©The Author(s) 2017.
World J Gastroenterol. Oct 21, 2017; 23(39): 7191-7197
Published online Oct 21, 2017. doi: 10.3748/wjg.v23.i39.7191
Published online Oct 21, 2017. doi: 10.3748/wjg.v23.i39.7191
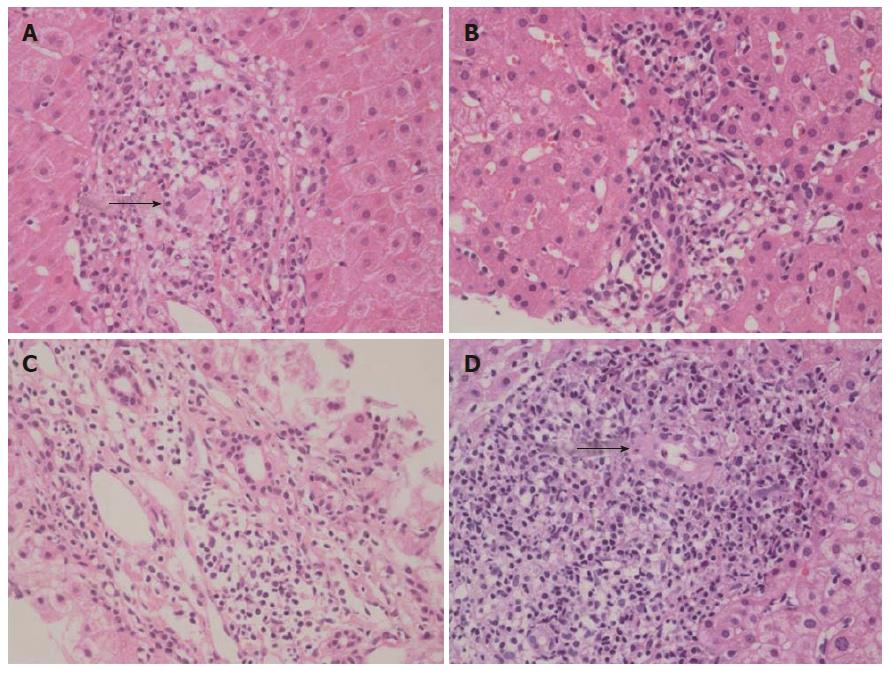
Figure 1 Microscopic features of the patients’ liver biopsies (H&E stain, × 400).
A: Patient 1: A non-necrotizing granuloma is surrounded by lymphoid infiltrates (arrow); B: Patient 2: Aggregates of lymphocytes indicate the early phase of the disease; C: Patient 3: Mild portal inflammation without bile duct damage or granuloma is present; D: Patient 4: A damaged bile duct is identified in a background of lymphocytes and plasma cells (arrow).
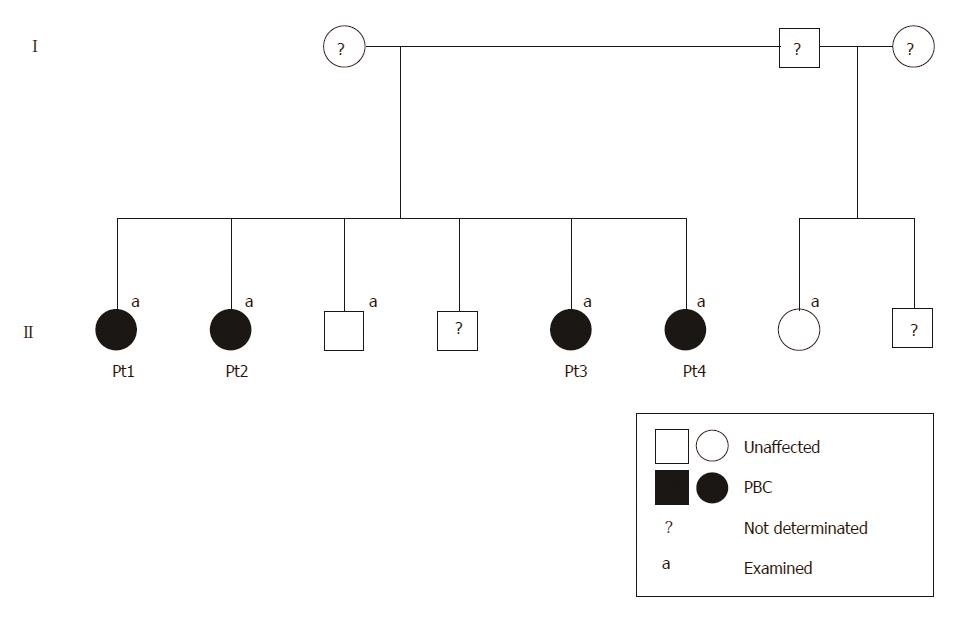
Figure 2 Pedigree of a family with four sisters with diagnoses of primary biliary cholangitis.
The black symbols indicate clinically affected family members, and the white symbols indicate non-affected members. No phenotypically relevant information was available for the members with question marks. Pt: Patient; PBC: Primary biliary cholangitis.
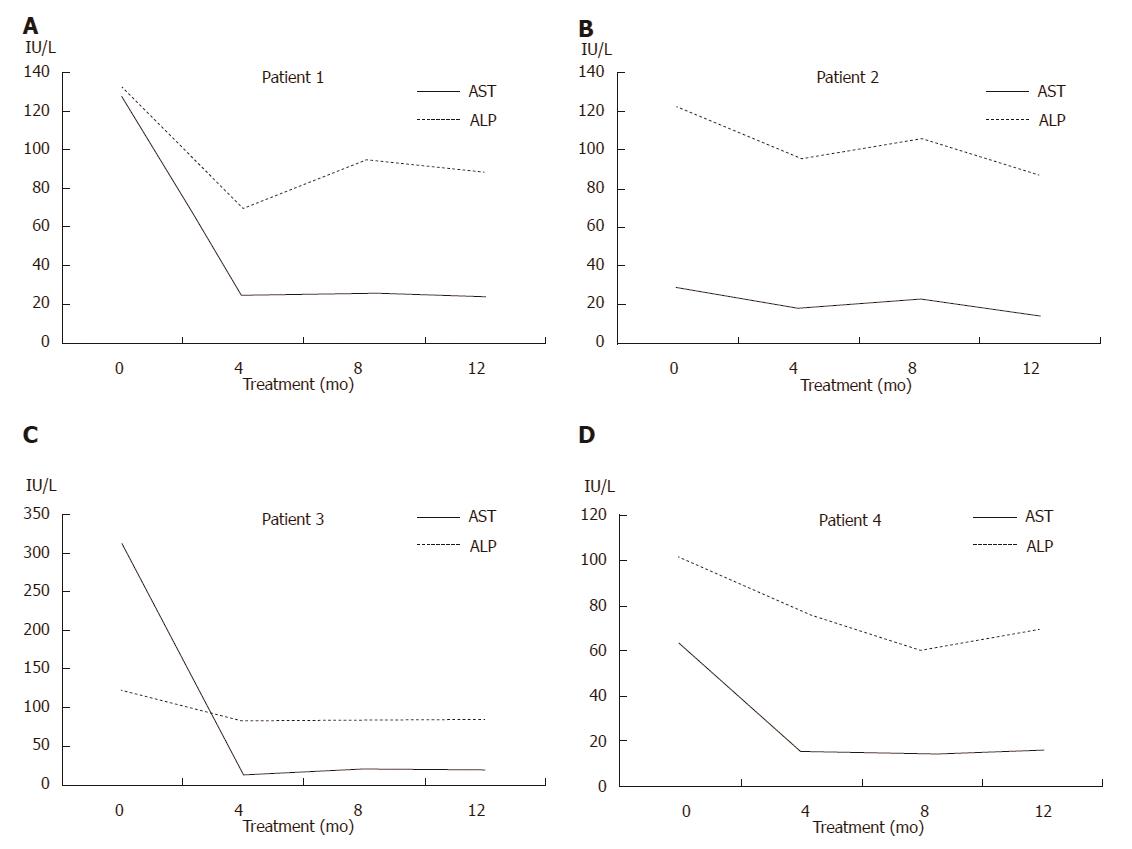
Figure 3 Biochemical responses to ursodeoxycholic acid treatment.
A-D: Serum activities of aspartate aminotransferase (AST; solid lines) and alkaline phosphatase (ALP; dotted lines) showing good responses to ursodeoxycholic acid in patients 1-4.
- Citation: Shin S, Moh IH, Woo YS, Jung SW, Kim JB, Park JW, Suk KT, Kim HS, Hong M, Park SH, Lee MS. Evidence from a familial case suggests maternal inheritance of primary biliary cholangitis. World J Gastroenterol 2017; 23(39): 7191-7197
- URL: https://www.wjgnet.com/1007-9327/full/v23/i39/7191.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i39.7191