Copyright
©The Author(s) 2015.
World J Gastroenterol. Dec 14, 2015; 21(46): 13140-13151
Published online Dec 14, 2015. doi: 10.3748/wjg.v21.i46.13140
Published online Dec 14, 2015. doi: 10.3748/wjg.v21.i46.13140
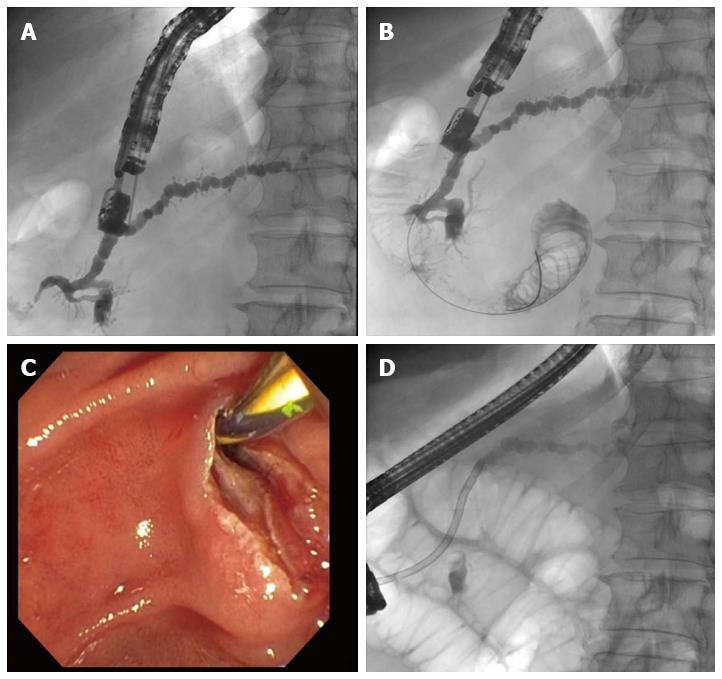
Figure 1 Patient with dilated pancreatic duct, recurrent pancreatitis, and pancreas divisum in whom endoscopic retrograde cholangiopancreatography has failed.
A: After endoscopic ultrasonography-guided puncture and administration of contrast medium, imaging of the pancreatic duct under fluoroscopic control shows there is almost no outflow of contrast medium out of the minor papilla; B: The guide wire is advanced into the pancreatic duct and through and out of the minor papilla; C: After changing to a duodenoscope, the guide wire was identified and an extending papillotomy was performed using a conventional technique; D: An 11.5-Fr. prosthesis is placed into the minor papilla, with subsequent adequate outflow of contrast medium.
Figure 2 Will’s high-frequency ring knife (MTW-Endoskopie, Wesel, Germany).
The inset top left shows the tip of the device, enlarged.
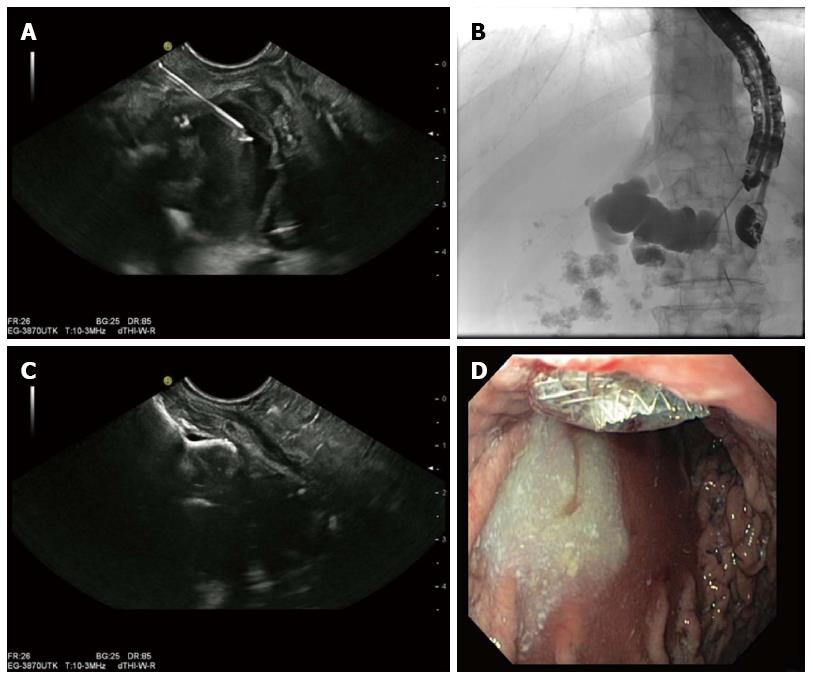
Figure 3 Patient with recurrent episodes of severe chronic pancreatitis and manifested retention of fluid in the pancreatic duct against a background of pancreatolithiasis in whom endoscopic retrograde cholangiopancreatography failed.
A: Endoscopic ultrasonography-guided puncture of the clearly dilated pancreatic duct; B: Pancreatography showed complete obturation of the pancreatic duct; C: After failure to advance the guide wire through and out of the papilla, a 10 mm × 10 mm AXIOSTM stent was released and the position of the intraductal part of the stent checked by endoscopic ultrasonography; D: The intragastric part of the AXIOSTM stent with secreted opaque pancreatic juice flowing into the gastric lumen.
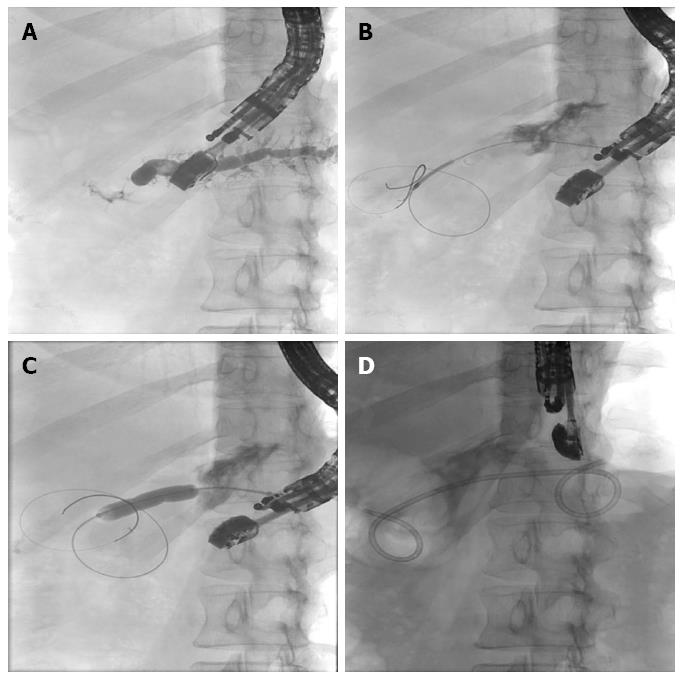
Figure 4 Patient with anastomotic stenosis and painful retention in the pancreatic duct after previous resection of the pancreatic head for a metastasis of bronchial carcinoma.
A: After endoscopic ultrasonography-guided puncture and pancreatography, retention of fluid in the pancreatic duct is revealed - there is no flow of contrast through the stenotic anastomosis; B: The guide wire is advanced through the anastomotic stenosis; C: Balloon dilatation of the anastomotic stenosis up to 8 mm; D: Transgastric implantation of a 7-Fr double-pigtail prosthesis as a so-called “ring drainage” (gastropancreatojejunostomy).
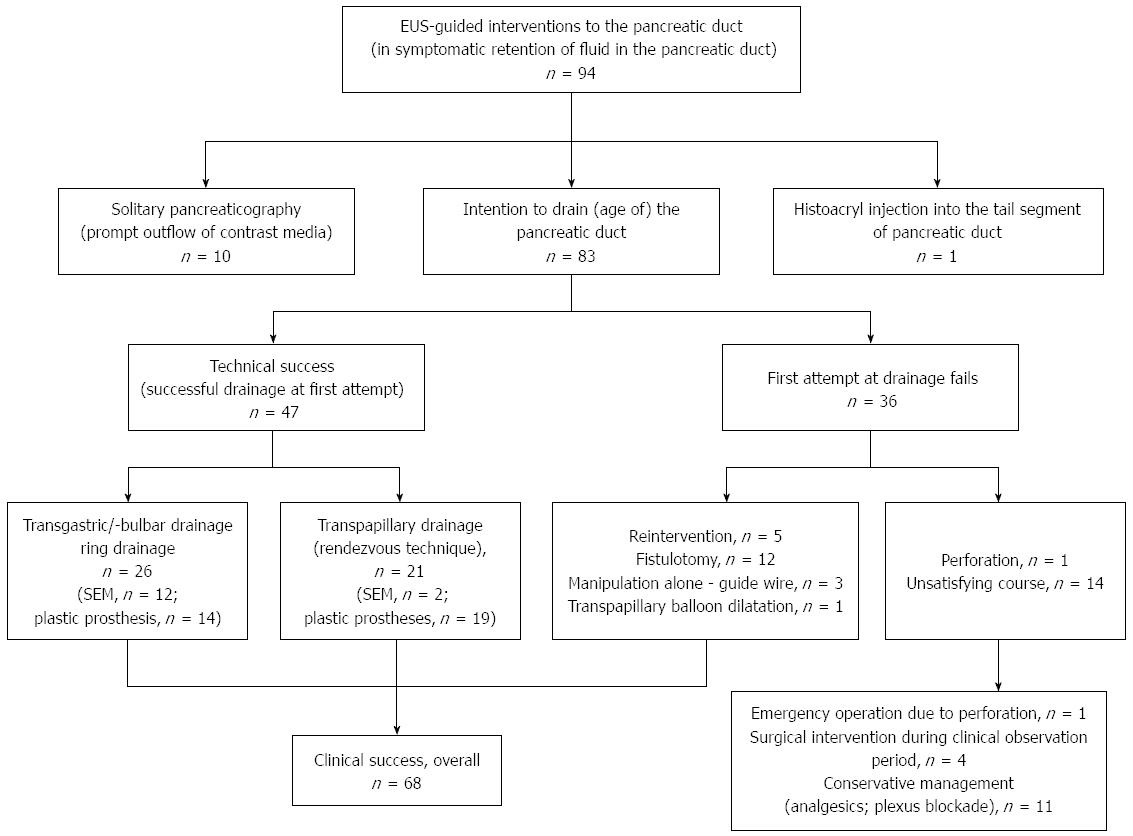
Figure 5 Overview of the endoscopic ultrasonography-guided interventions of the pancreatic duct performed at the Gera Municipal Hospital from June 2002 to April 2014.
EUS: Endoscopic ultrasonography; SEM: Self-expanding metal stent.
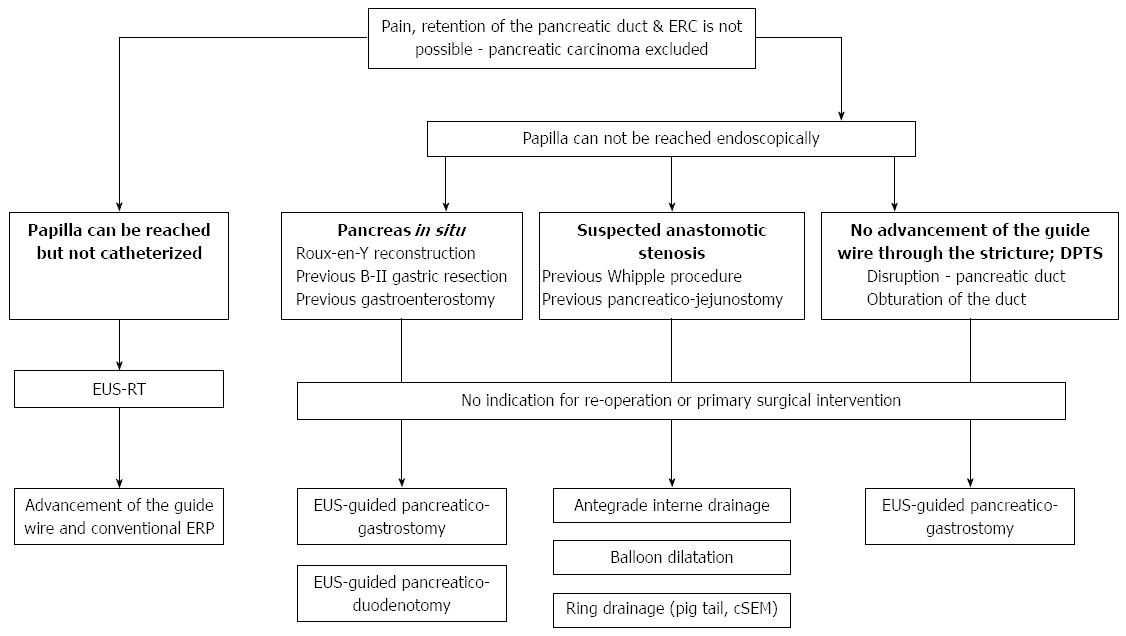
Figure 6 Treatment algorithm for patients with symptomatic retention in the pancreatic duct.
ERC: Endoscopic retrograde cholangiography; DPTS: Disconnected pancreatic tail syndrome; EUS: Endoscopic ultrasonography; EUS-RT: EUS-guided rendezvous technique.
- Citation: Will U, Reichel A, Fueldner F, Meyer F. Endoscopic ultrasonography-guided drainage for patients with symptomatic obstruction and enlargement of the pancreatic duct. World J Gastroenterol 2015; 21(46): 13140-13151
- URL: https://www.wjgnet.com/1007-9327/full/v21/i46/13140.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i46.13140