©The Author(s) 2016.
World J Gastroenterol. Dec 28, 2016; 22(48): 10512-10522
Published online Dec 28, 2016. doi: 10.3748/wjg.v22.i48.10512
Published online Dec 28, 2016. doi: 10.3748/wjg.v22.i48.10512
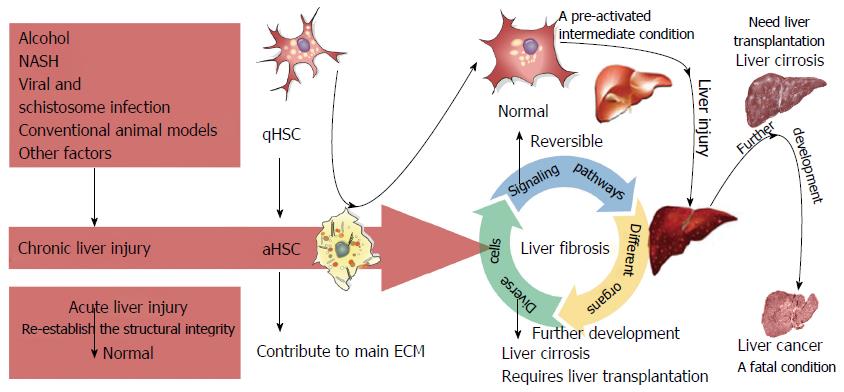
Figure 1 Initiation, progression, and resolution of liver fibrosis involving hepatic stellate cells.
Upon various types of chronic injury - including that caused by alcohol, viral and schistosome infection, nonalcoholic steatohepatitis (NASH), and other factors - hepatic stellate cells (HSCs) transdifferentiate from quiescent HSCs to activated HSCs, the latter of which secrete abundant extracellular proteins that contribute to liver fibrosis. Liver fibrosis is thought to be a reversible condition owing to the elimination of causative agents and different strategies of limiting HSC activation; however, they cannot totally return to a quiescent status of the naive HSCs. Instead, they exhibit a pre-activated intermediate condition with an increased sensitivity to injury. Thus, preventing recurrent chronic liver injury is of great importance in patients undergoing treatment for liver fibrosis. Untreated or relapsed fibrosis progresses to liver cirrhosis, which often requires hepatic transplantation.
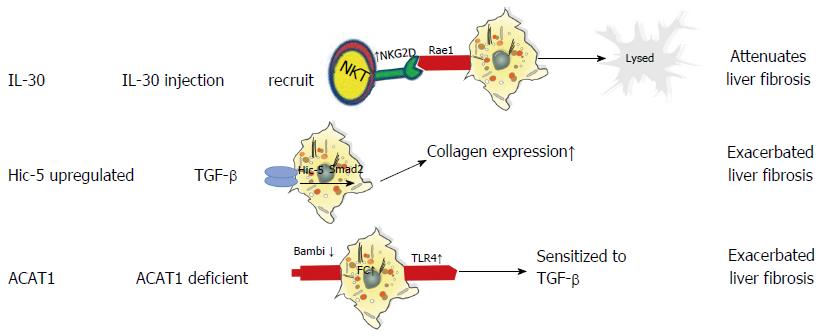
Figure 2 Roles of interleukin-30, hydrogen peroxide inducible clone 5, and cholesterol acyltransferase 1 in liver fibrosis.
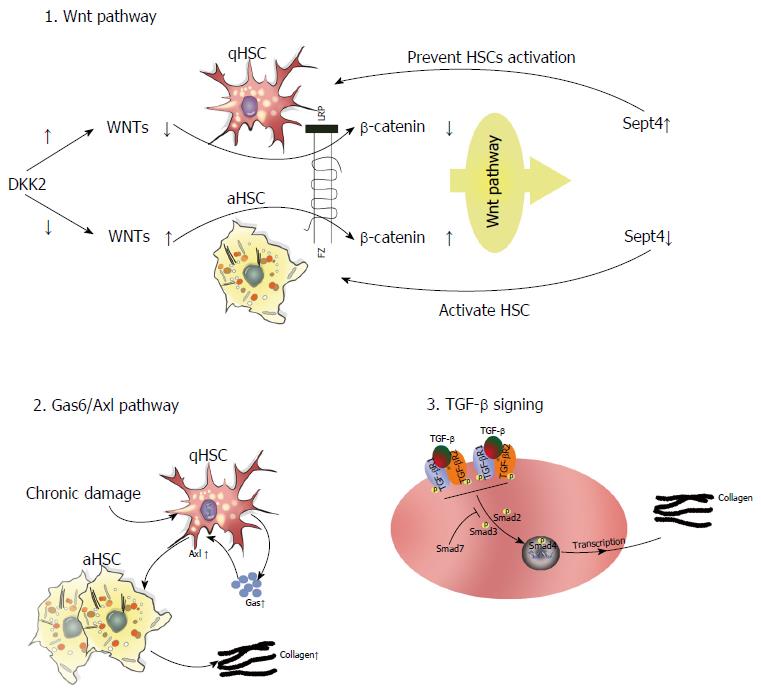
Figure 3 Roles of the Wnt, TGF-β/Smad, and Gas6/Axl signaling pathways in the progression of liver fibrosis.
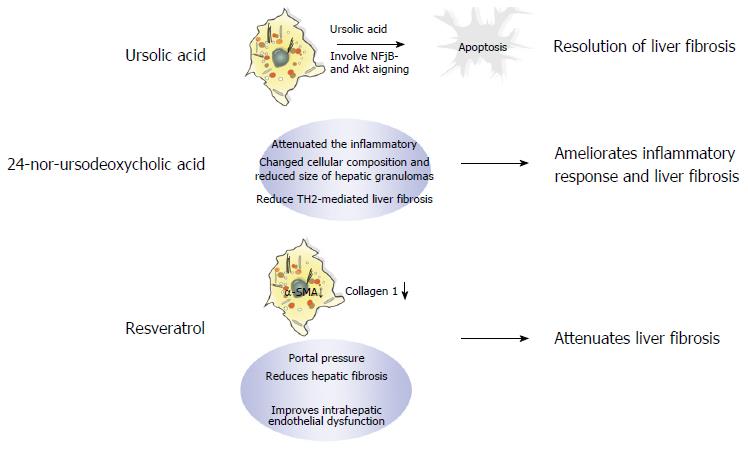
Figure 4 Mechanism of action of three potential therapeutic drugs-ursolic acid, 24-nor-ursodeoxycholic acid, and resveratrol-for treating fibrosis.
- Citation: Zhang CY, Yuan WG, He P, Lei JH, Wang CX. Liver fibrosis and hepatic stellate cells: Etiology, pathological hallmarks and therapeutic targets. World J Gastroenterol 2016; 22(48): 10512-10522
- URL: https://www.wjgnet.com/1007-9327/full/v22/i48/10512.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i48.10512