©The Author(s) 2004.
World J Gastroenterol. Nov 15, 2004; 10(22): 3322-3327
Published online Nov 15, 2004. doi: 10.3748/wjg.v10.i22.3322
Published online Nov 15, 2004. doi: 10.3748/wjg.v10.i22.3322
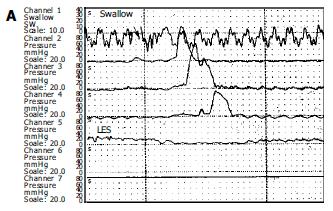
Figure 1 Manometric samples from a normal individual (A) and a patient with achalasia (B).
Figure A illustrates the normal peristaltic activity forwarding at cranio-caudal direction whereas figure B shows typical manometric findings of achalasia. Note the aperistalsis, weak and simultaneous contractions (mirror sign), and incomplete LES relaxation after swallow. Basal LES pressure is high (40 mmHg).
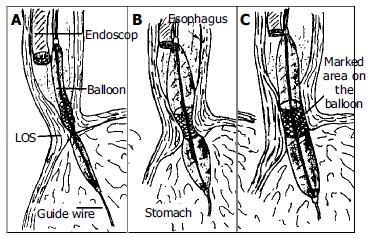
Figure 2 Technique for pneumatic dilatation under endoscopic control without fluoroscopy.
The balloon was positioned so that its midsection was at the high pressure level (A). The balloon was inflated and the endoscopist observes with endoscope proximally to balloon (B). With successful dilatation the ischemic ring of dilated segment was diminished or disappeared (C).
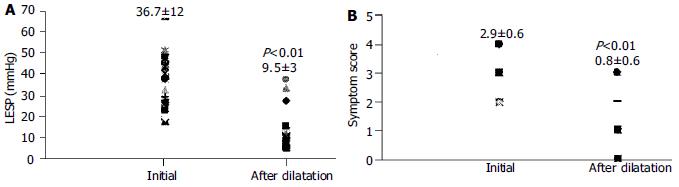
Figure 3 Lower esophageal sphincter pressures (LESP) (A) and symptom scores (B) of patients with therapeutic response initially and at one month after pneumatic dilatation.
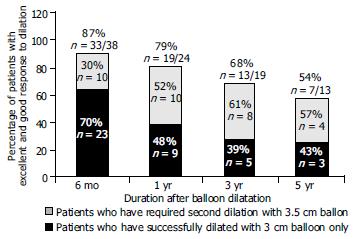
Figure 4 Percentage of patients with excellent and good response to dilatation at 6 mo, 1, 3 and 5 years.
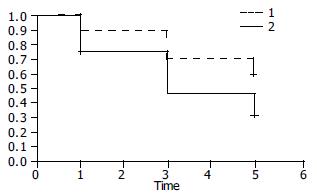
Figure 5 Kaplan-Meier plot for the two treatment groups of patients who were dilated once2 or twice1.
The cumulative one, three and five year remission rates were higher in patients dilated twice but this difference was not statistically significant (Log-rank χ2 = 2.10, P = 0.1471).
- Citation: Dobrucali A, Erzin Y, Tuncer M, Dirican A. Long-term results of graded pneumatic dilatation under endoscopic guidance in patients with primary esophageal achalasia. World J Gastroenterol 2004; 10(22): 3322-3327
- URL: https://www.wjgnet.com/1007-9327/full/v10/i22/3322.htm
- DOI: https://dx.doi.org/10.3748/wjg.v10.i22.3322