©2013 Baishideng Publishing Group Co.
World J Gastroenterol. May 14, 2013; 19(18): 2826-2829
Published online May 14, 2013. doi: 10.3748/wjg.v19.i18.2826
Published online May 14, 2013. doi: 10.3748/wjg.v19.i18.2826
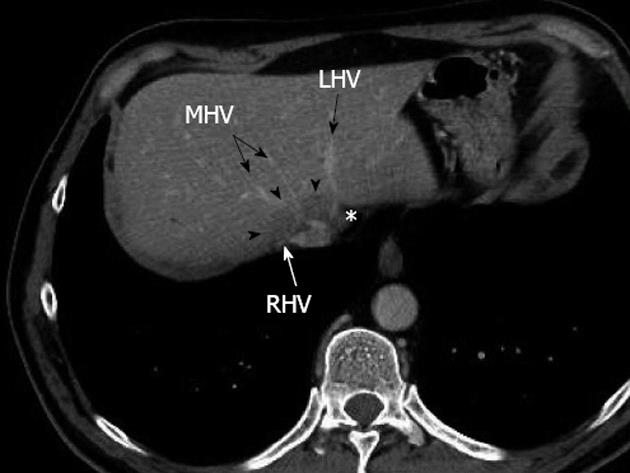
Figure 1 Preoperative multidetector computed tomograph at portal venous phase showing a large metastasis (arrowheads) encircling the confluence of the right hepatic vein and middle hepatic vein, without any thrombosis, and displacing the end of the left hepatic vein (asterisk).
RHV: Right hepatic vein; MHV: Middle hepatic vein; LHV: Left hepatic vein.
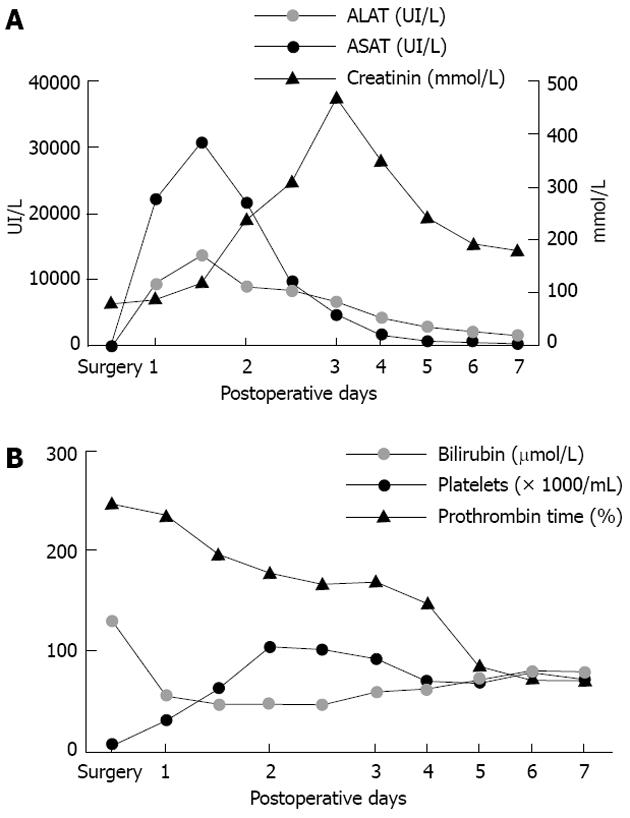
Figure 2 Postoperative blood tests.
A: Transaminases increased from postoperative day 1, reached a peak at postoperative day 3, then returned to normal value on postoperative day 7. Serum creatinin started to increase after the peak of transaminases, as observed in the toxic liver syndrome, and decreased after hemofiltration; B: Platelets decreased regularly as from the first postoperative day. Total bilirubin increased from the first postoperative day and reached a plateau around 100 μmol/L. Prothrombin time fell rapidly to 47% at postoperative day 1 and thereafter increased progressively. ASAT: Aspartate amino transferase; ALAT: Alanine amino transferase.
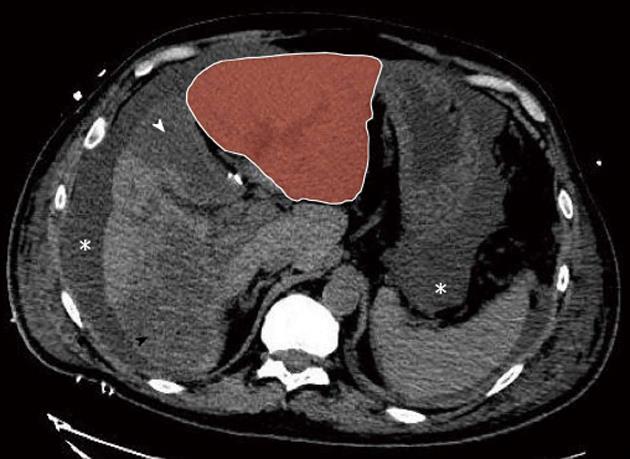
Figure 3 Postoperative day 2 non-enhanced multidetector computed tomograph scan.
Massive hepatic necrosis of the medial segment of the left lobe (segment 4, white arrowhead) and of a large part of the right lobe (black arrowhead) are shown, with remarkable hypertrophy of the lateral segments of the left lobe (red zone). Note also ascites (asterisk).
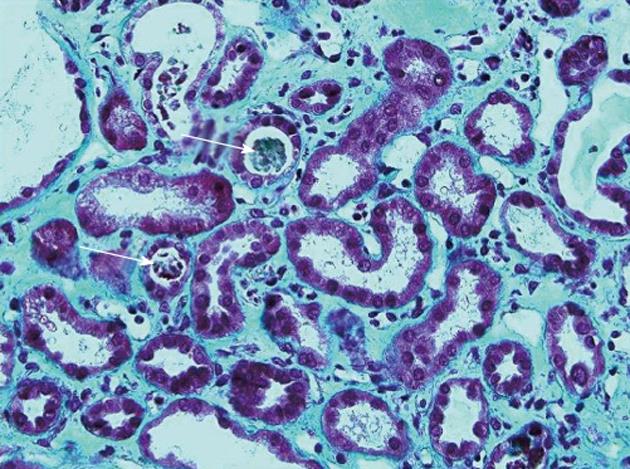
Figure 4 Renal biopsy showing acute tubular necrosis: Tubules dilated with sometimes a low-lying epithelium and pleomorphic nuclei.
The brush border of the proximal tubular cells is missing. The lumen of some tubules contains rare tubular cell necrosis (white arrows). There is a diffuse interstitial edema (Masson’s trichrome, ×40).
- Citation: Dupré A, Gagnière J, Tixier L, Ines DD, Perbet S, Pezet D, Buc E. Massive hepatic necrosis with toxic liver syndrome following portal vein ligation. World J Gastroenterol 2013; 19(18): 2826-2829
- URL: https://www.wjgnet.com/1007-9327/full/v19/i18/2826.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i18.2826