Copyright
©The Author(s) 2017.
World J Gastroenterol. Jul 7, 2017; 23(25): 4508-4516
Published online Jul 7, 2017. doi: 10.3748/wjg.v23.i25.4508
Published online Jul 7, 2017. doi: 10.3748/wjg.v23.i25.4508
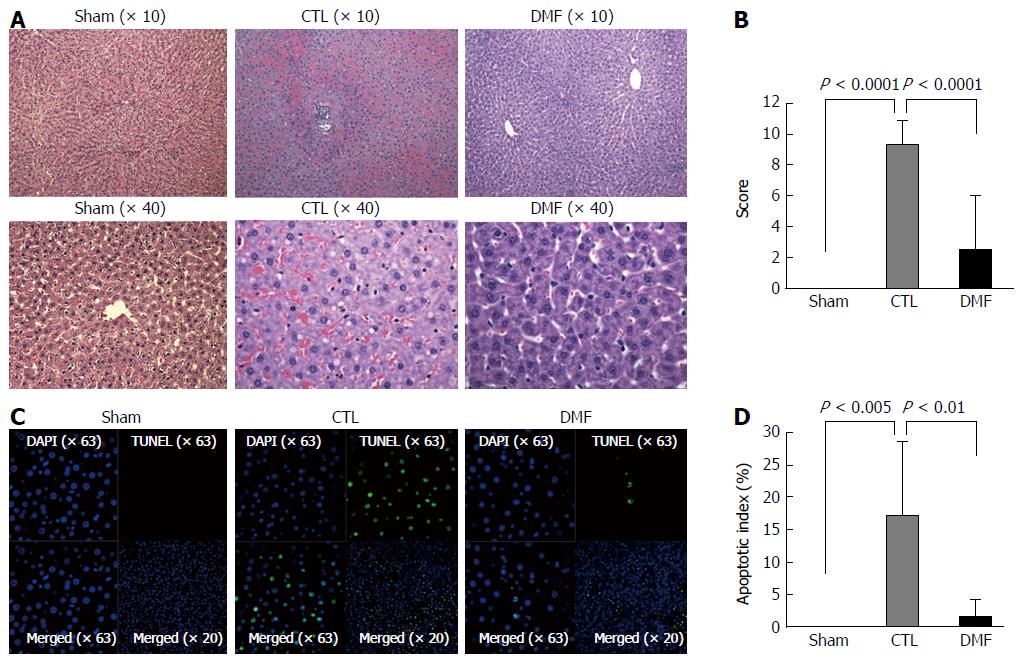
Figure 1 Liver ischemia/reperfusion injury in a rat model.
A: Hematoxylin and eosin (H&E)-stained histology of rat liver subjected to 60 min of ischemia and 2 h of reperfusion. The levels of substantial intracellular vacuolization, sinusoidal dilatation, congestion, and focal necrosis of the liver parenchyma in the dimethyl fumarate (DMF) group were significantly improved compared to those of the CTL group; B: Liver histology damage scoring (Suzuki score). Data represent the mean ± SD. Pretreatment with DMF ameliorated ischemia/reperfusion injury (I/RI)-induced histological changes; C: TUNEL staining of rat liver subjected to 60 min of ischemia and 2 h of reperfusion. The DMF-treated group had significantly fewer TUNEL-positive cells (green fluorescence) than the CTL group; D: Apoptotic index indicating that pretreatment with DMF improved I/RI-induced apoptosis (P ≤ 0.01). Data represent the mean ± SD. DMF: Dimethyl fumarate; CTL: Control.
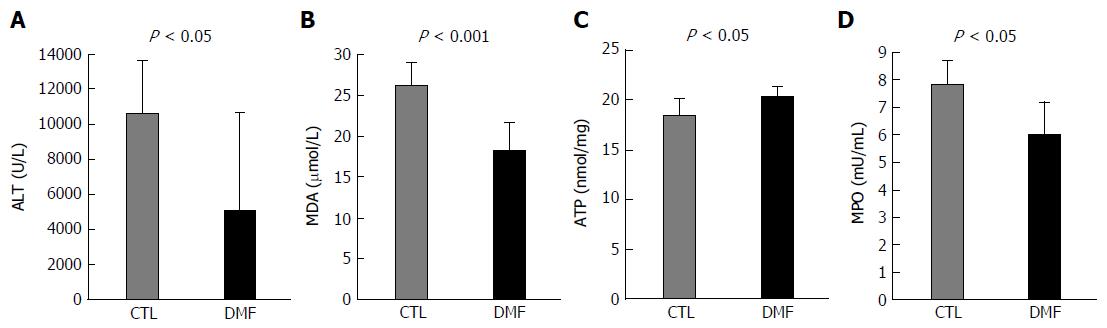
Figure 2 Effect of dimethyl fumarate on serum alanine aminotransferase and malondialdehyde and liver adenosine triphosphate and myeloperoxidase.
The levels of serum alanine aminotransferase (ALT) (A) and malondialdehyde (MDA) (B) and liver adenosine triphosphate (ATP) (C) and myeloperoxidase (MPO) (C) in the liver tissue were determined. Serum ALT and MDA in the DMF group were significantly lower than in the CTL group (ALT: P < 0.05, MDA: P < 0.001; data represent the mean ± SD). Liver ATP in the DMF group was significantly higher than in the CTL group (P < 0.05; data represent the mean ± SD). Liver MPO in the DMF group was significantly lower than in the CTL group (P < 0.05; data represent the mean ± SD). DMF: Dimethyl fumarate; CTL: Control.
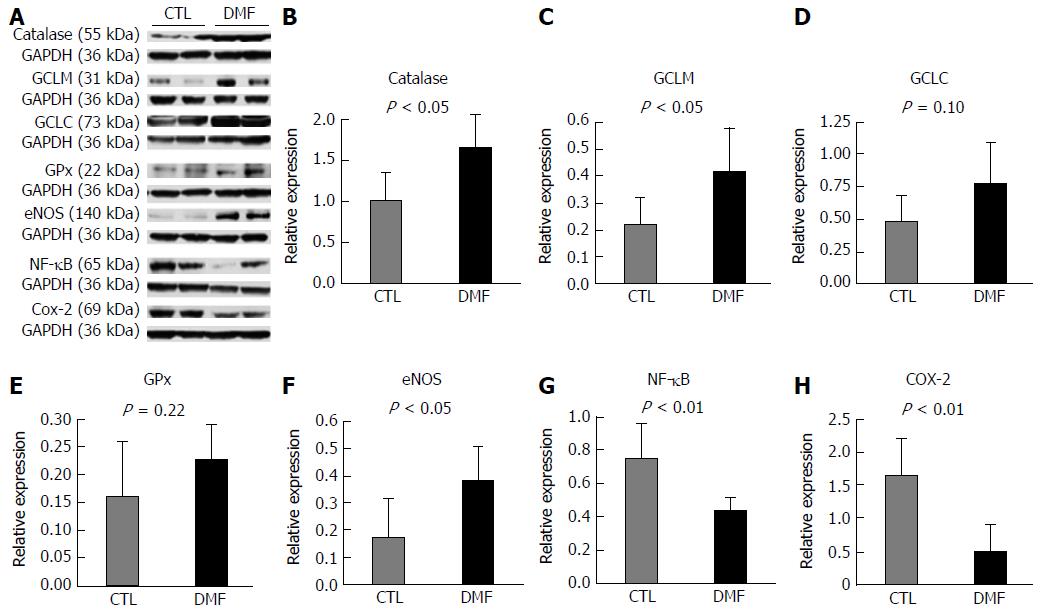
Figure 3 Effects of dimethyl fumarate on the expression levels of anti-oxidant enzymes, endothelial nitric oxide synthase, NF-κB and cyclooxygenase-2 in the liver.
A: Representative western blots of CAT, GCLM, GCLC, GPx, eNOS, NF-κB and COX-2 in the CTL and dimethyl fumarate (DMF) groups. The bar graph summarizing the western blot data of (B) CAT, (C) GCLM, (D) GCLC, (E) GPx, (F) eNOS, (G) NF-κB, and (H) COX-2. Data represent the mean ± SD. Significant increases in liver CAT and GCLM expression levels were observed in the DMF group compared to those in the CTL group (CAT: P = 0.03, Figure 3B; GCLM: P = 0.04, Figure 3C). The protein expression of eNOS was also enhanced by DMF administration compared to that of the CTL group (P = 0.02, Figure 3F). Furthermore, DMF decreased the levels of NF-κB and COX-2 expression in the liver (NF-κB, P = 0.01, Figure 3G; COX-2, P = 0.007, Figure 3H). The protein expression levels of GPx, HO-1, SOD and NQO-1 were not significantly different between the two groups (GPx: P = 0.22, HO-1: P = 0.39, SOD: P = 0.32 and NQO-1: P = 0.95). GCLM: Glutamate-cysteine ligase modifier subunit; COX-2: Cyclooxygenase-2; GCLC: Glutamate-cysteine ligase catalytic subunit; eNOS: Endothelial nitric oxide synthase; GPx: Glutathione peroxidase; DMF: Dimethyl fumarate; CTL: Control.
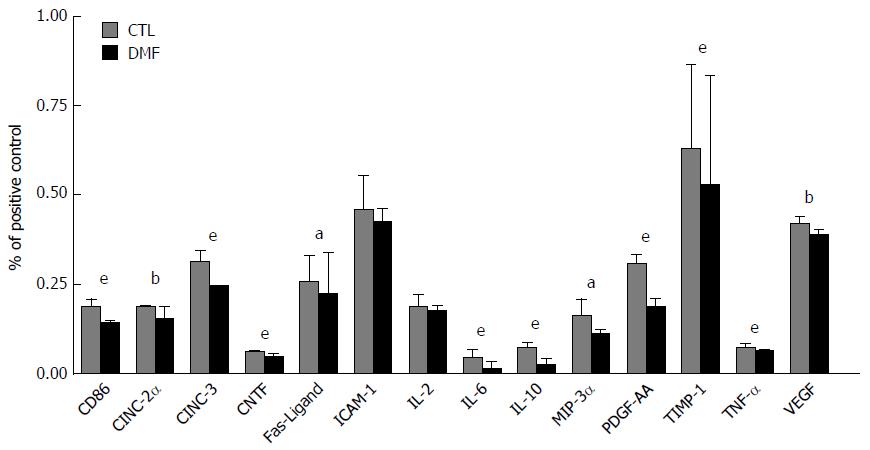
Figure 4 Inflammatory mediator production in rat serum.
Dimethyl fumarate (DMF) significantly reduced the production of inflammatory mediators in the serum relative to the CTL group. Significant reductions of CD86, CINC-2α, CINC-3, CNTF, Fas ligand, IL-6, IL-10, MIP-3α, PDGF-AA, TIMP-1, TNF-α and VEGF were observed in the DMF-treated group. Data represent the mean ± SD (aP < 0.05, bP < 0.01, eP < 0.001). DMF: Dimethyl fumarate; CTL: Control; IL: Interleukin; CD86: Cluster of differentiation 86; CINC-2α: Cytokine-induced neutrophil chemoattractant-2α; CNTF: Ciliary neurotrophic factor; MIP-3α: Macrophage inflammatory protein-3α; PDGF-AA: Platelet-derived growth factor-AA; TIMP-1: Tissue inhibitor of metalloproteinase 1; TNF-α: Tumor necrosis factor α; VEGF: Vascular endothelial growth factor.
- Citation: Takasu C, Vaziri ND, Li S, Robles L, Vo K, Takasu M, Pham C, Farzaneh SH, Shimada M, Stamos MJ, Ichii H. Treatment with dimethyl fumarate ameliorates liver ischemia/reperfusion injury. World J Gastroenterol 2017; 23(25): 4508-4516
- URL: https://www.wjgnet.com/1007-9327/full/v23/i25/4508.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i25.4508