©2012 Baishideng Publishing Group Co.
World J Gastroenterol. Oct 21, 2012; 18(39): 5640-5644
Published online Oct 21, 2012. doi: 10.3748/wjg.v18.i39.5640
Published online Oct 21, 2012. doi: 10.3748/wjg.v18.i39.5640
Figure 1 Selective upper mesenteric artery angiogram showing severe incomplete thrombosis with more than a 75% reduction of the arterial lumen and poor perfusion of the bowel loop.
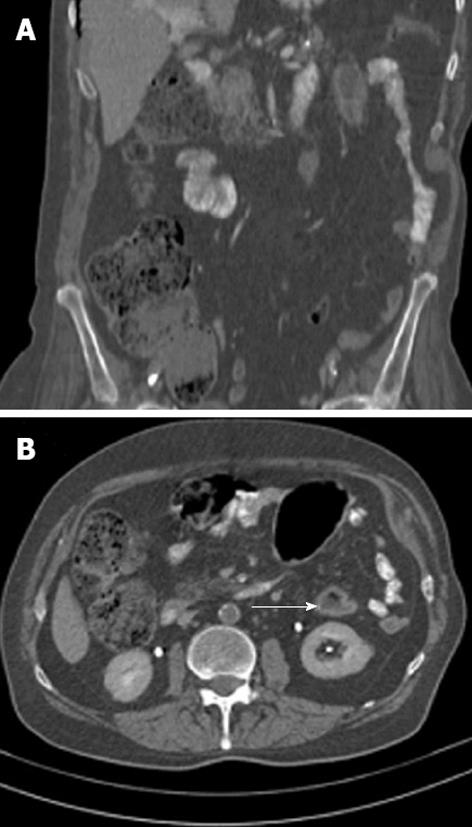
Figure 2 Contrast-enhanced abdominal computed tomography scans suggesting segmental colitis involving the splenic flexure and the descending colon.
A: Coronal sections with zones of mural thickening of the colon just below the splenic flexure and a long and narrow axial stenosis of the descending colon; B: Sagittal sections showing (arrow) the "double halo" sign, a tomographic equivalent of the classic “thumbprinting” that is observed in barium enemas.
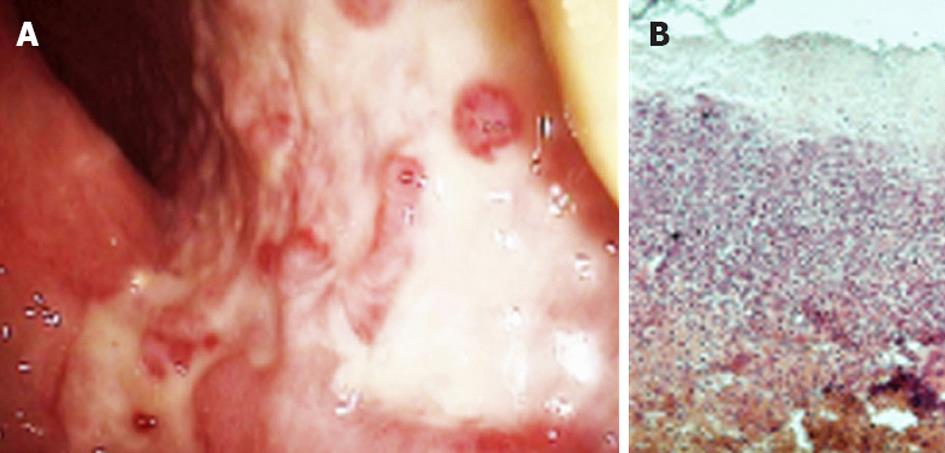
Figure 3 Morphologic changes confirming ischemic colitis by lower digestive endoscopy and histology.
A: Areas of mucosal ulceration, pseudomembranes and subsequent granulation observed at colonoscopy; B: Biopsy specimens from affected areas showing submucosal necrosis, inflammatory infiltration, cryptal atrophy and hyalinization. Hematoxylin-eosin staining, ×100. Courtesy Dr. Simionescu.
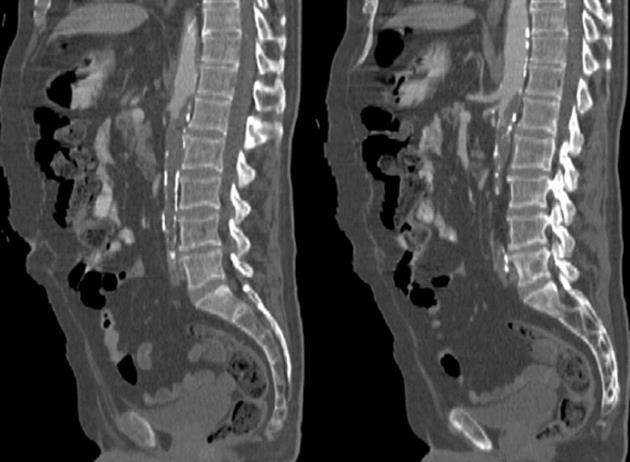
Figure 4 Calcification of the abdominal aorta with extensive thrombosis inside, which completely obstructed the lumen below the 2nd lumbar vertebra.
Note that the celiac trunk and upper mesenteric artery are spared, whereas the lower mesenteric is completely occluded.
- Citation: Georgescu EF, Carstea D, Dumitrescu D, Teodorescu R, Carstea A. Ischemic colitis and large bowel infarction: A case report. World J Gastroenterol 2012; 18(39): 5640-5644
- URL: https://www.wjgnet.com/1007-9327/full/v18/i39/5640.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i39.5640