Published online Jun 8, 2024. doi: 10.37126/aige.v5.i2.92090
Revised: February 11, 2024
Accepted: April 7, 2024
Published online: June 8, 2024
Processing time: 117 Days and 1.8 Hours
Virtual reality (VR) has emerged as an innovative technology in endoscopy training, providing a simulated environment that closely resembles real-life scenarios and offering trainees a valuable platform to acquire and enhance their endoscopic skills. This systematic review will critically evaluate the effectiveness and feasibility of VR-based training compared to traditional methods.
To evaluate the effectiveness and feasibility of VR-based training compared to traditional methods. By examining the current state of the field, this review seeks to identify gaps, challenges, and opportunities for further research and implemen-tation of VR in endoscopic training.
The study is a systematic review, following the guidelines for reporting syste
Sixteen articles were included in the final analysis. The total number of participants was 523. Five studies focused on both upper endoscopy and colonoscopy training, two on upper endoscopy training only, eight on colon-oscopy training only, and one on sigmoidoscopy training only. Gastro-intestinal Mentor virtual endoscopy simulator was commonly used. Fifteen reported positive results, indicating that VR-based training was feasible and acceptable for endoscopy learners. VR technology helped the trainees enhance their skills in manipulating the endoscope, reducing the procedure time or increasing the technical accuracy, in VR scenarios and real patients. Some studies show that the patient discomfort level decreased significantly. However, some studies show there were no significant differences in patient discomfort and pain scores between VR group and other groups.
VR training is effective for endoscopy training. There are several well-designed randomized controlled trials with large sample sizes, proving the potential of this innovative tool. Thus, VR should be more widely adopted in endoscopy training. Furthermore, combining VR training with conventional methods could be a promising approach that should be implemented in training.
Core Tip: Virtual reality (VR) is a promising tool in endoscopy training. This systematic review assessed VR's effectiveness and feasibility. Sixteen articles were analyzed, with 15 reporting positive results. VR training enhanced endoscopy skills, reducing procedure time and increasing accuracy in both VR scenarios and real patients. Patient discomfort also decreased significantly. VR training is effective and should be widely adopted in endoscopy training. Combining VR with conventional methods could further enhance training.
- Citation: Dương TQ, Soldera J. Virtual reality tools for training in gastrointestinal endoscopy: A systematic review. Artif Intell Gastrointest Endosc 2024; 5(2): 92090
- URL: https://www.wjgnet.com/2689-7164/full/v5/i2/92090.htm
- DOI: https://dx.doi.org/10.37126/aige.v5.i2.92090
The coronavirus disease 2019 pandemic has affected various domains of our lives, such as work, communication and education. In medical training, despite the difficulties it has posed, it has also opened up new possibilities. In addition to conventional methods, alternative forms of training are required to cope with the unprecedented situation of the pandemic. Furthermore, the rising demand for high-quality, safe medical care and the expectation of patient satisfaction have exposed the limitations of traditional medical training. Thus, the necessity of incorporating more innovative approaches to address the unmet need is evident.
Virtual reality (VR) is a simulated experience that can be like or completely different from the real world. It is achieved by using computer-generated images or sounds that create an immersive and interactive environment for the user. VR creates a 3D environment that enables users to explore and interact with virtual surroundings in a way that approximates reality, as it is perceived through the users' senses, with special devices, such as a headset, gloves, goggles, and controllers. The simulated environment is developed with advanced computer hardware and software.
Because of these unique features, VR has its advantages and disadvantages. Firstly, it can provide an immersive experience that can enhance the enjoyment and engagement of the user. For example, VR can be used for gaming, movies, and social networking, where users can feel part of the virtual world. Secondly, VR can increase productivity and efficiency by creating a distraction-free environment for work or learning. Finally, VR offers medical therapy and treatment applications for various conditions and disorders.
However, VR has some disadvantages. One drawback is that it requires expensive equipment and software that may not be accessible or affordable for everyone. Next, it can cause health risks such as nausea, dizziness, eye strain, headaches, and motion sickness, also known as VR sickness. Moreover, if VR is overused, it may lead to social isolation and addiction by reducing the interaction with the natural world and people. This can lead to losing social skills, empathy, and emotional connection.
With its unique features, VR application in medical training is an ideal innovative approach that could be used to meet the urgent needs of medical training lately. VR has been increasingly used in various fields of medical education and training, such as anatomy, communication skills, physical examinations, procedures, surgeries or diagnostic imaging feedback. VR enables learners to practice their skills in realistic and risk-free situations, improve their confidence, and obtain immediate feedback. VR can also reduce the costs and limitations of using physical models, cadavers, or live patients. Furthermore, VR can also facilitate collaborative and adaptive learning, as multiple learners can interact with each other and the virtual environment in real time. According to several studies, VR can enhance the learning outcomes, motivation, engagement and retention of medical students and professionals. Moreover, VR can provide opportunities for practicing complex and rare scenarios in a safe and controlled setting, without risking patient safety or ethical issues[1-4].
VR has emerged as an innovative technology in endoscopy training, providing a simulated environment that closely resembles real-life scenarios and offering trainees a valuable platform to acquire and enhance their endoscopic skills. Several studies have highlighted the potential benefits of VR-based training in gastrointestinal endoscopy[5]. VR simulation training provides a realistic, immersive, controlled, and highly interactive experience, allowing trainees to practice endoscopic procedures[6]. It has been shown to reduce procedural errors, improve polyp detection rates, and shorten the learning curve. Furthermore, VR-based endoscopy training has positively improved adverse events and enhanced patient safety[7].
Furthermore, VR training can boost the psychomotor skills of the trainees, which involve coordination, dexterity, and precision of movements[8]. VR training can also improve the quality of the endoscopic study, which is determined by factors such as bowel preparation, visualization, and documentation[9]. Additionally, VR training can help the trainees to correctly identify pathologies during the procedure, which is essential for diagnosis and treatment[10,11]. VR training can also reduce the adverse events that may occur during or after the procedure, such as perforation, bleeding, infection, or cardiopulmonary complications[8,9]. Finally, VR training can enhance the skill test performance of the trainees, which is a way to assess their technical and cognitive success in performing endoscopy[11,12].
Current American Council for Graduate Medical Education (ACGME) training guidelines mandate incorporating simulation training into gastroenterology fellowship programs. While simulation can potentially reduce training costs as staff endoscopists are more productive when performing procedures independently, there are costs associated with acquiring and maintaining simulators. It is therefore essential to ensure that skills gained through simulation training positively transfer to the clinical environment[13].
According to the current guidelines established by the ACGME, gastroenterology fellowship programs must include simulation training as part of their curriculum[13]. This study aims to evaluate the effectiveness and feasibility of VR-based training compared to traditional methods. By examining the current state of the field, this review seeks to identify gaps, challenges, and opportunities for further research and implementation of VR in endoscopic training.
This study is a systematic review following the guidelines for reporting systematic reviews set out by the PRISMA statement[14].
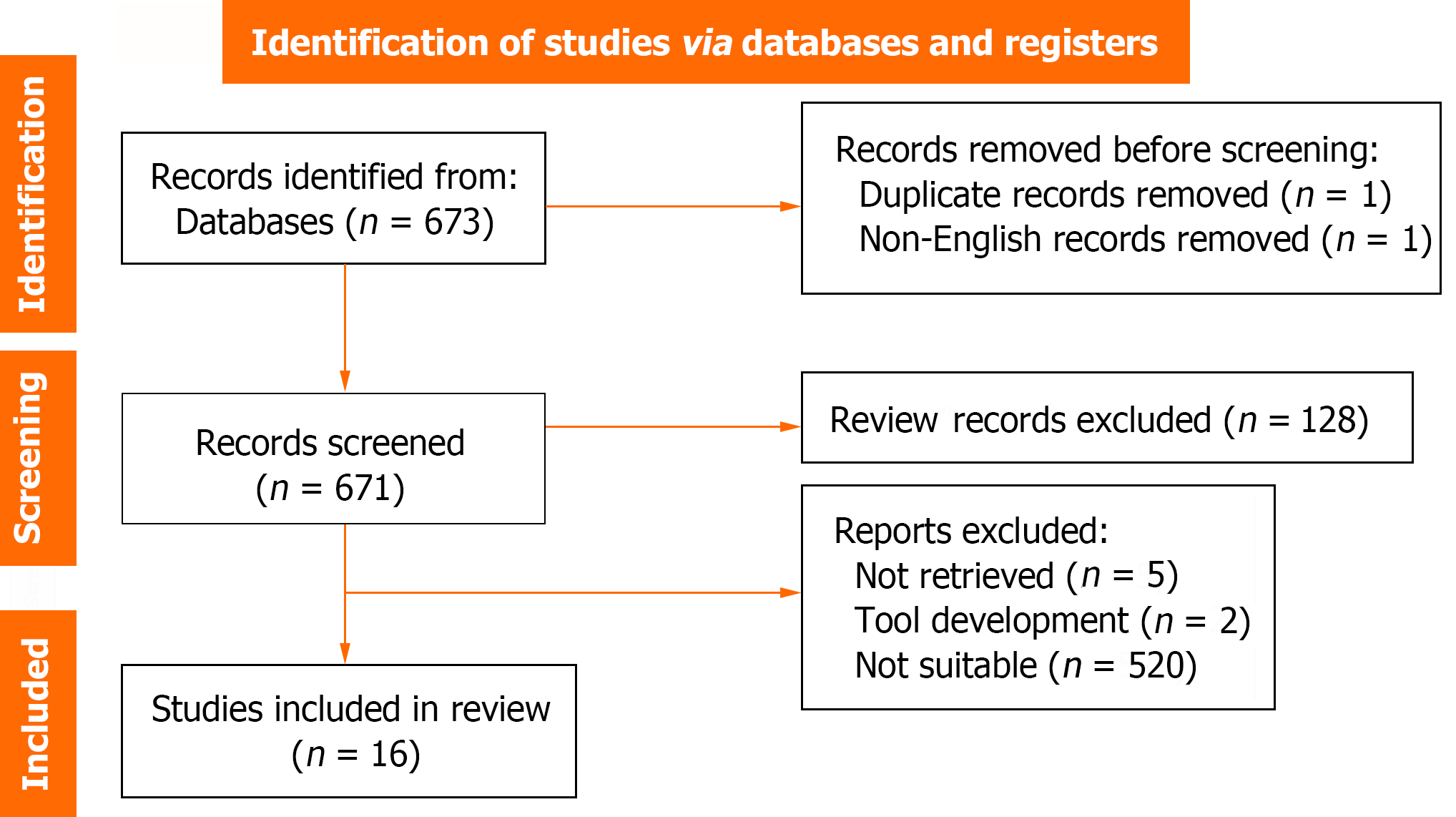
A comprehensive search command was designed and implemented to identify relevant studies from electronic databases, including PubMed, Scopus, Cochrane, and Google Scholar, to achieve the stated objectives. A total of 673 articles were found after running the following search on 11 September 2023: ("virtual reality" OR "computer simulation" OR "virtual training" OR "virtual simulation" OR "Cyberspace" OR "simulation training") AND ("training" OR "teaching" OR "learning") AND ("digestive endoscopy" OR "colonoscopy" OR "endoscopy").
The search utilized predefined keywords related to simulation-based training, VR, gastrointestinal endoscopy, training, and simulation.
The inclusion criteria encompassed studies published in peer-reviewed journals that evaluate the use of VR for training in gastrointestinal endoscopy and report outcomes related to endoscopic skills or patient outcomes. Studies not available in English and those without relevant outcomes related to endoscopic skills or patient outcomes were excluded.
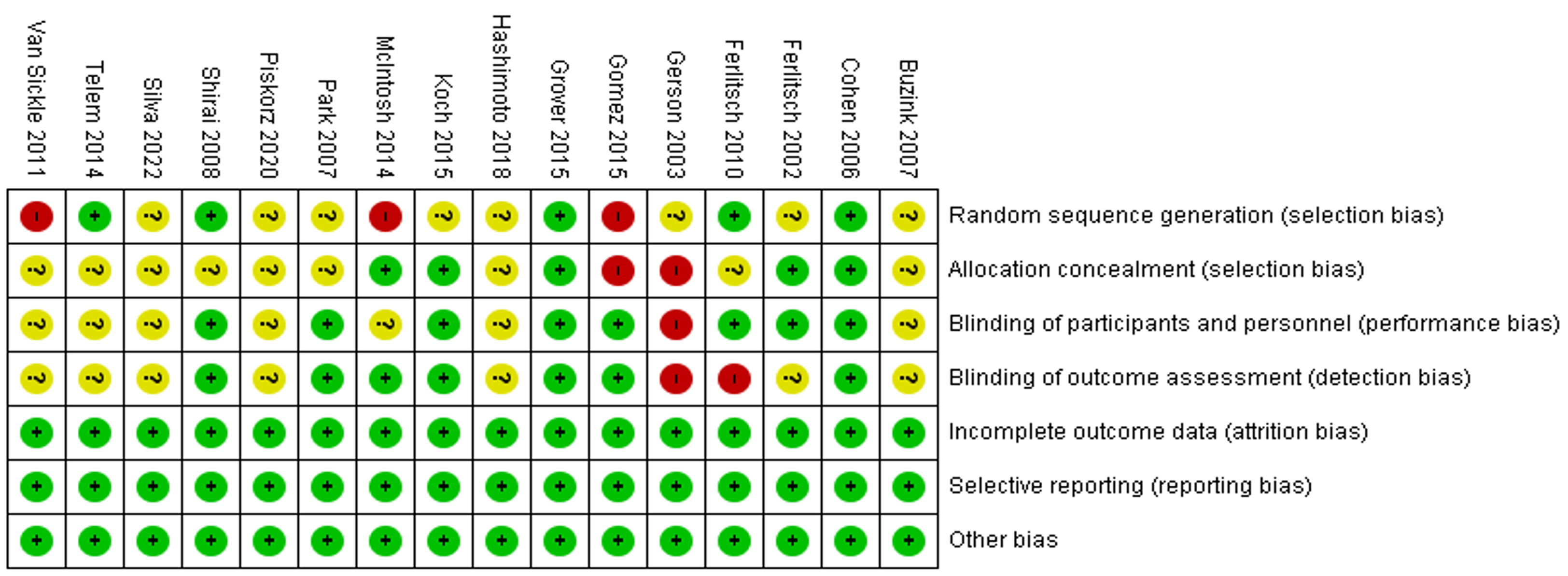
The screening process involved the reviewers assessing the titles and abstracts of the identified studies for potential eligibility based on the inclusion and exclusion criteria. Full-text articles of potentially eligible studies were retrieved and assessed for final inclusion. The study selection process was documented using a flowchart following the PRISMA guidelines for literature review. This step assessed each paper’s administrative information such as titles, authors, the introduction, the research method, study design, risks of biases and confidence in cumulative evidence. In terms of risk of bias assessment, the Application of Cochrane Collaboration’s tool for assessing risk of bias was used. Each study was evaluated for seven factors, including random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other potential sources of bias. Each factor was categorized as ‘‘low risk’’, ‘‘high risk’’ or “unclear risk” of bias.
Microsoft excel version 2016 was used for data extraction. Data extraction involved developing a standardized form to collect relevant information from the selected studies, including study characteristics, participant characteristics, details of the VR intervention, outcome measures, and results related to endoscopic skills acquisition or patient outcomes. The outcome measures included the effectiveness of VR tools in improving technical skills and performance, the feasibility and acceptability of VR-based training programs, the impact of VR training on patient outcomes, the advantages and limitations of VR-based training and other secondary outcomes.
To limit bias, the data collection process was also done under the supervision of the study supervisor.
A narrative synthesis of the included studies summarized their characteristics and findings. Heterogeneity among the studies was assessed by considering the study designs, participant characteristics, VR interventions, and outcome measures.
The Search command retrieved 673 references. After applying the exclusion criteria (duplicate records, n = 1; non-English records, n = 1; “review” records, n = 128; meeting abstract without full-text, n = 5; not meeting criteria, n = 522), 16 articles were included in the final analysis. Figure 1 explains the selection process. Table 1 and Table 2 summarizes the data gathered from each included paper.
| Ref. | Study design | Study setting | Duration | Types of trainees | No. of participants | Types of colonoscopies | Types of VR training |
| Buzink et al[4], 2007 | Pre and post study | Academic medical centers | Novice endoscopists, expert endoscopists | 30 | Colonoscopy | GI Mentor II | |
| Cohen et al[15], 2006 | Multicenter RCT | Academic medical centers | 2 yr | Gastroenterology fellows | 45 | Colonoscopy | GI Mentor |
| Ferlitsch et al[10], 2002 | Single-center RCT | Academic institution | 3 wk | Medical residents | 13 | Upper endoscopy and colonoscopy | GI Mentor |
| Ferlitsch et al[12], 2010 | Single-center RCT | Academic institution | 4 yr | Internal medicine residents | 28 | Upper endoscopy | GI Mentor |
| Gerson and Van Dam[19], 2003 | Single-center RCT | Academic institution | 9 months | Internal medicine residents | 16 | Sigmoidoscopy | VR sigmoidoscopy simulator |
| Gomez et al[20], 2015 | Single-center RCT | Academic institution | 1 month | Surgery residents | 27 | Colonoscopy | GI Mentor |
| Grover et al[8], 2015 | Single-center RCT | Academic medical centers | 6 wk | Surgery residents, medicine residents, gastroenterology fellows | 33 | Colonoscopy | VR endoscopy simulator |
| Hashimoto et al[9], 2018 | Two-phase study | Academic medical centers | 6 months | Endoscopists | 44 | Upper endoscopy and colonoscopy | GI Mentor |
| Koch et al[11], 2015 | Prospective study | Academic institution | Trainees | 18 | Colonoscopy | GI Mentor II | |
| McIntosh et al[21], 2014 | Single-center RCT | Academic institution | 1 month | Residents between year 2-4 | 18 | Colonoscopy | GI Mentor II |
| Park et al[22], 2007 | Single-center RCT | Academic medical centers | Surgery residents, internal medicine residents | 24 | Colonoscopy | Computer-based colonoscopy simulator | |
| Piskorz et al[16], 2020 | Pre and post study | Academic medical centers | 1st yr fellows of gastroenterology | 126 | Upper endoscopy and colonoscopy | GI Mentor | |
| Shirai et al[23], 2008 | Single-center RCT | Academic institution | 17 months | Residents | 20 | Upper endoscopy | GI Mentor II |
| Silva Mendes et al[24], 2021 | Prospective, multicenter study | Academic institution | 6 months | 1st yr gastroenterology residents | 23 | Upper endoscopy and colonoscopy | GI Mentor II |
| Telem et al[18], 2014 | Prospective study | Academic institution | 6 wk | Novice surgical interns, attending physicians | 12 | Colonoscopy | GI Mentor |
| Van Sickle et al[17], 2011 | Multicenter pre and posttest study | Academic institution | 8 wk | Postgraduate year 1-4 | 41 | Upper endoscopy and colonoscopy | GI Mentor II |
| Ref. | Training methods | Duration of training and frequency of training sessions | Self-evaluation methods | Evaluation by trainers | Comparator | Main outcomes measured |
| Buzink et al[4], 2007 | Basic skills training | 4 sessions, each session: One EndoBubble task and managed multiple VR colonoscopy cases (two in first session and three in subsequent sessions) | Objective metrics | Proecess skills, procedure time | ||
| Cohen et al[15], 2006 | Basic skills training | 10 h of unsupervised training on the GI Mentor or no simulator experience during the first 8 wk of fellowship | Expert evaluations | No intervention | Procedure completion, global rating of performance, patient discomfort | |
| Ferlitsch et al[10], 2002 | Basic skills training | 2 h per d, 3 wk | Objective metrics | No intervention | Proecess skills, procedure time | |
| Ferlitsch et al[12], 2010 | Basic skills training | 2 h per d, 5 h to 20 h in total | Expert evaluations | Conventional, patient-based training only | Precedure time, patient discomfort | |
| Gerson and Van Dam[19], 2003 | Basic skills training | 2 wk or ten sigmoidoscopy examination with attending gastroenterologists | Expert evaluations | Bedside teaching | Procedure time, procedure completion, patient discomfort, complication or critical flaw, global rating performance | |
| Gomez et al[20], 2015 | Basic skills training | 3 modules, 3 wk in total | Expert evaluations (GAGES scale) | Physical simulator group, combination group | Composite score of competency, performance time, visualization of mucosa | |
| Grover et al[8], 2015 | Basic skills training | 6 h of didactic lectures and 8 h of VR simulation-based training with expert feedback | Expert evaluations (JAG DOPS scale) | VR simulation training only (no experts feedback) | Composite score of competency | |
| Hashimoto et al[9], 2018 | Basic skills training | Not limited | Objective metrics | Ten repetitions of each VR simulator | Precedure skills | |
| Koch et al[11], 2015 | Basic skills training | 50 (group I) or 100 (group II) VR colonoscopies | Expert evaluations | 50 (group I) or 100 (group II) VR colonoscopies | Procedure time, procedure completion | |
| McIntosh et al[21], 2014 | Basic skills training | 16 h of VR simulator training | Expert evaluations, objective metrics | No intervention | The number of proctors 'assists' required per colonoscopy. Precedure time, precedure skills, patient discomfort | |
| Park et al[22], 2007 | Basic skills training | Expert evaluations (global rating scale) | No intervention | Procedure completion, complication or critical flaw | ||
| Piskorz et al[16], 2020 | Basic skills training | 8-h worked utilizing two GI Mentor™ in a specialized clinical simulation center | Objective metrics | Precedure time, precedure skills | ||
| Shirai et al[23], 2008 | Basic skills training | 5 h simulation training + bedside training vs bedside training | Expert evaluations | Conventional, patient-based training only | Precedure time | |
| Silva Mendes et al[24], 2021 | Basic skills training | Theoretical and a hands-on module (20 h) in the GI Mentor II | Objective metrics | Cognitive score, precudure time, precedure skills, patient discomfort | ||
| Telem et al[18], 2014 | Basic skills training | 2 h a wk, 6 wk | Expert evaluations (GAGES scale), objective metrics | No intervention | Precudure skills, precudure time | |
| Van Sickle et al[17], 2011 | Basic skills training, advanced skills | Self-rating score | Expert evaluations (GAGES scale), objective metrics | Precedure time, precedure skills, patient discomfort |
The studies were mainly from the United States (6 studies), followed by Canada and Netherlands (2 studies each), and Austria, United Kingdom, Argentina and Portugal (1 study each). The total number of participants was 523. The sample size ranged from 12 to 126 participants, with six studies having more than 30 participants[4,8,9,15-17]. The smallest sample sizes were from Ferlitsch et al[10], 2002, and Telem et al[18], 2014, with 12 and 13 participants, respectively[10,18]. All participants were physicians of different specialties, including endoscopists, expert endoscopists, gastroenterology fellows, and surgery or internal medicine residents.
Nine of the studies were randomized controlled trials[8,10,12,15,19-23], two were pre and post designs, and two were prospective studies[4,16,11,24]. The study by Hashimoto et al[9] in 2018 had two phases[9].
The academic setting was standard for all studies, with nine conducted at academic institutions and seven at academic medical centers. The duration of the studies varied from week to years, with the most extended being Ferlitsch et al[12] in 2010, which lasted for four years[12].
Regarding the types of endoscopy, five studies focused on both upper endoscopy and colonoscopy training, two on upper endoscopy training only, eight on colonoscopy training only, and one on sigmoidoscopy training only.
A variety of simulator systems were used for simulation-based training, such as the gastrointestinal (GI) Mentor virtual endoscopy simulator (13 studies), VR sigmoidoscopy simulator[19], VR endoscopy simulator (Grover, 2015)[8] and computer-based colonoscopy simulator[22]. The GI Mentor II was the most commonly used method. The VR platform was mainly used to train fundamental skills, except for one trial that included basic and advanced skills training[17].
The control group was exposed to different types of interventions across the studies. The control group received no intervention in five trials[10,15,18,21,22]. In two trials, the control group underwent conventional bedside teaching training, while the intervention group received VR training[12,19]. In the remaining trials, the control group also used a physical or VR simulator with less time or feedback than the intervention group.
The assessment methods varied across the studies. Three studies used expert ratings based on specific scales and VR platform scores to evaluate trainees[17,18,22]. Eight studies relied on expert ratings only, while five studies used only VR platform scores[4,9,10,16,24]. Van Sickle et al[17] study was the only one that also included self-rating as an assessment method[17]. Among studies that used experts' assessment, the Global Assessment of Gastrointestinal Endoscopic Skills (GAGES) scale was the most commonly used.
The measurement of primary outcomes varied among different studies, but the most common primary outcomes were procedure time, procedure skills, and patient discomfort.
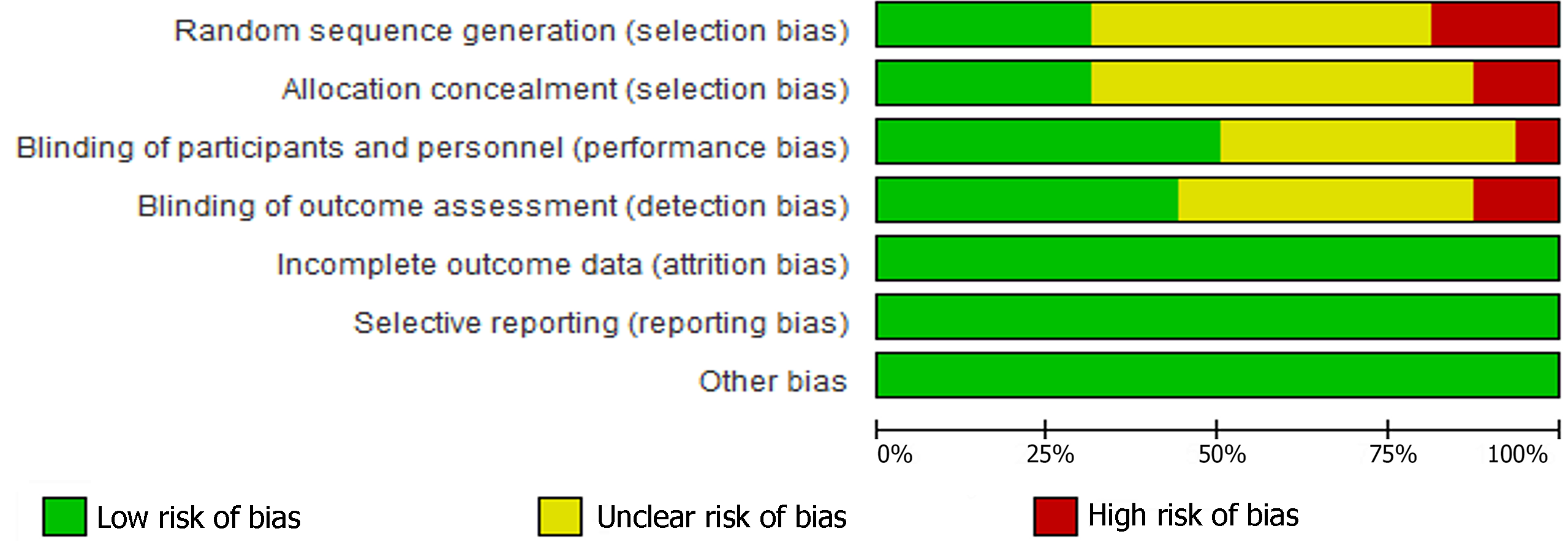
Figure 2 shows the risk of bias assessment for the included studies. Two studies had low risk of bias in all domains[3,10]. Five studies had high risk of bias in one or more domains, such as blinding[12,19] and selection[17,19-21]. Nine studies had unclear risk of bias in some domains, mainly due to insufficient reporting of randomization, allocation concealment, blinding of participants and/or blinding of outcome assessment. Figure 3 summarizes the risk of bias across the studies. Most studies had low attrition bias and reporting bias, while selection bias was the most common source of high or unclear risk of bias.
Yellow circles, green circles and red circles illustrate ‘‘unclear risk of bias,’’ ‘‘low risk of bias,’’ and ‘‘high risk of bias,’’ respectively.
The primary outcome in included studies was effectiveness of VR in different circumstances, without comparator, vs no training, vs conventional patient-based training, vs other forms of endoscopy simulation. Most of the studies indicated that that VR-based training was feasible and acceptable for endoscopy learners, including enhance their skills in manipulating the endoscope, reducing the procedure time or increasing the technical accuracy, in VR scenarios and real patients. Some studies assessed the impact of VR training in patient outcomes, advantages and limitations of VR-based training and the feasibility and acceptability of VR-based training program.
Four studies assessed the role of VR in endoscopy training. All of them used the GI mentor as the training tool, and most focused on colonoscopy, with basic endoscopy skills[4,16,17,24].
Buzink et al[4] conducted a study to examine the learning curve of novice endoscopists in basic endoscope navigation skills using the GI Mentor II simulator[4]. The study involved 30 participants who had no prior experience in endoscopy, and they completed a VR training session. The task for the VR colonoscopies was to reach the cecum as fast as possible without causing patient discomfort. The result showed that the novices improved significantly, especially in the time needed to complete the tasks. The study implies that VR colonoscopy training significantly enhances novice endoscopists' basic endoscope navigation skills. Piskorz et al[16], 2020, reported that trainees who used two GI Mentor™ for 8 h in a clinical simulation center improved their psychomotor skills and endoscopic skills (including cecal intubation time, percentage of examined mucosa, and efficacy of screening) significantly[16].
The quality of the endoscopic study also improved; the proportion of examined mucosa over 85% increased significantly after training with an adjusted OR of 2.72 (95%CI: 1.51-4.89, P = 0.001). The authors concluded that the addition of VR endoscopy in the training curriculum enhances trainee endoscopists' performance and psychomotor skills and teaches them how to conduct a quality endoscopic study in a safe and non-patient setting.
A prospective, multicenter study by Silva Mendes et al[24] in 2021 examined the effectiveness of GI Mentor II for teaching esophagogastroduodenoscopy (EGD) and colonoscopy. The study measured the technical skills of 21 residents based on the time to reach the D2/cecum (seconds), the efficiency of screening (%), and the time the patient was in pain (%). The residents received theoretical and practical training for 20 h using the GI Mentor II. The results showed that the residents improved their cognitive score and significantly reduced the time the patient was in pain (27% vs 10%, P = 0.005). The screening efficiency also increased, although not significantly (50% vs 68%, P = 0.062). The study concluded that VR could be useful for teaching cognitive and technical skills to novice endoscopists[24]. Likewise, the study of Van Sickle et al[17], 2011 proved the same patterns. His study used two GI Mentor II flexible endoscopy simulators, and postgraduate years from year 1 to year four participated in this study. This is a multicenter study, with five medical institutions, including the University of Texas Health Science Center-San Antonio, Texas A and M University, Methodist Hospital, and Brooke Army Medical Center, and University of Texas Southwestern. After the training, the procedure time, screening efficiency, and GAGES scores increased significantly. In addition, subjects' endoscopy self-rating scores also show an increase. In conclusion, residents who completed the VR training demonstrated subjective and objective growth in flexible endoscopy skills[17].
Five studies had the control group did not receive intervention, compared to the VR training group, which included 10 h for eight weeks[15], 2 h per day for three weeks[10], 16 h of VR[21], 2 to 3 h[22] or 2 h a week, six weeks[18] of unsupervised training on the GI Mentor I or II. It can be seen clearly that the VR training group in all five studies significantly improved their endoscopy competency after training.
The intervention group showed better objective and subjective outcomes than the control group in Cohen J's study[15]. The simulator group had higher objective competence, which means they could reach the transverse colon and the cecum without help and recognize and identify abnormalities correctly, with P < 0.0001. The difference was more pronounced in the first four blocks than in the last 16 blocks of 20 cases (P < 0.001). The simulator group also improved their subjective performance, which was rated on a 5-point scale from 1 (totally unskilled) to 5 (competent and expedient), with P < 0.001. The gap between the groups was more significant in the first 40 cases than in the remaining 160 cases (P = 0.02). In conclusion, trainees who underwent GI mentor training performed significantly better during the early phase of real colonoscopy training[15].
The study by Ferlitsch et al[10] in 2002 shows that intervention improved performance significantly after three weeks of VR training. This could be considered a fast improvement in endoscopic skills. The number of adverse events during endoscopy, the insertion time during colonoscopy, and skill test performance all showed significant improvement. One limit of this study was that the VR-based cases, which cannot interpret the impact of virtual simulator training on real-life endoscopy[10].
According to Ferlitsch et al[10] 2002 study, three weeks VR training significantly enhanced the intervention's effectiveness. This suggests a rapid improvement in endoscopic skills. The outcomes of skill test performance, insertion time during colonoscopy, and adverse events during endoscopy all improved considerably. However, this study had a limitation: The VR-based assessment did not reflect real-life endoscopy scenarios, so the influence of virtual simulator training on actual endoscopy needed to be clarified[10].
McIntosh et al[21] conducted a study to evaluate the effect of VR simulator training on novice trainees' performance of patient-based colonoscopies. They divided the participants into two groups: The intervention group received 16 h of VR training in GI Mentor II, while the control group did not. The results indicated that the intervention group performed better than the control group regarding procedure time, procedure skill, proctor assists, and competence ratings from the proctors and the nurses. The authors suggested that VR colonoscopy simulation is a valuable tool to enhance the learning curve of beginner colonoscopists, especially in the early training phase[21].
According to Park et al[22], 2007, residents who practiced colonoscopy on a simulator before their first live patient procedure performed significantly better than those who did not. The global ratings of performance, which were validated by previous studies, were higher for the treatment group than the control group. This demonstrated that VR skills can be transferred to live patients. However, only 2 out of 8 metrics from the computer-based simulator correlated significantly with the global ratings. This suggests that the simulator's metrics should be refined to match the actual performance level better[22].
Likewise, the Telem et al[18], 2014 study suggested that training on the GI mentor simulator improved the colonoscopic skills of novice surgical interns. Before training, only one intern (11%) could reach the cecum in 19.56 min. After training, six interns (67%) could do it in 9.2 min on average (P < 0.05). They also improved in four of the five GAGES-C criteria. The interns who reached the cecum after training had better scores on the simulator in efficiency (79% vs 67.1%, P = 0.05) and time to cecum (3.37 vs 5.59 min, P = 0.01) than those who did not. There was no significant difference in other GAGES-C categories or simulator parameters. Although the assessment was animal and VR-based, this study still supports training on the GI mentor simulator, improved the colonoscopic skills of novice surgical interns, and used this endoscopic simulator training as an effective supplement to clinical experience for surgical residents[18].
In conclusion, five studies show that VR training helped improve their endoscopy competency significantly, including procedure time, procedure skills, procedure completion, and global performance rating. They also support using endoscopic simulator training as a supplement to clinical experience for surgical residents.
Three single-center randomized controlled trials (RCTs) from Ferlitsch et al[10], 2010; Gerson and Van Dam[19], 2003; and Shirai et al[23], 2008 assessed the effectiveness of VR tools for training in gastrointestinal endoscopy, including upper and lower endoscopy. They compared the VR training group with conventional patient-based training. The outcomes were diverse, and there were some controversies[10,19,23].
The trial by Ferlitsch et al[10], 2010 demonstrates that VR training positively impacts technical accuracy, such as procedure time and diagnosis of pathological entities. The trial shows that the VR group reached the duodenum faster than the control group in their first ten endoscopic examinations in patients [239 s (range 50-620) vs 310 s (110-720)], with P < 0.0001, and performed better in technical accuracy with P < 0.02. After 60 endoscopic examinations, the VR group's investigation time was still shorter group. However, the VR group no longer had an advantage over the control group in terms of technical accuracy or diagnostic accuracy. In addition, simulator training did not increase the number of pathological entities detected. However, both groups improved their skills and knowledge significantly after 60 live patients' examinations and increased their rate of pathological findings during upper gastrointestinal endoscopy. Therefore, the trial indicates that VR training can be a beneficial component of an endoscopy training curriculum. However, it cannot wholly substitute on-patient training, which is essential for training success[10].
Likewise, Shirai et al[23] (2008) conducted a study to evaluate the impact of the GI-Mentor II simulator on residents' EGD skills. They randomly assigned the residents to two groups: One group received simulator training (5 h) and bedside training, while the other group received only bedside training. The residents then performed two EGDs each and were assessed on 11 criteria using a five-point scale. The simulator group showed significantly higher scores on the criteria related to insertion and navigation skills, such as esophageal entry, esophagogastric junction and pylorus crossing, and duodenal bulb and fornix examination. VR training helps residents with manipulation skills[19].
Conversely, an RCT by Gerson and Van Dam[19] in 2003 compared the effectiveness of VR and bedside teaching methods for teaching internal medicine residents how to perform sigmoidoscopy in asymptomatic patients for colorectal cancer screening. The trial involved 16 residents who did five procedures each, and their duration, completion, and skills were measured. The trial found that the VR group had more challenges inserting the endoscope and passing the rectosigmoid junction than the conventional group. VR group also had lower rates of reaching the splenic flexure independently and retroflexing the endoscope. Their average procedure time was longer as well. The trial concluded that a VR-based endoscopy simulator was less effective than conventional bedside teaching techniques when used solely for training residents in sigmoidoscopy[23].
Among 16 studies, one study from Gomez PP, 2015 assessed VR training compared to physical model training. Participants in this RCT completed a 3-wk flexible endoscopy curriculum. One group was assigned to train with the GI mentor simulator, one with the Kyoto physical simulator, and the last with both simulators. The trial indicates that there is a statistically significant improvement in the GAGES total score (P < 0.001). The VR group or combination group showed significant improvement from the pretest to the posttest in terms of GAGES total score (P = 0.017 vs 0.024, respectively). This was not observed for those exclusively using the Kyoto platform (P = 0.072. This trial suggests that VR training with the GI mentor platform for colonoscopy training, or in combination with a physical model simulator, improves skill performance in real colonoscopy cases when measured with the GAGES tool[20].
Hashimoto et al[9], 2018, Koch et al[11], 2015 and Grover et al[8], 2015 conducted studies that compared different methods of VR application in endoscopy training[8,9,11].
Hashimoto et al[9] used the fundamentals of endoscopic surgery (FES) examination, which measures knowledge and skill in flexible GI endoscopy. They randomly assigned participants in pairs to either a repetition curriculum (10 times each task) or a proficiency curriculum (repeated each task until reaching the benchmark twice in a row). They compared both groups' FES scores and pass rates with national and institutional data. The proficiency group outperformed the historical control group significantly (P = 0.0003) and had a 100% pass rate (proficiency: 100%, historical control 61.5%, P = 0.01). The repetition and proficiency curricula had similar results, but only the proficiency curriculum had a 100% pass rate and a performance that was significantly better than the historical institutional control[9].
Koch et al[11] conducted a study with two groups of participants. Group I had 50 VR colonoscopies, and group II had 100 cases. Participants were evaluated on both simulator-based assessment (SBA) and patient-based assessment, and the average cecal intubation time on the SBA for all participants reduced from 9.50 min at the beginning to 2.20 min at the end of the training (P = 0.002). Colonic insertion depth during patient-based assessment increased from 29.4 cm to 63.7 cm (P <0.001). The findings indicate a quick improvement in simulator performance during the first 50 VR colonoscopies. After 60 VR colonoscopies, the learning effect of extended training on the simulator diminished. This implies that VR training in colonoscopy can enhance performance on the simulator and, more importantly, patient-based colonoscopy. This study also supports intensive simulator training in the early learning curve of colonoscopy trainees[11].
A RCT by Grover et al[8] in 2015 evaluated the effectiveness of a simulation-based structured comprehensive curriculum (SCC) for colonoscopy training. The SCC group received six hours of theoretical lectures and eight hours of VR training with expert feedback, while the control group only received a list of objectives and practiced on the same simulator for eight hours without feedback. The outcome measures showed that the SCC group had better performance, knowledge, communication, and global skills during their first and second clinical colonoscopies than the control group[8].
The potential of VR training in endoscopy was demonstrated by all three studies, which enhanced the skills of trainees in both VR cases and live patients. However, the first two studies differed in their recommendations regarding the timing and duration of VR training. The authors suggested a more extensive, multi-center study to address this limitation. The trial of Grover et al[8] showed the importance of incorporating endoscopy simulation into a structured curriculum that includes VR training, instructional feedback, and complementary didactic knowledge as the most effective way to train in colonoscopy.
Many of the 16 studies that were reviewed focused on evaluating the patient outcomes of VR training for endoscopy. In addition to improving endoscopy capacities in live patients from VR training, such as procedure time, procedure skills, some studies also assessed the level of discomfort the patients experienced during the procedure. One such study, conducted by Van Sickle et al[17] in 2011, demonstrated that after the VR training, flexible endoscopies of trainees showed that the patient discomfort level decreased significantly, indicating a positive impact on patient satisfaction and safety[17]. However, not all studies found such benefits of VR training on patient outcomes. In the group of studies that compared VR training with no training, the patient's perspectives were also evaluated by Cohen et al[15] in 2006 and McIntosh et al[21] in 2014. The results of Cohen et al[15] study showed that the simulator and the control groups performed similarly overall, and there was no significant difference in the patient comfort level between them[15]. Likewise, McIntosh et al[21]2002 reported no significant differences in pain ratings by proctors, nurses, or patients or attention to discomfort between the VR group and the no-training group[21]. Similarly, according to the studies from Ferlitsch et al[12] in 2010 and Gerson and Van Dam[19] in 2003, which compared VR training with conventional patient-based training, there were no significant differences in patient discomfort and pain scores between the two groups. These findings suggest that VR training may not have a consistent or substantial effect on patient outcomes and that other factors may influence the patient experience of endoscopy[12,19].
VR training has some pros and cons compared to traditional training methods. This is shown by three studies from Ferlitsch et al[12], 2010; Gerson and Van Dam[19], 2003; and Shirai et al[23], 2008, that compare VR tools and bedside teaching for training in gastrointestinal endoscopy[12,19,23].
The study of Shirai et al[23] in 2008 proved other advantages of VR tools. According to this study, the VR simulator helped trainees significantly improve manipulation skills, including insertion and navigation skills, such as esophageal entry, EGJ and pylorus crossing, and duodenal bulb and fornix examination[12].
However, according to the study by Ferlitsch et al[10], 2010, the VR group had better procedure time and technical accuracy results than the conventional group. However, this advantage did not last long, and the VR group did not perform better than the control group in technical or diagnostic accuracy after a while. Moreover, the VR group did not detect more pathological entities than the control group. Therefore, this study suggests that VR is beneficial for training technical skills in the early stages of training. However, it has some drawbacks for training the later stages and the pathological entities. These are the areas where bedside teaching is more effective[19].
Similarly, regarding sigmoidoscopy in asymptomatic patients for colorectal cancer screening, the study from Gerson and Van Dam[19] in 2003 found that the VR group had more challenges with inserting the endoscope and passing the rectosigmoid junction than the conventional group. VR group also had lower rates of reaching the splenic flexure independently and retroflexing the endoscope. Their average procedure time was longer as well. The trial concluded that a VR-based endoscopy simulator was less effective than conventional bedside teaching techniques when used solely for training residents in sigmoidoscopy[23].
Gerson and Van Dam[19] (2003) concluded that a VR-based endoscopy simulator was inferior to conventional bedside teaching techniques when used alone for training residents in sigmoidoscopy. Notably, comparing the VR group and the conventional group in sigmoidoscopy for colorectal cancer screening, the VR group had more difficulties inserting the endoscope and passing the rectosigmoid junction than the conventional group. The VR group also had lower success rates of reaching the splenic flexure and retroflexing the endoscope. Their procedure time was longer as well[23].
This systematic review included 16 studies that assessed the feasibility and acceptability of using VR as a training tool for gastrointestinal endoscopy. Of these 16 studies, 15 reported positive results, indicating that VR-based training was feasible and acceptable for endoscopy learners. The main reason for this finding was that VR technology helped the trainees enhance their skills in manipulating the endoscope, reducing the procedure time or increasing the technical accuracy both in VR scenarios and in actual patients[4,15-17,24]. VR training was also a promising alternative to no training methods, as it improved the performance of endoscopy learners compared to those who did not receive any training. Furthermore, VR tools were superior to conventional training methods in some aspects, especially for the initial phases of endoscopy training, such as insertion and navigation skills[10,23]. Shirai et al[23] also suggested that VR could be used as an effective assessment tool with capabilities similar to expert evaluators[23].
Only one study out of 16 claimed that VR-based training was inferior to conventional teaching and could not replace it (Gerson and Van Dam[19], 2003). This study implied that VR technology did not offer the same benefits as traditional bedside teaching. However, it needed to consider combining the advantages of both teaching methods. A hybrid teaching method involving both VR and patient-based teaching could be a more effective way of delivering endoscopy training[19].
This systematic review underscores the efficacy of VR simulator training in instructing gastrointestinal endoscopy, encompassing both gastroscopy and colonoscopy. The findings reveal that VR training surpasses scenarios with no training, lacks comparators, or employs alternative simulations in enhancing trainees' proficiency in endoscope manipulation, procedure duration, psychomotor skills, and technical precision. Consequently, the incorporation of VR-based endoscopy training emerges as an innovative and beneficial approach for practical implementation. Moreover, the review suggests diverse strategies for training endoscopy learners, ranging from utilizing VR cases in isolation to combining them with lectures or incorporating expert feedback.
This systematic review indicates that VR training has some unique benefits, but it also has some drawbacks that prevent it from entirely replacing bedside teaching. Three single-center RCTs from Ferlitsch et al[12], 2010; Gerson and Van Dam[19], 2003; and Shirai et al[23], 2008 found that VR training can enhance an endoscopy training curriculum, but cannot substitute for on-patient training, which is crucial for success[12,19,23].
This systematic review of VR training's effects on patient discomfort levels reveals that VR training significantly reduced patient discomfort levels, suggesting a positive influence on patient satisfaction and safety. Although the VR and bedside teaching groups had similar overall performance, the VR training improved patient discomfort levels.
These findings are consistent with Singh et al[25] in 2014, Qiao et al[26] in 2014, Ekkelenkamp et al[27] in 2015, and Khan et al[28] in 2018.
A systematic review and meta-analysis by Singh et al[25] 2014 examined 39 articles on simulation-based training for endoscopy. The result shows that compared with no intervention (n = 32 studies), simulation-based training significantly improved endoscopic process skills in a test setting [effect size (ES) = 0.79, n = 22], process behaviors in clinical practice (ES = 0.49, n = 8), time to procedure completion in both a test setting (ES = 0.79, n = 16) and clinical practice (ES = 0.75, n = 5), and patient outcomes (procedural completion and risk of significant complications, ES = 0.45, n = 10). Only five studies evaluated the comparative effectiveness of different simulation-based training approaches, which provided inconclusive evidence regarding feedback and simulation modalities[25].
According to a systematic review by Qiao et al[26] in 2014, fifteen studies met the inclusion criteria of his study. The review compared the outcomes of simulators and conventional training for gastroscopy and colonoscopy. For gastroscopy, simulator training resulted in a significantly higher rate of independent completion of the procedure (87.7% vs 70.0%, 1 study, 22 participants, relative risk (RR) = 1.25, 95%CI: 1.13–1.39, P < 0.0001). For colonoscopy, there was no significant difference between simulator training and conventional training in terms of independent completion of the procedure (89.3% vs 88.9%, 7 studies, 163 participants, RR = 1.10, 95%CI: 0.88–1.37, P = 0.41, I2 = 85%)[26].
Ekkelenkamp et al[27] 2015 carried out a systematic review of twenty-seven studies on simulator validation. Increased performance on a VR simulator was shown in all studies. Improved performance in patient-based assessment was demonstrated in 14 studies. Four studies reported on the use of simulators for assessment of competence levels. Current simulators lack the discriminative power to determine competence levels in patient-based endoscopy. Eight out of 14 studies on colonoscopy, endoscopic retrograde cholangiopancreatography, and endosonography reported on learning curves in patient-based endoscopy and proved the value of this approach for measuring performance. Ten studies explored the numbers needed for competence, but the proposed thresholds varied widely. Five out of nine studies describing the development and evaluation of assessment tools for GI endoscopy provided insight into the performance of endoscopists. Five out of seven studies proved that intense training programs result in good performance[27].
A 2018 review by Khan et al[28] analyzed 18 trials with 3817 endoscopic procedures performed in 2017. The review showed that VR training was better than no training in terms of independent procedure completion (RR = 1.62, 95%CI: 1.15–2.26, moderate-quality evidence), overall rating of performance [mean difference (MD) 0.45, 95%CI: 0.15–0.75, very low-quality evidence], and mucosal visualization (MD 0.60, 95%CI: 0.20–1.00, very low-quality evidence). On the other hand, VR training led to fewer independent procedure completions than conventional training (RR = 0.45, 95%CI: 0.27–0.74, low-quality evidence), and VR training did not improve the composite score of competencies compared to no training or conventional training. Khan et al[28] did not find any significant differences between VR training and no training or conventional training for other outcomes and did not find any significant differences between VR training and other simulation training methods based on qualitative analysis. Unlike unstructured curricula, VR curricula that were structured according to educational theory had a positive effect on the composite score of competencies[28].
This systematic review and the above all agreed that VR simulator training is practical for beginners in endoscopy training. Despite minor differences between this review and the other three, the results all suggest that VR-based teaching is effective in endoscopy training, especially in the early training phases. Although there are some debates about whether VR training can fully replace conventional training, it is still a balanced option to consider this method complementary to conventional endoscopy training.
The integration of VR training encounters notable challenges, with a primary obstacle being the substantial cost associated with VR technology for endoscopic training. Acquiring, maintaining, and updating VR simulators demands considerable financial investment, alongside the necessity for dedicated space and personnel. Consequently, the accessibility and affordability of VR training become limiting factors for numerous endoscopic centers, particularly those situated in low-resource settings. Furthermore, the scarcity of long-term studies assessing the impact of VR on clinical outcomes and patient safety raises additional concerns regarding the widespread feasibility of VR training, particularly in resource-constrained environments. Additionally, the development of cases tailored to meet learners' needs and curriculum objectives is a demanding task, requiring in-depth knowledge of the subject matter, learning outcomes, and effective pedagogical strategies.
Moreover, it involves carefully selecting relevant and authentic scenarios, data, and resources to engage and challenge the learners. Furthermore, it necessitates precisely aligning the case with the assessment criteria and feedback mechanisms. Therefore, case development is a complex and time-consuming process that requires careful planning, design, and evaluation. More long-term studies are needed to confirm the cost-effective balance and efficacy of simulator-based training methods for endoscopy learners.
Lately, the field of medicine is undergoing significant changes as a result of the development and application of artificial intelligence (AI) techniques[29,30]. Moreover, AI can also help improve the performance of endoscopists as a cutting-edge training tool[31]. By offering real-time assistance, feedback and evaluation, AI can facilitate the learning process of endoscopy and help endoscopists achieve better outcomes[32].
Endoscopy training can benefit from the integration of AI and VR. While AI can enhance the learning process by providing individualized feedback, tailoring the difficulty level to the learner's needs and generating realistic cases from real-world data, VR can augment and optimize the learning environment that mimic real environments. By combining AI and VR, endoscopy training can offer a more comprehensive and engaging learning experience that improves the trainees' competencies and self-efficacy. Blended learning, which combines conventional methods with cutting-edge technologies such as AI and VR, is a promising approach for endoscopy training. Another potential strategy is mobile health, which involves the use of mobile devices and wireless technologies to deliver health care services and education. Mobile health can enhance the accessibility, quality and efficiency of endoscopy training, especially in remote and rural areas. This strategy can complement blended learning. More studies are needed before implementing these methods to reality.
Regarding limitations, there was the diversity of results, including methodology, types of trainees, interventions and outcomes measured. As a result, head-to-head comparison of individual studies as well as meta-analysis were not conducted.
Additionally, our results were limited by methodological quality of the included studies. About half of them were non-randomized, including several single-group, pre and post, prospective and two-phase studies.
In conclusion, this systematic review supports the idea that VR training is practical for endoscopy training. There are several well-designed RCTs with large sample sizes, proving the potential of this innovative tool. Thus, VR should be more widely used in endoscopy training. Moreover, VR training in combination with conventional methods could be a promising approach that should be deployed in training. However, more studies are needed to compare VR training with traditional methods and to design the ideal curriculum for VR or VR and traditional methods.
We would like to extend our sincere appreciation to the Acute Medicine MSc program at the University of South Wales for their invaluable assistance in our work. We acknowledge and commend the University of South Wales for their commitment to providing advanced problem-solving skills and life-long learning opportunities for healthcare professionals.
| 1. | Lateef F. Simulation-based learning: Just like the real thing. J Emerg Trauma Shock. 2010;4:348-352. [RCA] [DOI] [Full Text] [Cited by in Crossref: 351] [Cited by in RCA: 366] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 2. | Mishra R, Narayanan MDK, Umana GE, Montemurro N, Chaurasia B, Deora H. Virtual Reality in Neurosurgery: Beyond Neurosurgical Planning. Int J Environ Res Public Health. 2022;19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 125] [Cited by in RCA: 112] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 3. | Dyer E, Swartzlander BJ, Gugliucci MR. Using virtual reality in medical education to teach empathy. J Med Libr Assoc. 2018;106:498-500. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 117] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 4. | Buzink SN, Koch AD, Heemskerk J, Botden SM, Goossens RH, de Ridder H, Schoon EJ, Jakimowicz JJ. Acquiring basic endoscopy skills by training on the GI Mentor II. Surg Endosc. 2007;21:1996-2003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Triantafyllou K, Lazaridis LD, Dimitriadis GD. Virtual reality simulators for gastrointestinal endoscopy training. World J Gastrointest Endosc. 2014;6:6-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 46] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Walsh CM, Sherlock ME, Ling SC, Carnahan H. Virtual reality simulation training for health professions trainees in gastrointestinal endoscopy. Cochrane Database Syst Rev. 2012;CD008237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 58] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 7. | Khan R, Plahouras J, Johnston BC, Scaffidi MA, Grover SC, Walsh CM. Virtual reality simulation training for health professions trainees in gastrointestinal endoscopy. Cochrane Database Syst Rev. 2018;8:CD008237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 59] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 8. | Grover SC, Garg A, Scaffidi MA, Yu JJ, Plener IS, Yong E, Cino M, Grantcharov TP, Walsh CM. Impact of a simulation training curriculum on technical and nontechnical skills in colonoscopy: a randomized trial. Gastrointest Endosc. 2015;82:1072-1079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 78] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 9. | Hashimoto DA, Petrusa E, Phitayakorn R, Valle C, Casey B, Gee D. A proficiency-based virtual reality endoscopy curriculum improves performance on the fundamentals of endoscopic surgery examination. Surg Endosc. 2018;32:1397-1404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Ferlitsch A, Glauninger P, Gupper A, Schillinger M, Haefner M, Gangl A, Schoefl R. Evaluation of a virtual endoscopy simulator for training in gastrointestinal endoscopy. Endoscopy. 2002;34:698-702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 107] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 11. | Koch AD, Ekkelenkamp VE, Haringsma J, Schoon EJ, de Man RA, Kuipers EJ. Simulated colonoscopy training leads to improved performance during patient-based assessment. Gastrointest Endosc. 2015;81:630-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Ferlitsch A, Schoefl R, Puespoek A, Miehsler W, Schoeniger-Hekele M, Hofer H, Gangl A, Homoncik M. Effect of virtual endoscopy simulator training on performance of upper gastrointestinal endoscopy in patients: a randomized controlled trial. Endoscopy. 2010;42:1049-1056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 60] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 13. | Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Gastroenterology (Internal Medicine). Available from: https://www.acgme.org/globalassets/pfassets/programrequirements/144_gastroenterology_2022_tcc.pdf. |
| 14. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44932] [Cited by in RCA: 51140] [Article Influence: 10228.0] [Reference Citation Analysis (2)] |
| 15. | Cohen J, Cohen SA, Vora KC, Xue X, Burdick JS, Bank S, Bini EJ, Bodenheimer H, Cerulli M, Gerdes H, Greenwald D, Gress F, Grosman I, Hawes R, Mullin G, Schnoll-Sussman F, Starpoli A, Stevens P, Tenner S, Villanueva G. Multicenter, randomized, controlled trial of virtual-reality simulator training in acquisition of competency in colonoscopy. Gastrointest Endosc. 2006;64:361-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 159] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 16. | Piskorz MM, Wonaga A, Bortot L, Linares ME, Araya V, Olmos JI, Gardey M, Perretta C, Olmos JA. Impact of a Virtual Endoscopy Training Curriculum in Novice Endoscopists: First Experience in Argentina. Dig Dis Sci. 2020;65:3072-3078. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Van Sickle KR, Buck L, Willis R, Mangram A, Truitt MS, Shabahang M, Thomas S, Trombetta L, Dunkin B, Scott D. A multicenter, simulation-based skills training collaborative using shared GI Mentor II systems: results from the Texas Association of Surgical Skills Laboratories (TASSL) flexible endoscopy curriculum. Surg Endosc. 2011;25:2980-2986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 18. | Telem DA, Rattner DW, Gee DW. Endoscopic simulator curriculum improves colonoscopy performance in novice surgical interns as demonstrated in a swine model. Surg Endosc. 2014;28:1494-1499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Gerson LB, Van Dam J. A prospective randomized trial comparing a virtual reality simulator to bedside teaching for training in sigmoidoscopy. Endoscopy. 2003;35:569-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 81] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 20. | Gomez PP, Willis RE, Van Sickle K. Evaluation of two flexible colonoscopy simulators and transfer of skills into clinical practice. J Surg Educ. 2015;72:220-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 21. | McIntosh KS, Gregor JC, Khanna NV. Computer-based virtual reality colonoscopy simulation improves patient-based colonoscopy performance. Can J Gastroenterol Hepatol. 2014;28:203-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Park J, MacRae H, Musselman LJ, Rossos P, Hamstra SJ, Wolman S, Reznick RK. Randomized controlled trial of virtual reality simulator training: transfer to live patients. Am J Surg. 2007;194:205-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 140] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 23. | Shirai Y, Yoshida T, Shiraishi R, Okamoto T, Nakamura H, Harada T, Nishikawa J, Sakaida I. Prospective randomized study on the use of a computer-based endoscopic simulator for training in esophagogastroduodenoscopy. J Gastroenterol Hepatol. 2008;23:1046-1050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Silva Mendes S, Areia M, Dinis Ribeiro M, Rolanda C. The Impact of a Structured Virtual Reality Simulation Training Curriculum for Novice Endoscopists. GE Port J Gastroenterol. 2022;29:385-392. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 25. | Singh S, Sedlack RE, Cook DA. Effects of simulation-based training in gastrointestinal endoscopy: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2014;12:1611-23.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 63] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 26. | Qiao W, Bai Y, Lv R, Zhang W, Chen Y, Lei S, Zhi F. The effect of virtual endoscopy simulator training on novices: a systematic review. PLoS One. 2014;9:e89224. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 27. | Ekkelenkamp VE, Koch AD, de Man RA, Kuipers EJ. Training and competence assessment in GI endoscopy: a systematic review. Gut. 2016;65:607-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 126] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 28. | Khan R, Plahouras J, Johnston BC, Scaffidi MA, Grover SC, Walsh CM. Virtual reality simulation training in endoscopy: a Cochrane review and meta-analysis. Endoscopy. 2019;51:653-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 72] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 29. | Tontini GE, Rimondi A, Vernero M, Neumann H, Vecchi M, Bezzio C, Cavallaro F. Artificial intelligence in gastrointestinal endoscopy for inflammatory bowel disease: a systematic review and new horizons. Therap Adv Gastroenterol. 2021;14:17562848211017730. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 30. | Soldera J. Artificial intelligence as a prognostic tool for gastrointestinal tract pathologies. Med Vozandes. 2023;34:9-14 Available from: https://revistamedicavozandes.com/wp-content/uploads/2023/07/02_EDITORIAL-1.html. |
| 31. | Sinonquel P, Eelbode T, Bossuyt P, Maes F, Bisschops R. Artificial intelligence and its impact on quality improvement in upper and lower gastrointestinal endoscopy. Dig Endosc. 2021;33:242-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 32. | El Hajjar A, Rey JF. Artificial intelligence in gastrointestinal endoscopy: general overview. Chin Med J (Engl). 2020;133:326-334. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 73] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country of origin: United Kingdom
Peer-review report’s classification
Scientific Quality: Grade A
Novelty: Grade A
Creativity or Innovation: Grade A
Scientific Significance: Grade A
P-Reviewer: Ammarullah MI, Indonesia S-Editor: Liu H L-Editor: A P-Editor: Cai YX