©2014 Baishideng Publishing Group Inc.
World J Gastroenterol. Dec 7, 2014; 20(45): 17260-17264
Published online Dec 7, 2014. doi: 10.3748/wjg.v20.i45.17260
Published online Dec 7, 2014. doi: 10.3748/wjg.v20.i45.17260
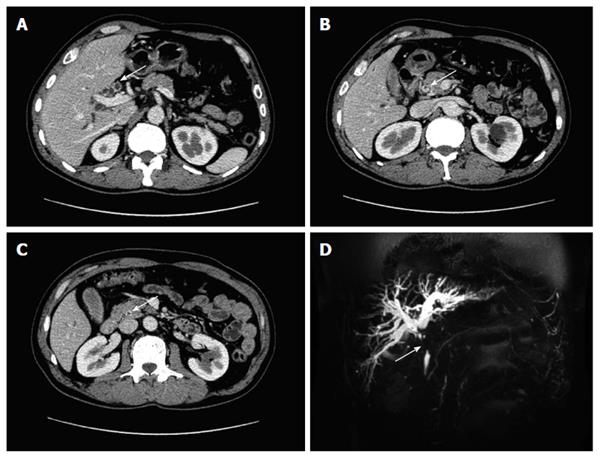
Figure 1 Enhanced computed tomography and magnetic resonance cholangiopancreatography findings related to the tumor.
A-C: Computed tomography scan revealed stenosis of the hepatic and upper common bile duct as well as irregular thickening of the common bile duct wall (white arrow); D: Magnetic resonance cholangiopancreatography showed obstruction of the common bile duct (white arrow).
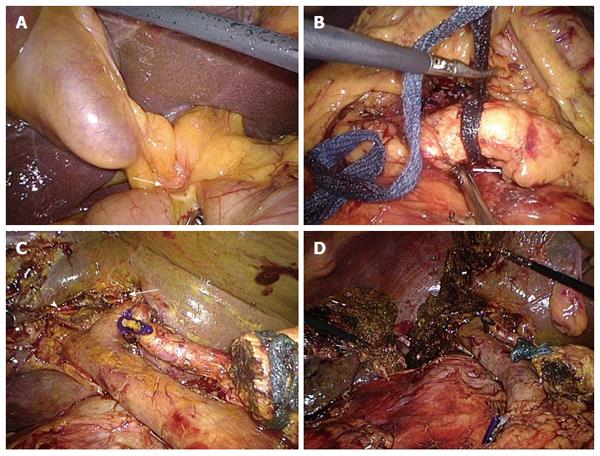
Figure 2 Key surgical steps of laparoscopic hepatopancreatoduodenectomy.
A: The duodenum was invaded by the tumor (white arrow); B: The inferior border of the pancreatic neck was dissected and a retropancreatic tunnel was created; C: The operative view after laparoscopic pancreaticoduodenectomy. The white arrow head indicates the opening of the right hepatic duct; arrow indicates the opening of the left hepatic duct; D: Laparoscopic hepatopancreatoduodenectomy was completed.
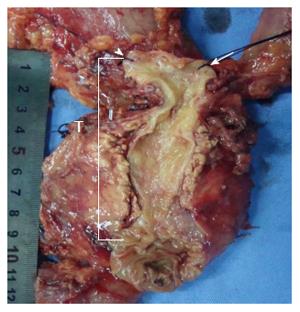
Figure 3 Resected specimen following laparoscopic pancreaticoduodenectomy.
Figure 4 Bile duct was opened from Vater's ampulla to the proximal duct stump.
Arrow head, left hepatic duct; arrow right, hepatic duct; T, the tumor had spread from the hepatic portal to the distal part of common bile duct 1.5 cm from Vater's ampulla.
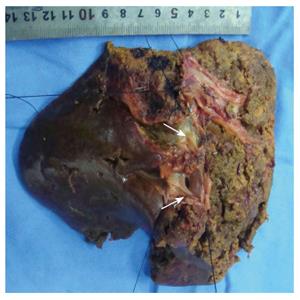
Figure 5 Specimen of laparoscopic right hemihepatectomy.
White arrows show the right anterior segmental duct and the right posterior segmental duct.
-
Citation: Zhang MZ, Xu XW, Mou YP, Yan JF, Zhu YP, Zhang RC, Zhou YC, Chen K, Jin WW, Matro E, Ajoodhea H. Resection of a cholangiocarcinoma
via laparoscopic hepatopancreato- duodenectomy: A case report. World J Gastroenterol 2014; 20(45): 17260-17264 - URL: https://www.wjgnet.com/1007-9327/full/v20/i45/17260.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i45.17260