©The Author(s) 2016.
World J Gastroenterol. Aug 14, 2016; 22(30): 6925-6935
Published online Aug 14, 2016. doi: 10.3748/wjg.v22.i30.6925
Published online Aug 14, 2016. doi: 10.3748/wjg.v22.i30.6925
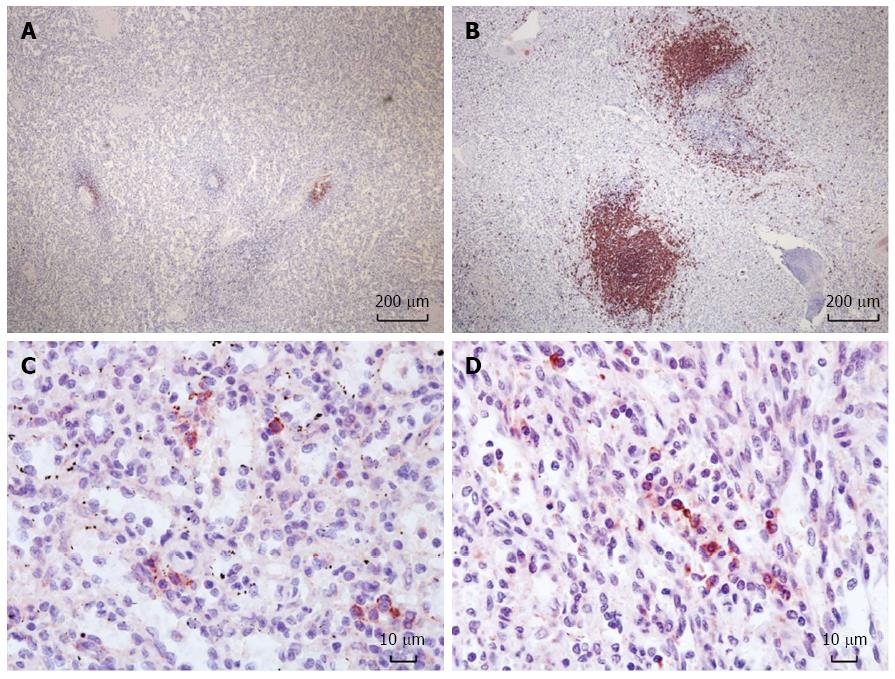
Figure 1 Immunohistochemistry of the spleen for CD20+ B-cell follicles and CD 138+ plasma cells.
Reduced size of B-cell follicles after rituximab prophylaxis in the spleen (A) compared to a control (B) (× 40). Plasma cells in the spleen with rituximab prophylaxis (C) and without (D) (× 400).
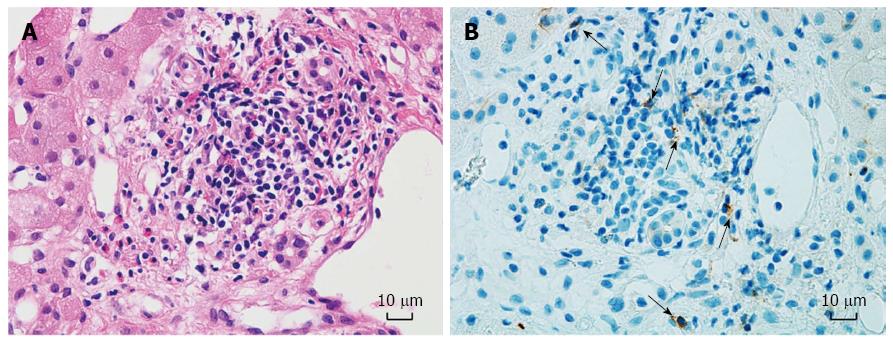
Figure 2 Liver biopsy pathology of case No.
12. Non-specific inflammation shown by H&E staining (A) (× 400). CD 56+ cells (black arrows) embedded in liver parenchyma (B) (× 400). The patient developed ITBL 23 d after the liver biopsy.
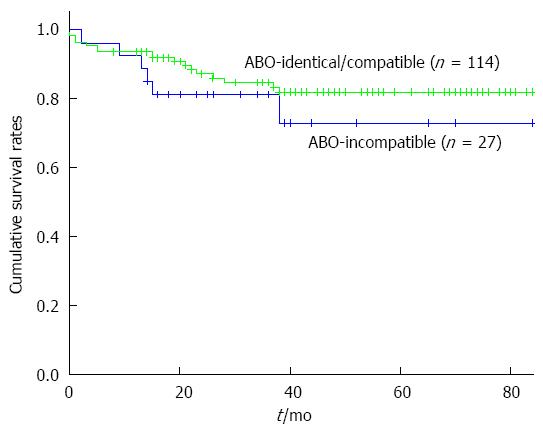
Figure 3 Overall survivals rates after adult living donor liver transplantation.
1-, 3-, and 5-yr survival rates are 93.9%, 84.8%, and 82% after ABO-identical/compatible ALDLT and 92.6%, 81.5%, and 73.0% after ABO-I ALDLT. There is no statistical difference between survival rates of the two groups (P = 0.303). ALDLT: Adult living donor liver transplantation.
Figure 4 Ischemic-type biliary lesion diagnosed by the cholangiogram via external biliary stent.
Diffuse dilatations of the intrahepatic bile ducts with irregularities are shown.
- Citation: Bang JB, Kim BW, Kim YB, Wang HJ, Lee HY, Sim J, Kim T, Lee KL, Hu XG, Mao W. Risk factor for ischemic-type biliary lesion after ABO-incompatible living donor liver transplantation. World J Gastroenterol 2016; 22(30): 6925-6935
- URL: https://www.wjgnet.com/1007-9327/full/v22/i30/6925.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i30.6925