©2014 Baishideng Publishing Group Inc.
World J Gastroenterol. Oct 14, 2014; 20(38): 13842-13862
Published online Oct 14, 2014. doi: 10.3748/wjg.v20.i38.13842
Published online Oct 14, 2014. doi: 10.3748/wjg.v20.i38.13842
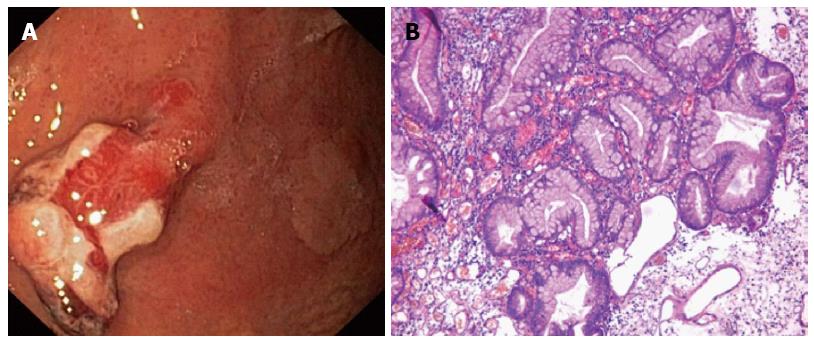
Figure 1 White light endoscopy of the stomach of a 60-year-old man.
A: Hyperplastic gastric polyp 40 mm × 20 mm in size is clearly visible in the foreground. The flat lesion in the background has been missed during first outpatient esophagogastroduodenoscopy; B: Pathomorphology after initial biopsy and polypectomy confirmed the hyperplastic nature of the polyp.
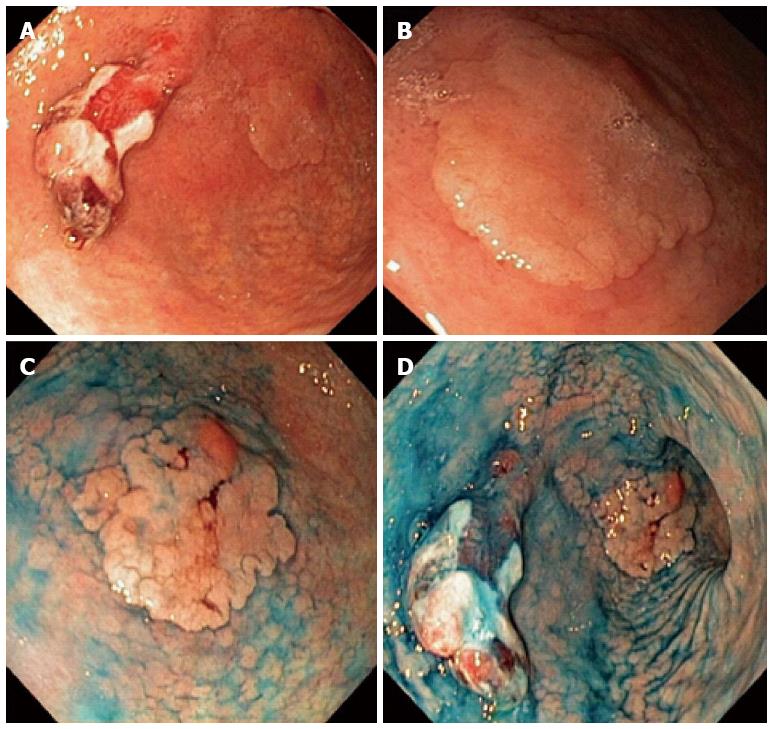
Figure 2 Esophagogastroduodenoscopy of the same patient.
A: The flat lesion in the background can been viewed more easily when better lit; B: Closer view of the superficial elevated lesion; C: After chromoendoscopy with indigo carmine - a roundish lesion 25 mm in diameter can be seen, with a smooth lobulated surface and a 6-mm, reddish protrusion in the distal part; type 0-IIa+Is according to Paris classification; D: Due to the marked inflammation and presence of intestinal metaplasia the precise proximal margin of the lesion is still unclear, even with the use of chromoendscopy.
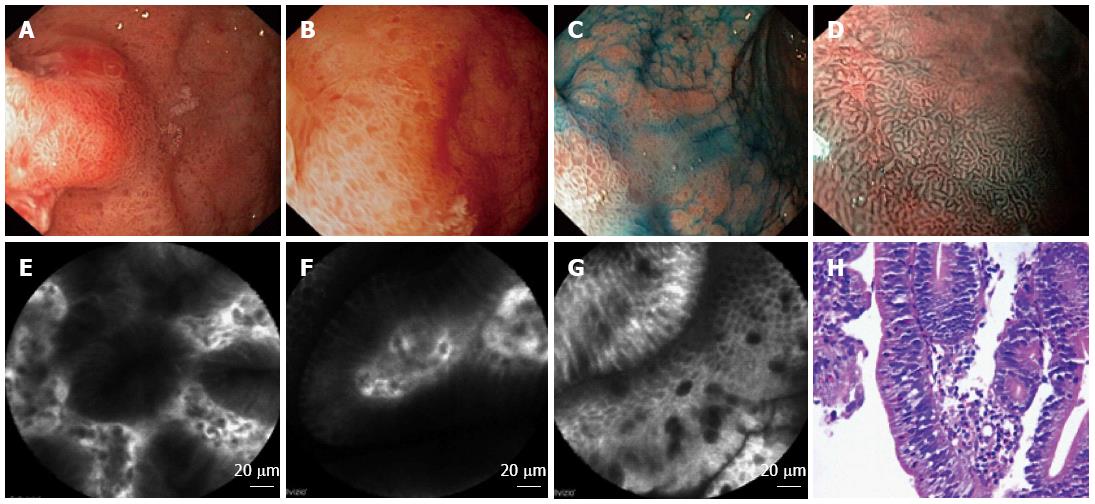
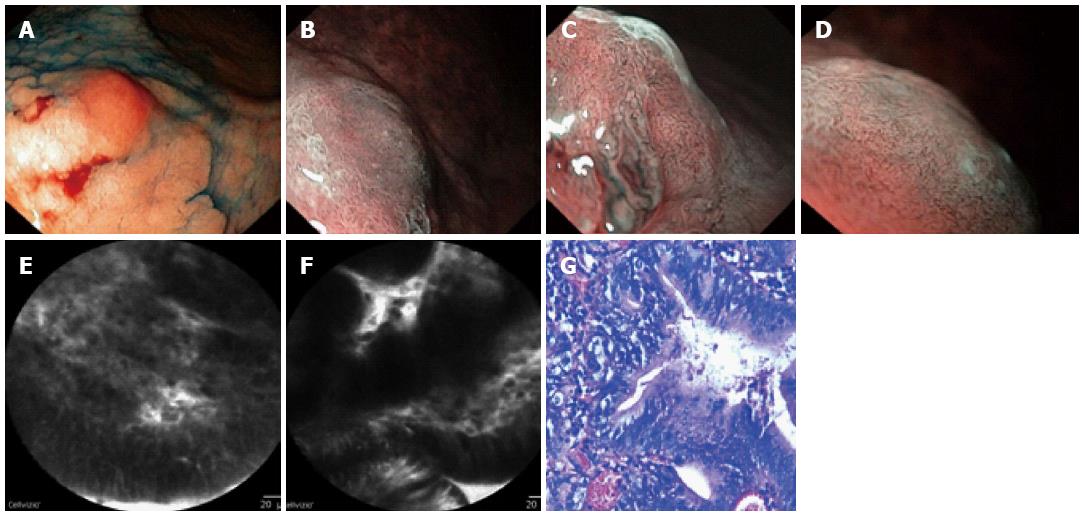
Figure 3 Characterization of the surrounding mucosa of the same patient.
A-C: WLE + chromoendoscopy: pronounced focal mucosal hyperemia, edema, petechiae, multiply foci of intestinal metaplasia; D: Narrow band imaging (NBI) + magnified endoscopy (zoom). The results, according to VS-classification[138]: the surrounding mucosa is inflamed, with a regular stick-like microsurface pattern, slightly irregular wavy microvascular pattern; E: Confocal laser endomicroscopy (CLE): A cross-section of normal glands; F: CLE: A longitudinal section of normal glands; G: CLE: Marks of intestinal metaplasia - Goblet cells; H: Pathomorphology: Active chronic Нр+ gastritis with incomplete intestinal metaplasia and low grade epithelial dysplasia.
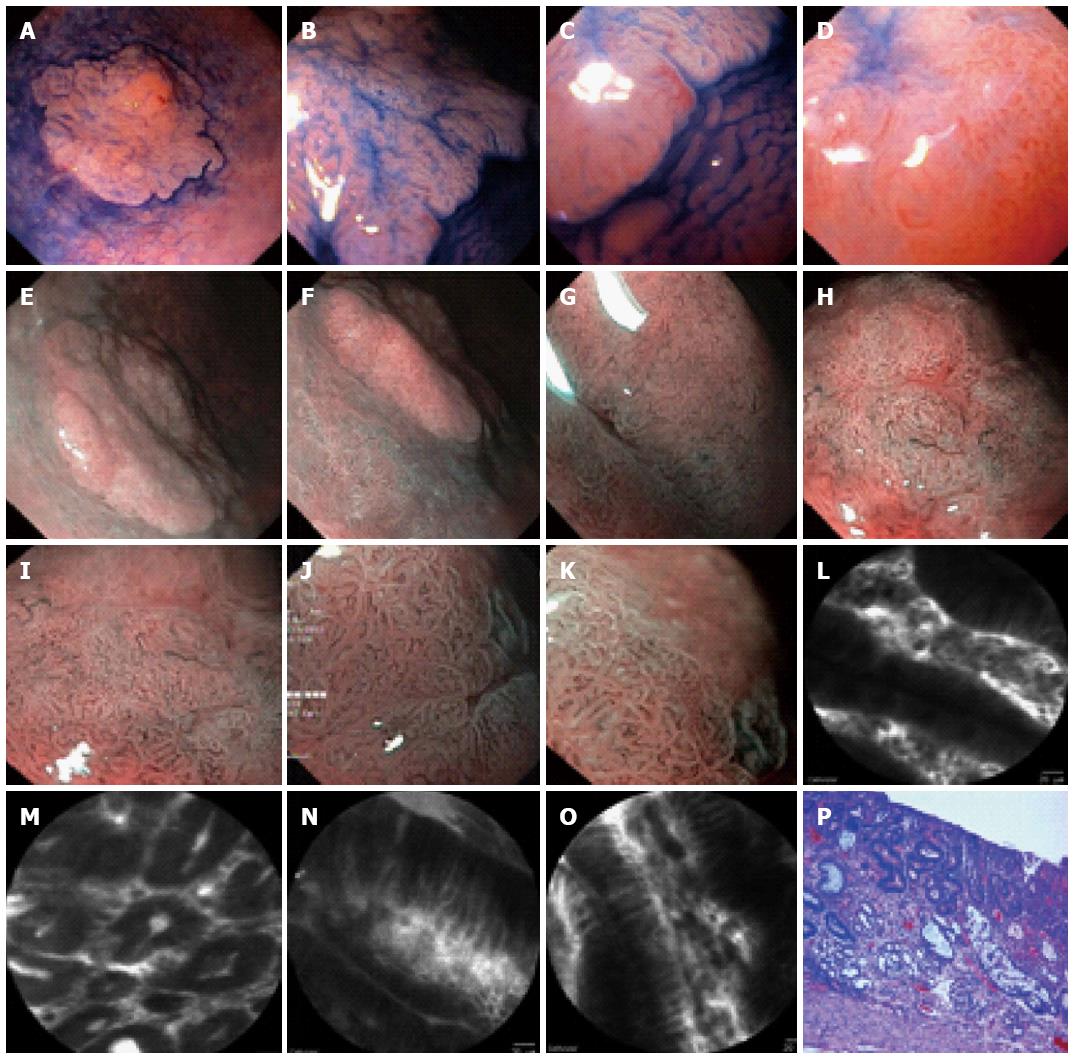
Figure 4 Some patient after 2 wk of Helicobacter pylori eradication therapy.
The characterization of the flat (IIa) part of the lesion type 0-IIa+Is is neoplastic: A-D: High definition Video-EGD + chromoendoscopy + Zoom: Shows a clear demarcation line between the lesion and surrounding mucosa; E-G: NBI + zoom: A clear demarcation line between the lesion and the surrounding mucosa; H, I: NBI + zoom: An irregular microsurface pattern - elongated and different in size and shape; J, K: An irregular microvascular pattern - tortuous, different in shape and size of the capillaries, forming an irregular network; L: CLE: Marks of intestinal metaplasia - Goblet cells; M: CLE: Deformed glands; N: CLE: Dark irregular glands; pseudostratified epithelium; O: CLE: Dark irregular glands; pseudostratified epithelium; P: Pathomorphology: Incomplete intestinal metaplasia and high grade dysplasia with foci of well-differentiated adenocarcinoma.
Figure 5 Some patient after 2 wk of Helicobacter pylori eradication therapy.
The characterization of the protruded (Is) part of the lesion type 0-IIa+Is is a differentiated adenocarcinoma. A: High definition Video-EGD + chromoendoscopy: A closer view of the protruded part of the lesion; B-D: Barrow-band imaging (NBI) + zoom: Unclear shredded microsurface pattern with an irregular network microvascular pattern - the capillaries differ in shape and diameter and are tortuous; E: Confocal laser endomicroscopy (CLE): Dark irregular glands; pseudostratified epithelium; irregularly shaped nuclei; F: CLE: Dark irregular glands; pseudostratified epithelium; G: Pathomorphology: A well-differentiated adenocarcinoma.
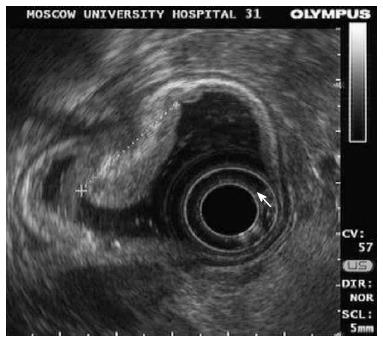
Figure 6 Same patient.
Endosonography of the lesion 0-IIa + Is. Area of the lesion (25 mm in size): Thickening of mucosa up to 5-7 mm; submucosal layer is clear under the tumor; lymph nodes are not visualized.
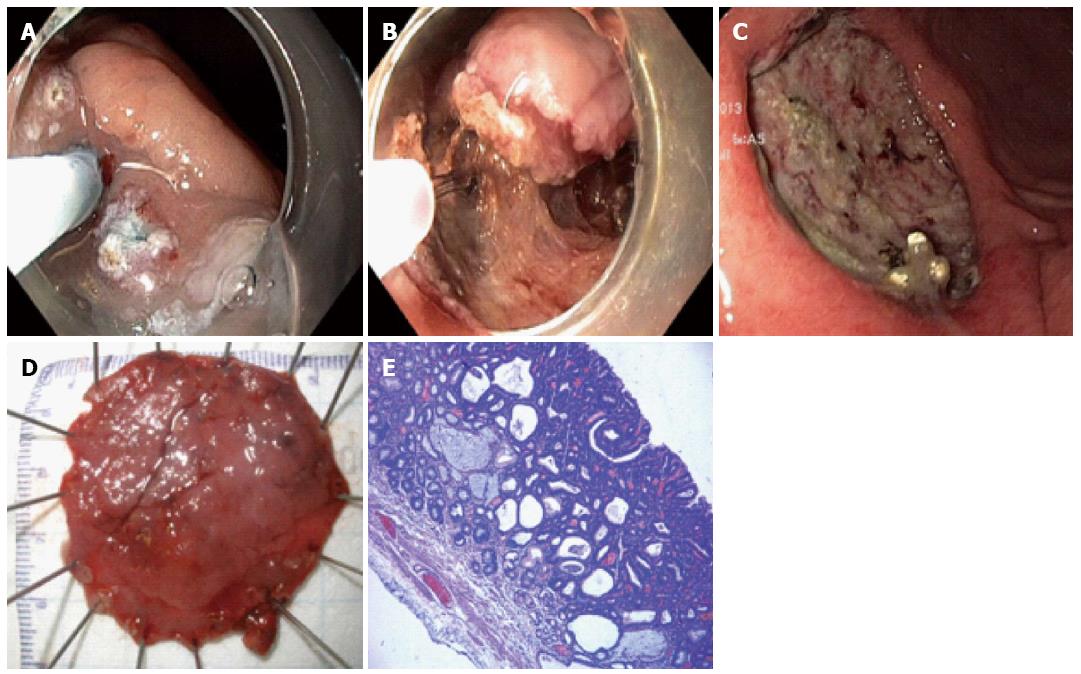
Figure 7 Same patient.
A-D: The lesion was removed en-block using triangle and IT-2 knives at endoscopic submucosal dissection without any complications; E: Well-differentiated adenocarcinoma no invasion in submucosa, clear horizontal and vertical margins, absence of vascular and lymphatic invasion.
- Citation: Pasechnikov V, Chukov S, Fedorov E, Kikuste I, Leja M. Gastric cancer: Prevention, screening and early diagnosis. World J Gastroenterol 2014; 20(38): 13842-13862
- URL: https://www.wjgnet.com/1007-9327/full/v20/i38/13842.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i38.13842