©2013 Baishideng Publishing Group Co.
World J Gastroenterol. May 28, 2013; 19(20): 3134-3142
Published online May 28, 2013. doi: 10.3748/wjg.v19.i20.3134
Published online May 28, 2013. doi: 10.3748/wjg.v19.i20.3134
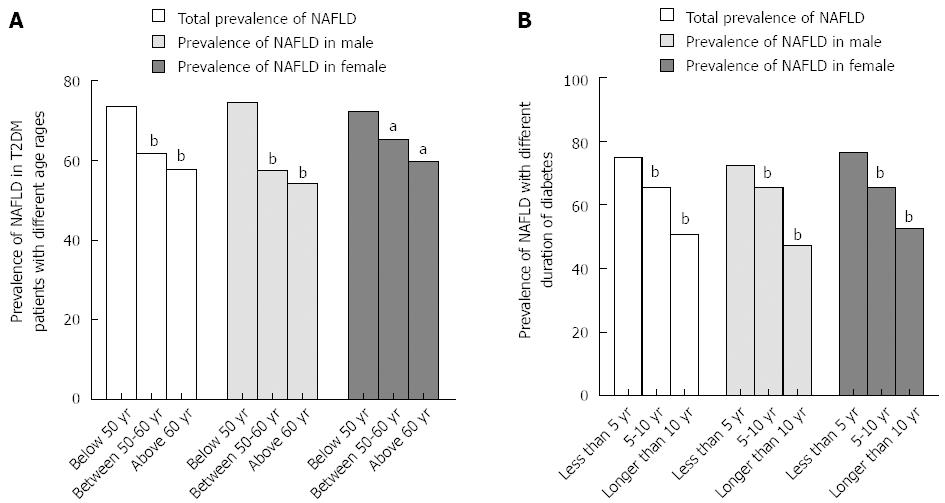
Figure 1 Prevalence of nonalcoholic fatty liver disease in type 2 diabetes mellitus patients according to different age ranges and durations of diabetes.
A: Prevalence of nonalcoholic fatty liver disease (NAFLD) in patients aged < 50, 50-60, and > 60 years was 73.4%, 61.6%, and 57.8%, respectively, indicating that the prevalence of NAFLD decreased significantly with increasing age (bP < 0.01 vs group below 50 years). In men (74.5%, 57.5%, and 54.2%, respectively, bP < 0.01 vs group below 50 years) and women (72.3%, 65.1%, and 59.6%, respectively, aP < 0.05 vs group below 50 years), the prevalence of NAFLD decreased significantly with increasing age. The prevalence of NAFLD in men was higher than in women (74.5% and 72.3%, respectively, P > 0.05) in the < 50 years age group; however, the reverse was evident in the > 50 years age group (57.5% and 65.1%, respectively, in the 50-60 years age group, and 54.2% and 59.6%, in the > 60 years age group, both P > 0.05); B: Prevalence of NAFLD, according to duration of diabetes, was 74.9%, 65.5%, and 50.7% for < 5, 5-10, and > 10 years, respectively. Prevalence of NAFLD decreased significantly with prolonged course of diabetes (bP < 0.01 vs group less than 5 years). This trend persisted even when patients were stratified by sex (72.3%, 65.6%, and 47.1%, respectively, in men, and 76.5%, 65.4%, and 52.6% in women, bP < 0.01 vs group less than 5 years). There were no significant differences in the prevalence of NAFLD between men and women with different durations of diabetes (P > 0.05). T2DM: Type 2 diabetes mellitus.
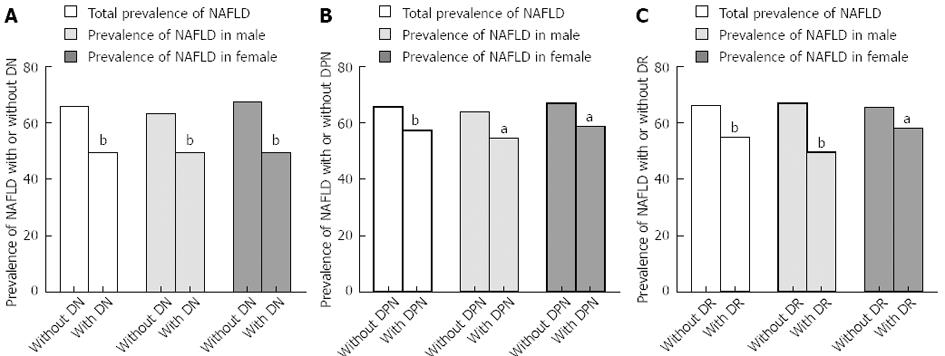
Figure 2 Prevalence of nonalcoholic fatty liver disease in T2DM with or without microangiopathy complications.
A: Incidence of nonalcoholic fatty liver disease (NAFLD) negatively correlated with DN (r = -0.154, P < 0.05). This trend persisted even when patients were stratified by sex (r = -0.13 in men, r = -0.17 in women, both P < 0.05). Prevalence of NAFLD in T2DM with and without DN was 49.4% and 65.9%, respectively (bP < 0.01 vs group without DN). Prevalence of NAFLD in men without DN was significantly higher than in patients with DN (63.3% and 49.3%, respectively, bP < 0.01 vs the group without DN). Prevalence of NAFLD in women without DN was significantly higher than in patients with DN (67.5% and 49.5%, respectively, bP < 0.01 vs the group without DN); B: Incidence of NAFLD negatively correlated with DPN (r = -0.086, P < 0.05). This trend persisted even when patients were stratified by sex (r = -0.095 in men, r = -0.084 in women, both P < 0.05). The general prevalence of NAFLD in T2DM with and without DPN was 57.2% and 65.6%, respectively (bP < 0.01 vs the group without DPN). Prevalence of NAFLD in men without DPN was significantly higher than in patients with DPN (63.9% and 54.5%, respectively, aP < 0.05 vs the group without DPN). Prevalence of NAFLD in women without DPN was also significantly higher than that in patients with DPN (66.9% and 58.6%, respectively, aP < 0.05 vs the group without DPN); C: Incidence of NAFLD negatively correlated with DR (r = -0.114, P < 0.05). This trend persisted even when patients were stratified by sex (r = -0.176 in men, r = -0.076 in women, both P < 0.05). Prevalence of NAFLD in T2DM with and without DR was 54.9% and 66.1%, respectively (bP < 0.01 vs the group without DR). Furthermore, the Prevalence of NAFLD in men without DR was significantly higher than that in patients with DR (66.9% and 49.5%, respectively, bP < 0.01 vs the group without DR). Prevalence of NAFLD in women without DR was also significantly higher than that in patients with DR (65.5% and 58.1%, respectively, aP < 0.05 vs the group without DR).
- Citation: Lv WS, Sun RX, Gao YY, Wen JP, Pan RF, Li L, Wang J, Xian YX, Cao CX, Zheng M. Nonalcoholic fatty liver disease and microvascular complications in type 2 diabetes. World J Gastroenterol 2013; 19(20): 3134-3142
- URL: https://www.wjgnet.com/1007-9327/full/v19/i20/3134.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i20.3134