©The Author(s) 2016.
World J Gastroenterol. Jan 28, 2016; 22(4): 1582-1592
Published online Jan 28, 2016. doi: 10.3748/wjg.v22.i4.1582
Published online Jan 28, 2016. doi: 10.3748/wjg.v22.i4.1582
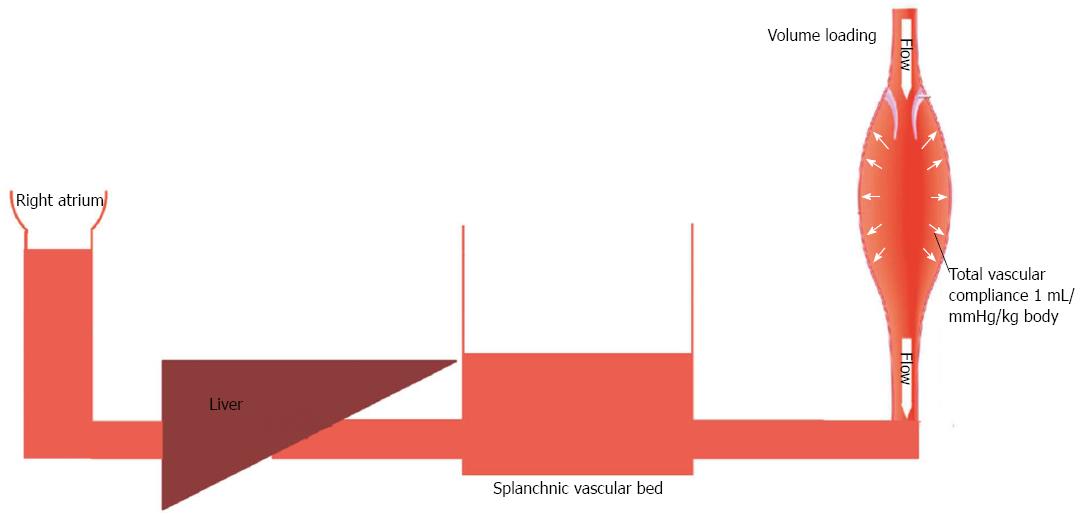
Figure 1 Fluid loading in a healthy subject.
Low vascular compliance combined with decreased pooling of blood in splanchnic circulation is associated with increased central venous pressure.
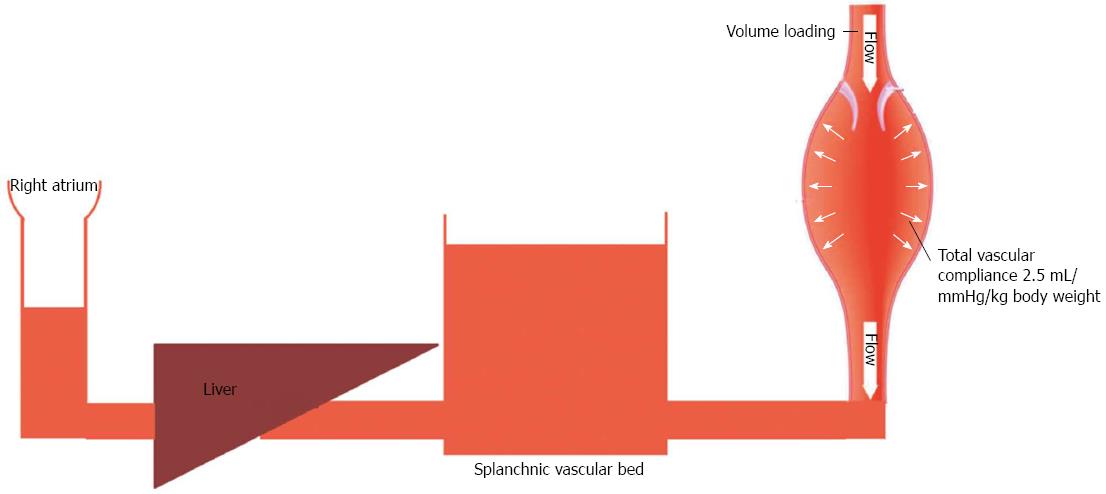
Figure 2 Fluid loading in a cirrhotic patient.
High vascular compliance combined with increased pooling of blood in splanchnic circulation is associated with a minimal increase in central venous pressure.
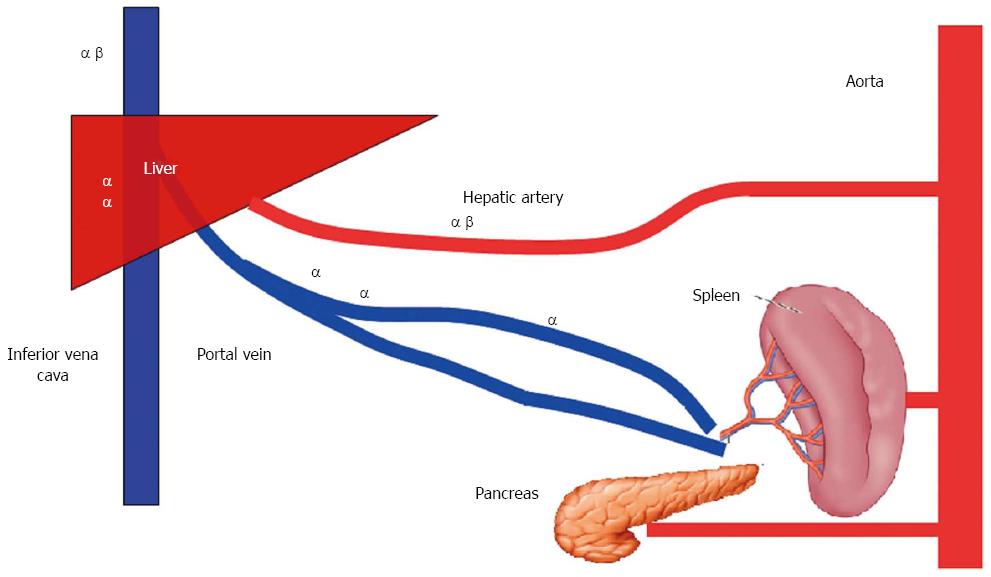
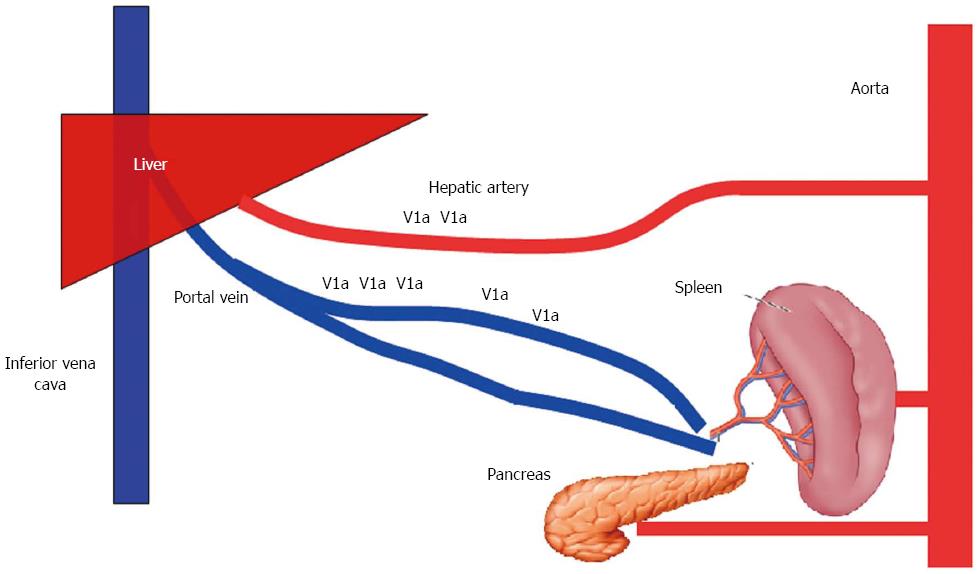
Figure 3 Anatomy of splanchnic blood flow.
The liver receives 25% of its arterial blood supply via the hepatic artery and the remaining 75% via the portal vein.
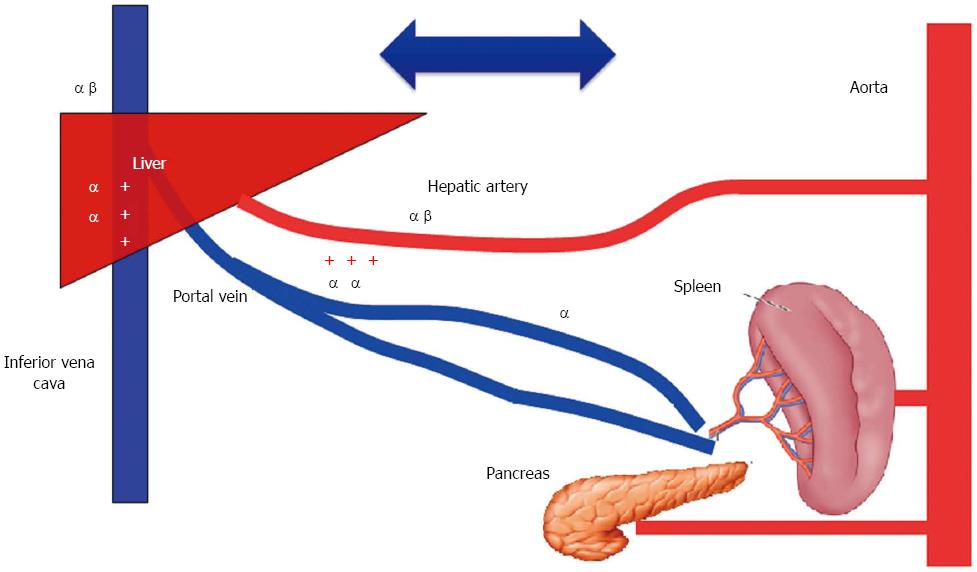
Figure 4 Distribution of catecholamine receptors in the splanchnic area.
The hepatic artery contains α1-, α2-, and β2-adrenergic receptors; the preportal (intestinal capacitance) and portal veins contain α-adrenergic, but not β2-adrenergic receptors. Capacitance vessels located inside the liver contain only α-adrenergic receptors, while the hepatic veins contain both α- and β2-adrenergic receptors.
Figure 5 Effect of stimulation of catecholamine receptors within the splanchnic area on blood flow.
Stimulation of α receptors in the pre- and post-portal capacitance vessels failed to create a gradient sufficient to shift blood from splanchnic to systemic circulation.
Figure 6 Distribution of vasopressin receptors in the splanchnic area.
V1a receptors are more prevalent on the portal venous side than the arterial side.
- Citation: Mukhtar A, Dabbous H. Modulation of splanchnic circulation: Role in perioperative management of liver transplant patients. World J Gastroenterol 2016; 22(4): 1582-1592
- URL: https://www.wjgnet.com/1007-9327/full/v22/i4/1582.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i4.1582