showing that the lesion adhered to and constricted the main trunk of the superior mesenteric vein.
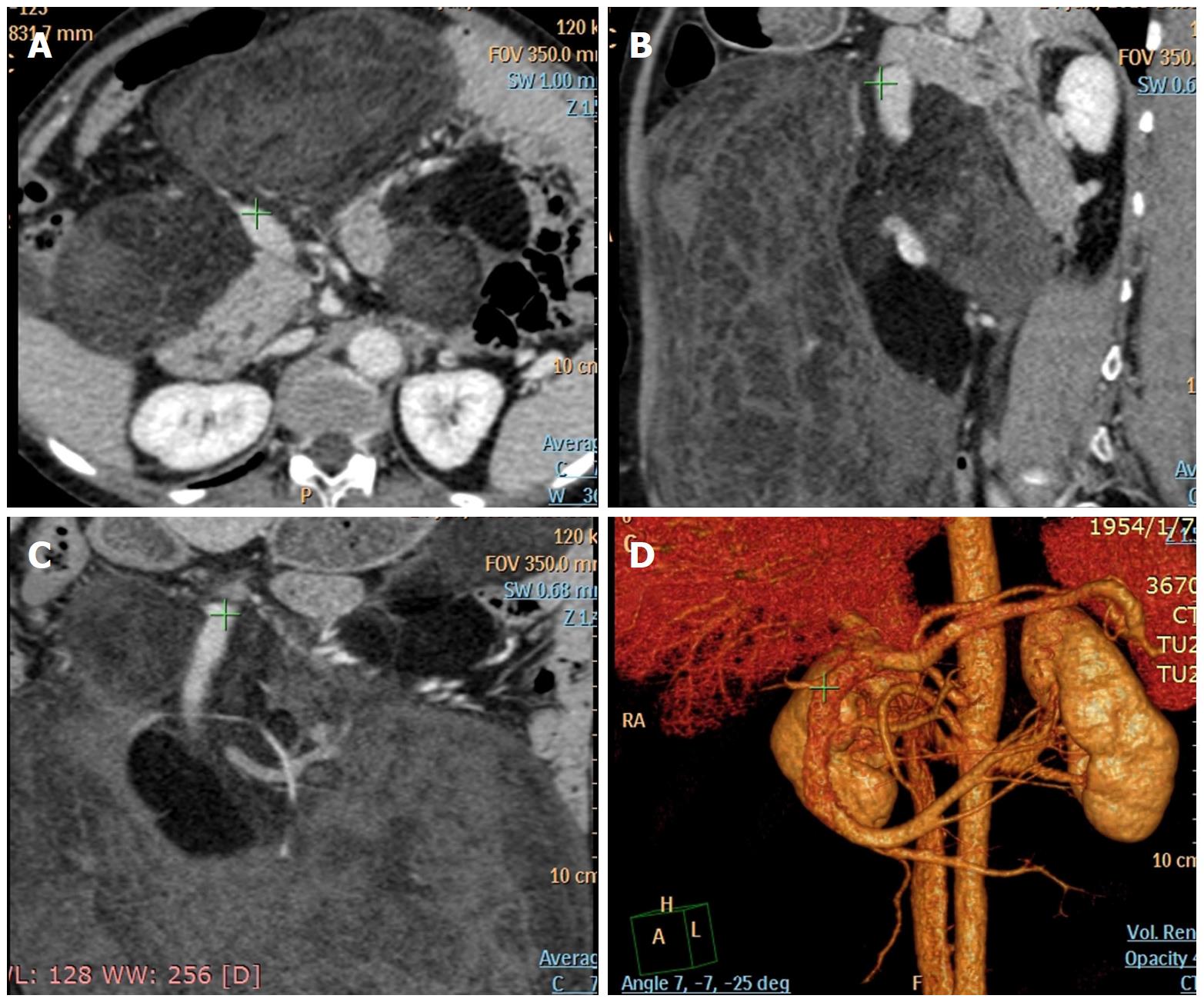
Figure 2 Preoperative abdominal computed tomographic angiography.
A-C: The same location (green cross) of the main trunk of the superior mesenteric vein in the horizontal scan, coronary scan, and sagittal scan. D: 3-dimensional CT scan showing that the lesion adhered to and constricted the main trunk of the superior mesenteric vein.
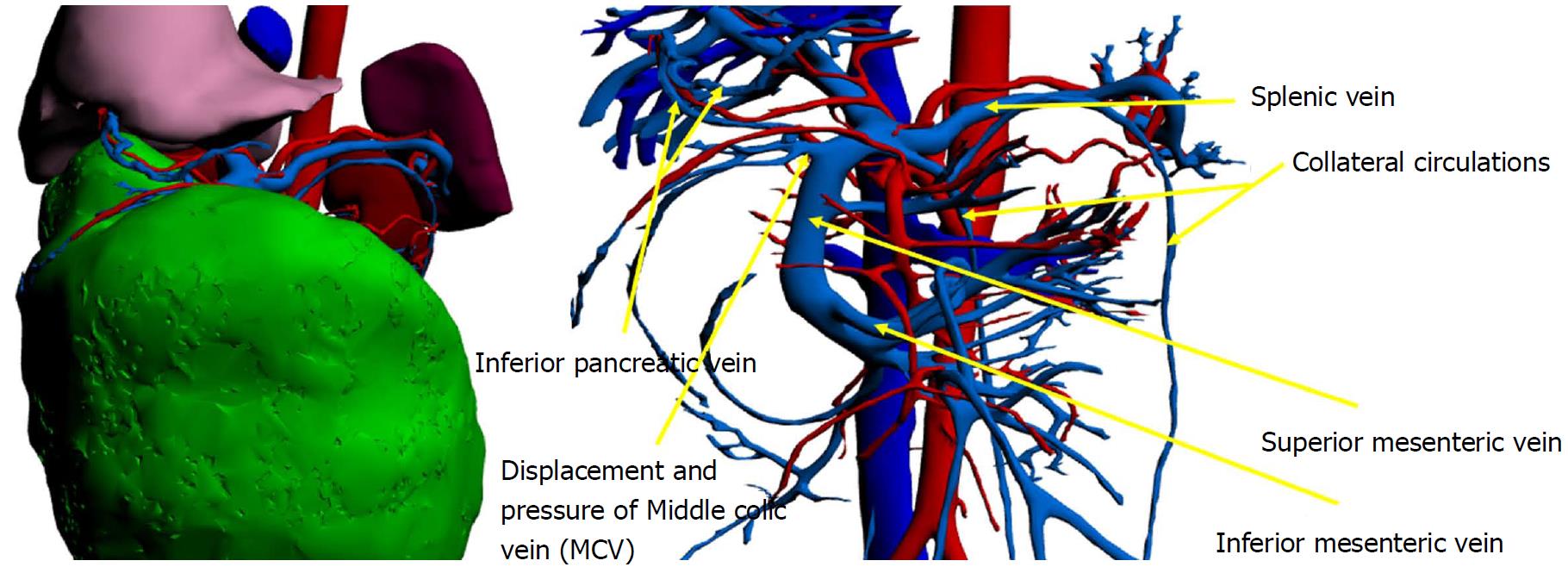
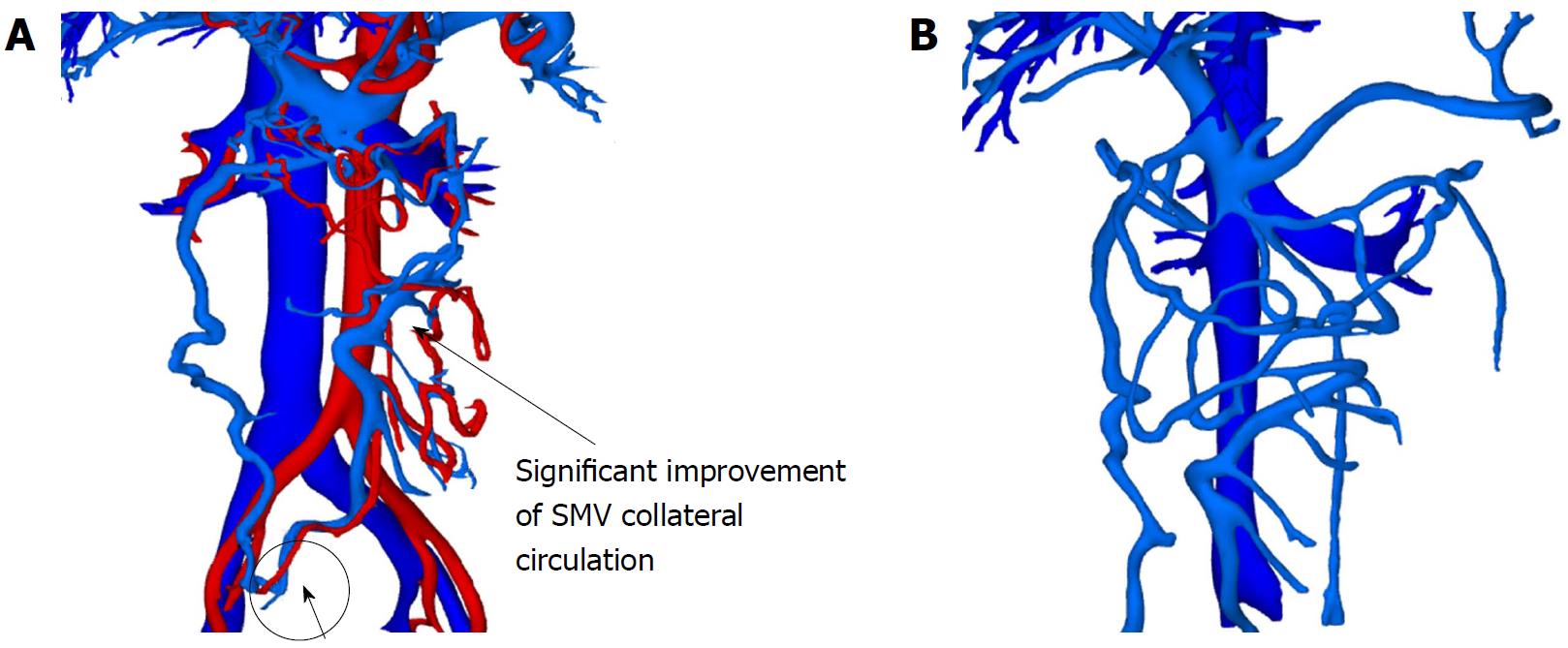
Figure 3 Preoperative vascular reconstruction plan: Superior mesenteric vein collateral circulation development.
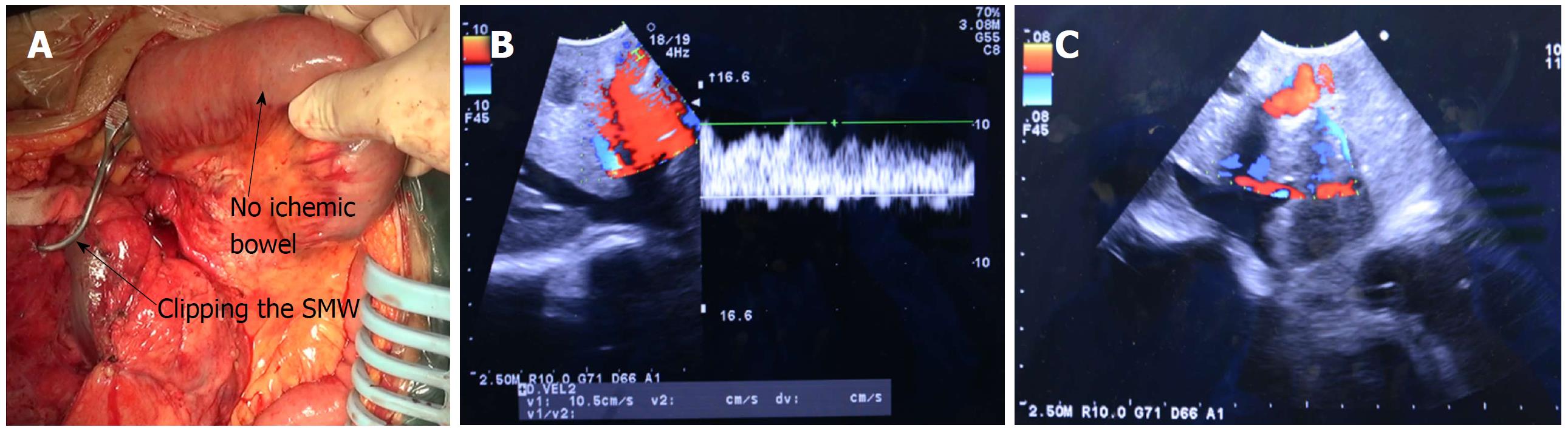
Figure 4 Normal bowel after the superior mesenteric vein was occluded by vessel clamp (A); and Doppler B-ultrasound showing venous blood flow (B and C).
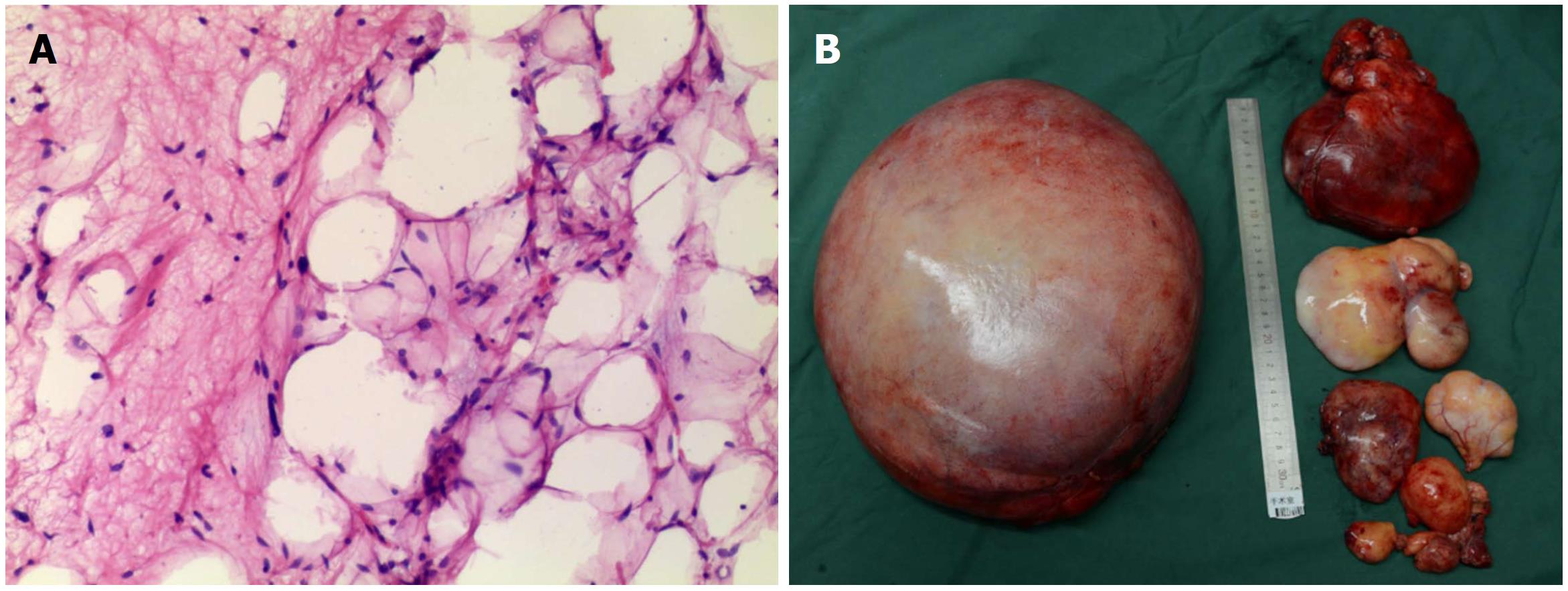
Figure 5 Histological analysis revealing a well-differentiated retroperitoneal liposarcoma (A) and surgical specimen of the liposarcoma (B).
Figure 6 Vascular reconstruction scan on postoperative day 20 showing significant improvement in superior mesenteric vein collateral circulation and inferior mesenteric vein (A).
B: Vascular reconstruction scan 2 mo after the operation. Various and remarkable SMV collateral circulation flow returning to the portal vein and IMV. SMV: Superior mesenteric vein.
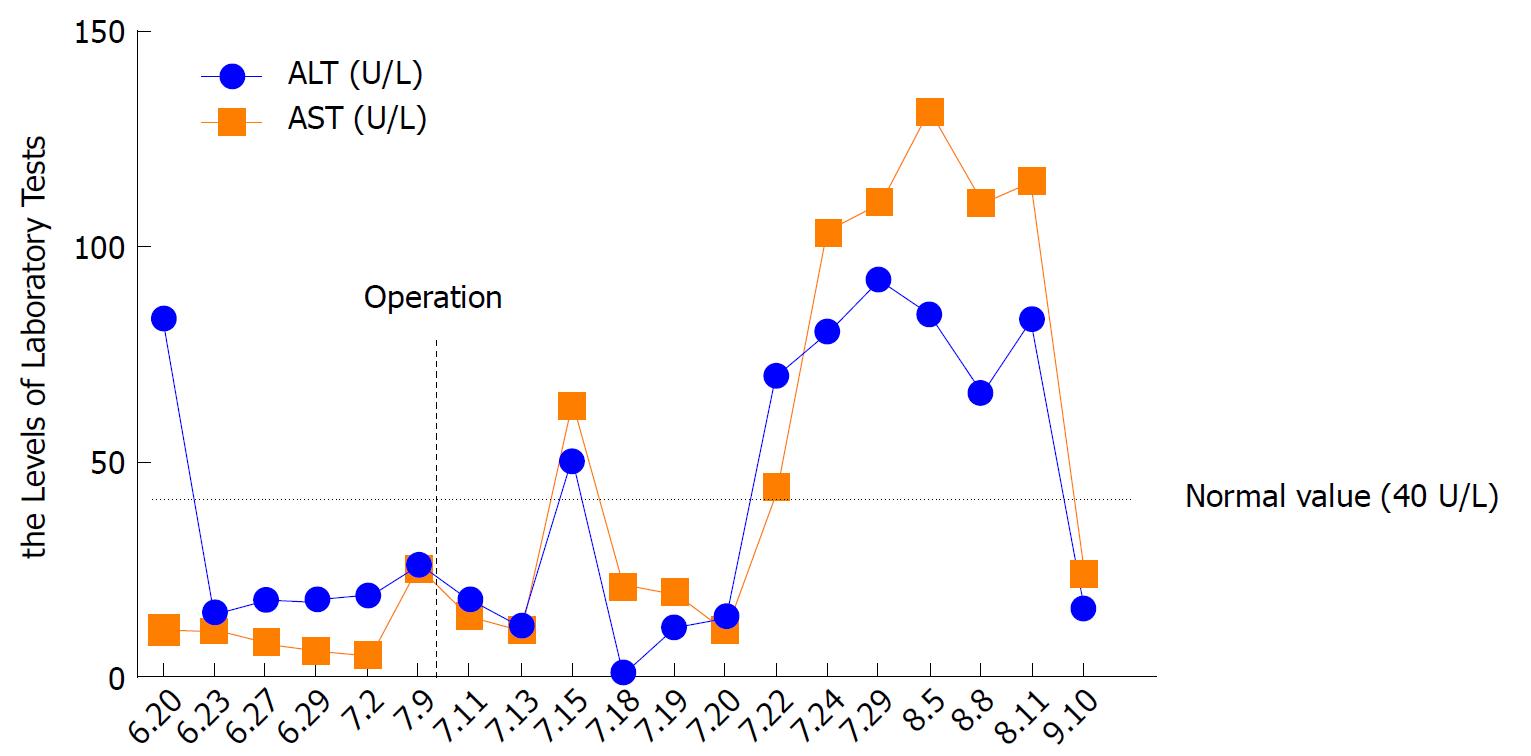
Figure 7 The change in alanine aminotransferase (orange line) and aspartate aminotransferase (blue line) levels during the hospital stay.
- Citation: Miao RC, Wan Y, Zhang XG, Zhang X, Deng Y, Liu C. Devascularization of the superior mesenteric vein without reconstruction during surgery for retroperitoneal liposarcoma: A case report and review of literature. World J Gastroenterol 2018; 24(22): 2406-2412
- URL: https://www.wjgnet.com/1007-9327/full/v24/i22/2406.htm
- DOI: https://dx.doi.org/10.3748/wjg.v24.i22.2406