©2006 Baishideng Publishing Group Co.
World J Gastroenterol. Jun 14, 2006; 12(22): 3546-3552
Published online Jun 14, 2006. doi: 10.3748/wjg.v12.i22.3546
Published online Jun 14, 2006. doi: 10.3748/wjg.v12.i22.3546
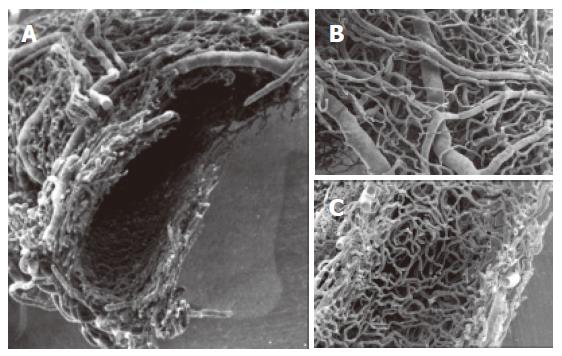
Figure 1 SEMvcc of normal rat liver (orig.
magn., 20×). A dense vascular network is arranged around the circumference of the common bile duct. A: transverse section of Extrahepatic peribiliary plexus. Observe the arterial and venous vessels on the outer layer (B) and a dense capillary network in the inner layer of the plexus (C).
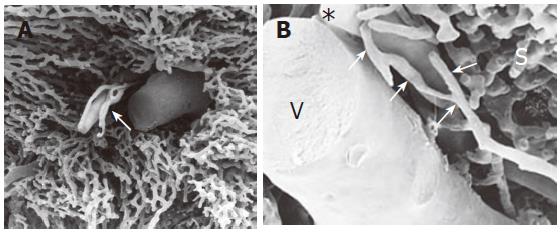
Figure 2 SEMvcc of normal rat liver (orig.
magn., A: 40×; B: 110×). (A) small portal tract: PBP is characterized by a single layer of capillaries. (B) * = terminal hepatic artery, V = vena porta, arrows = peribiliary plexus, S = sinusoids.
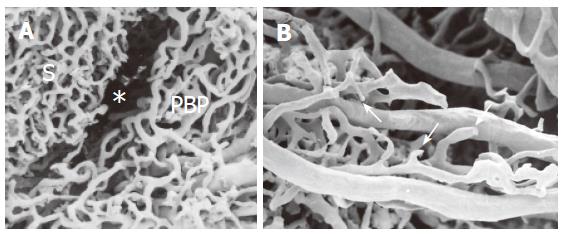
Figure 3 SEMvcc of BDL rat liver (orig.
magn., A: 40×; B: 60×). (A) proliferated PBP run at the periphery of the lobule separated from the sinusoidal network (S) by an empty space (*) which corresponds to proliferating connective tissue. (B) not completely developed PBP with typical neovascular organization with dead end vessels (arrows).
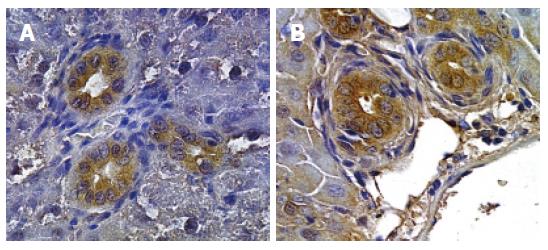
Figure 4 Immunohistochemistry for VEGF-A (A) and VEGF-C (B).
Proliferating bile ducts in BDL rat show an intense positivity for both VEGF-A and VEGF-C (Orig. magn., 20×).
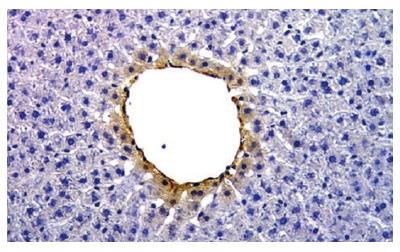
Figure 5 Immunohistochemistry for VEGF-A.
Normal rat liver. The hepatocyte of pericentral zone shows positivity for VEGF-A (Orig. magn., 20×).
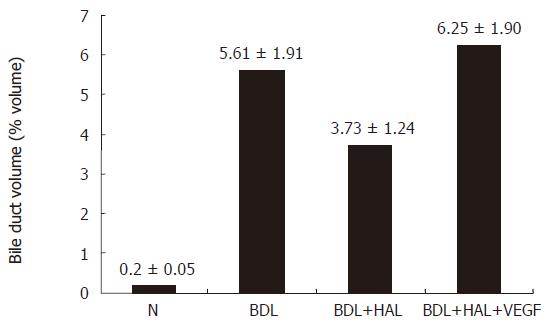
Figure 6 Effect of hepatic artery ligation and chronic administration of VEGF on bile duct volume.
Bile Duct volume is measured as a volume fraction of the entire liver tissue specimen. HAL induced in BDL rats a disappearance of PBP and an impaired cholangiocyte proliferation. The effects of HAL on PBP and cholangiocyte functions were prevented by r-VEGF by maintaining the integrity of the peribiliary plexus and cholangiocyte proliferation.
- Citation: Gaudio E, Franchitto A, Pannarale L, Carpino G, Alpini G, Francis H, Glaser S, Alvaro D, Onori P. Cholangiocytes and blood supply. World J Gastroenterol 2006; 12(22): 3546-3552
- URL: https://www.wjgnet.com/1007-9327/full/v12/i22/3546.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i22.3546