©2010 Baishideng.
World J Gastroenterol. Jan 28, 2010; 16(4): 513-517
Published online Jan 28, 2010. doi: 10.3748/wjg.v16.i4.513
Published online Jan 28, 2010. doi: 10.3748/wjg.v16.i4.513
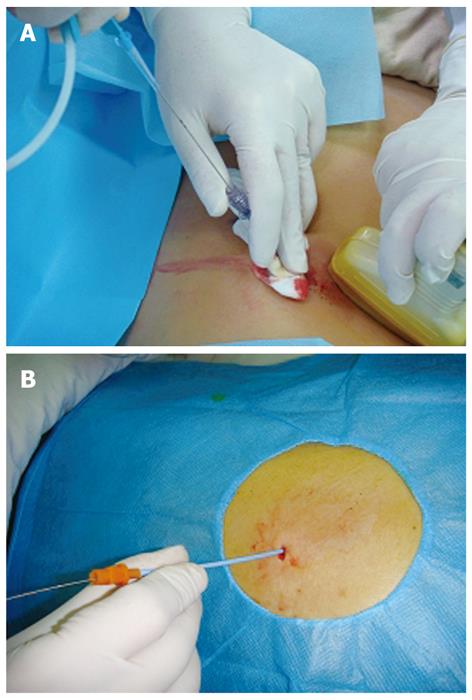
Figure 1 Ultrasound-guided percutaneous puncture and catheter drainage.
A: An 18-G puncture needle is inserted into the peripancreatic focus under the guidance of ultrasound with a guidewire placed in the focus through the puncture needle lumen; B: An 8-Fr drainage catheter is immediately delivered into the focus along the guidewire after adequate expansion of abdominal wall layers.
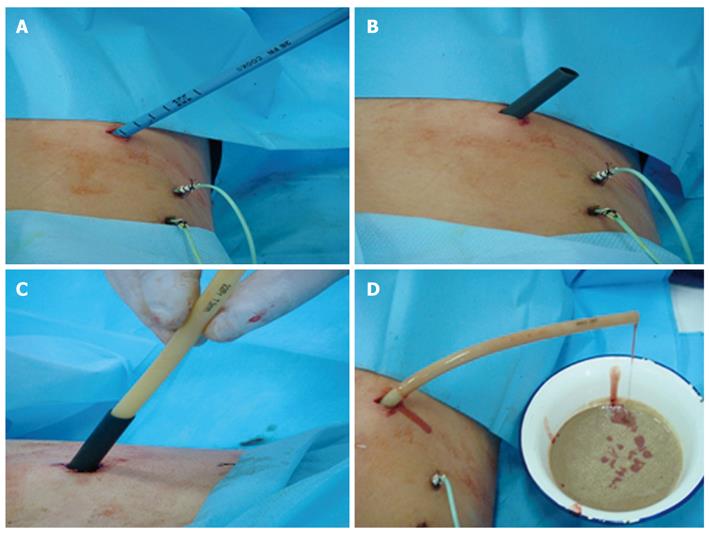
Figure 2 Replacement of the drainage catheter with a larger-diamete drainage tube.
A: Gradual expansion of the drainage catheter sinus tract using different Fr skin expanders along with the guidewire; B: Pulling out the expander with its sheath left in the focus after insertion of a sheath matching the 24-Fr skin expander into the focus; C: Insertion of a 22-Fr drainage tube into the focus through the sheath lumen of a skin expander; D: Left in the focus.
Figure 3 Debridement guided by choledochoscope.
Formation of sinus tract around the drainage tube (A) with a choledochoscope slowly inserted into the focus through the sinus tract (B) 7 d after drainage with a large drainage tube, flushing of accumulated pus and necrotic tissue fragments from the foci of SAP by injecting a large amount of sterile saline and 0.5% metronidazole into the infected foci via the water inlet of choledochoscope (C).
- Citation: Tang LJ, Wang T, Cui JF, Zhang BY, Li S, Li DX, Zhou S. Percutaneous catheter drainage in combination with choledochoscope-guided debridement in treatment of peripancreatic infection. World J Gastroenterol 2010; 16(4): 513-517
- URL: https://www.wjgnet.com/1007-9327/full/v16/i4/513.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i4.513