Published online Jun 8, 2025. doi: 10.35712/aig.v6.i1.106746
Revised: April 1, 2025
Accepted: April 11, 2025
Published online: June 8, 2025
Processing time: 92 Days and 18.2 Hours
Hepatobiliary surgery is complex and requires a thorough understanding of the liver’s anatomy, biliary system, and vasculature. Traditional imaging methods such as computed tomography (CT) and magnetic resonance imaging (MRI), although helpful, fail to provide three-dimensional (3D) relationships of these structures, which are critical for planning and executing complicated surgeries.
To explore the use of 3D imaging and virtual surgical planning (VSP) technologies to improve surgical accuracy, reduce complications, and enhance patient recovery in hepatobiliary surgeries.
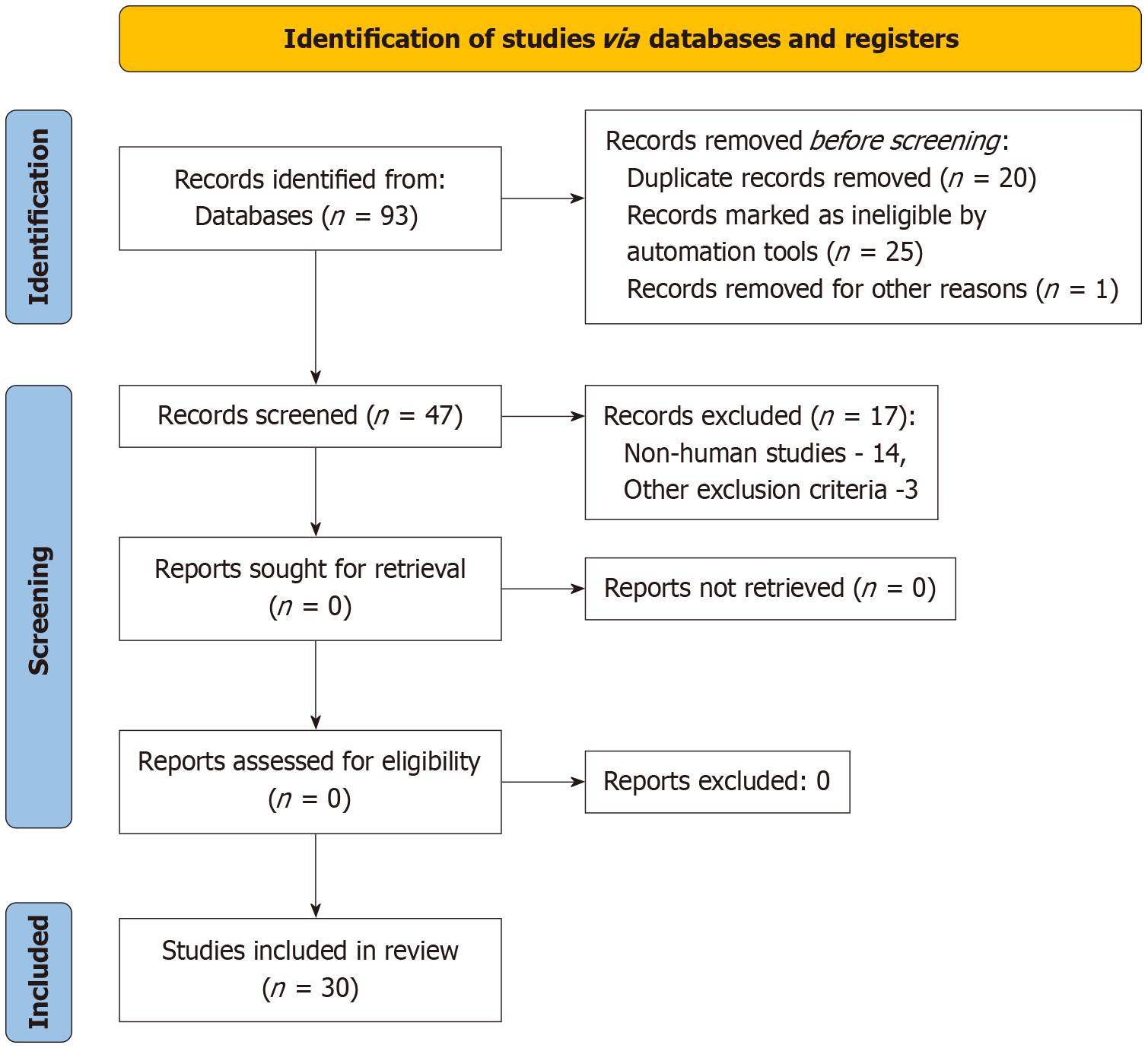
A comprehensive review of studies published between 2017 and 2024 was conducted through PubMed, Scopus, Google Scholar, and Web of Science. Studies selected focused on 3D imaging and VSP applications in hepatobiliary surgery, assessing surgical precision, complications, and patient outcomes. Thirty studies, including randomized controlled trials, cohort studies, and case reports, were included in the final analysis.
Various 3D imaging modalities, including multidetector CT, MRI, and 3D rotational angiography, provide high-resolution views of the liver’s vascular and biliary anatomy. VSP allows surgeons to simulate complex surgeries, improving preoperative planning and reducing complications like bleeding and bile leaks. Several studies have demonstrated improved surgical precision, reduced complications, and faster recovery times when 3D imaging and VSP were used in complex surgeries.
3D imaging and VSP technologies significantly enhance the accuracy and outcomes of hepatobiliary surgeries by providing individualized preoperative planning. While promising, further research, particularly randomized controlled trials, is needed to standardize protocols and evaluate long-term efficacy.
Core Tip: Integration of three dimensional (3D) imaging and virtual surgical planning has led to enhanced surgical precision, providing detailed anatomical visualization that significantly improves surgical accuracy. This allows for better preoperative planning and reduces intraoperative complications. The use of 3D models has contributed to a reduction in complications, with decreased operative times, lower blood loss, and fewer postoperative issues such as bile leaks and vascular injuries, thereby improving patient safety. Surgeries that incorporate 3D-assisted planning also result in improved patient outcomes, including faster recovery, lower morbidity rates, and better long-term survival, particularly in complex procedures like liver transplantation and hepatectomies.
- Citation: Agrawal H, Tanwar H, Gupta N. Revolutionizing hepatobiliary surgery: Impact of three-dimensional imaging and virtual surgical planning on precision, complications, and patient outcomes. Artif Intell Gastroenterol 2025; 6(1): 106746
- URL: https://www.wjgnet.com/2644-3236/full/v6/i1/106746.htm
- DOI: https://dx.doi.org/10.35712/aig.v6.i1.106746
Hepatobiliary surgery is one of the most challenging and complex surgical specialties. It requires surgeons to have a high level of expertise in the anatomy of the liver, biliary tree and their vasculature. The liver has a dual blood supply from the hepatic artery and the portal vein, and the biliary system presents special challenges because of its complex and highly individual anatomy. Special techniques like living donor liver transplantation (LDLT), extended hepatectomies, and complex bile duct resections are technically demanding and require excellent preoperative planning and execution of the operations to prevent hemorrhage, bile leakage, and liver failure while attempting to maximize patient benefits[1]. Computed tomography (CT) and magnetic resonance imaging (MRI) have traditionally been used to obtain two-dimensional (2D) images in preoperative assessment in hepatobiliary surgery. These imaging techniques are useful in determining the size, site, and vascular involvement of tumors. However, they are inadequate to demonstrate the real 3D relationships of the tumors with the hepatic veins and arteries, portal pedicles and bile ducts. This may pose a problem during the intraoperative period, resulting in increased operative time, intraoperative blood loss, and an increased risk of injuring vital structures[2]. The availability of improved 3D imaging technologies and virtual surgical planning (VSP) has revolutionized hepatobiliary surgery. These tools help surgeons generate very accurate patient-specified 3D models of the liver and its associated structures, thus giving the surgeon a better and easy understanding of the surgical anatomy. 3D models are generated by combining CT or MRI and other imaging techniques to offer a realistic view of the tumor, its relationship with the nearby vasculature, and biliary ducts. This helps the surgeon to plan complicated operations with more certainty[3]. In living donor liver transplant, 3D imaging can determine the size and vascular anatomy of the donor liver which in turn reduces the risk to the donor and the recipient. For instance, in hilar cholangiocarcinoma and other biliary duct tumors such as complex neuroendocrine tumors, the 3D models can be used to determine the extent of resection of the bile duct and the type of biliary enteric anastomosis to be done[4]. Also, VSP can help to perform simulation of surgeries that can help the surgeons to identify the possible issues and modify their strategy even before making an entry to the operating room. This not only improves the surgical efficacy, but also prevents certain life threatening complications[5]. 3D imaging and VSP are becoming popular in hepatobiliary surgery, but their effects on precision, complications, and patient results are not fully understood. However, to the best of our knowledge, no previous study has attempted to consolidate the available evidence on the effects of these technologies on surgical practice.
Hence, the purpose of this mini review was to assess the literature that exists on the use of 3D imaging and VSP in hepatobiliary surgery with regard to the accuracy of surgery, complications, and patients’ recovery.
This mini review examined studies focused on the application of 3D imaging and VSP in hepatobiliary surgeries. The studies included in this review either utilized 3D imaging or VSP as part of the surgical process or reported on surgical precision, complication rates, or patient outcomes such as morbidity, mortality, or recovery time, and were clinical trials, cohort studies, or case studies published in peer-reviewed journals. Exclusion criteria eliminated studies not directly related to hepatobiliary surgery, those that did not focus on 3D imaging or VSP technologies, and case reports or studies involving fewer than 10 participants.
Data for this review were sourced from multiple electronic databases, including PubMed, Scopus, Google Scholar and Web of Science. A comprehensive search was conducted using keywords such as "3D imaging", "virtual surgical planning", "hepatobiliary surgery", "liver resection", "liver transplantation", "biliary surgery", and "surgical precision". The search was restricted to studies published in English between 2017 and 2024 to ensure that the latest advancements were considered (Figure 1).
The study selection process involved two reviewers who screened the titles and abstracts of studies to assess eligibility. Full-text articles of potentially relevant studies were then reviewed to confirm whether they met the inclusion criteria. Disagreements between reviewers were resolved through discussion, and a third reviewer was consulted in cases of uncertainty.
Key data extracted from the included studies included study design and methodology, patient characteristics (age, sex, type of surgery), technology used (specific types of 3D imaging, software, and VSP tools), primary outcomes measured (surgical precision, complications, patient outcomes), and key findings and conclusions. Data analysis involved a qualitative synthesis, categorizing the findings into three main areas: Surgical precision, complications, and patient outcomes. Studies were summarized based on how 3D imaging and VSP impacted these outcomes, and the quality of the studies was assessed using standard critical appraisal tools.
A total of 30 studies were included in this mini review. The studies included randomized controlled trials, cohort studies, and systematic reviews focused on the use of 3D imaging and VSP in hepatobiliary surgery. The majority of the studies (22) evaluated the use of 3D imaging in hepatobiliary surgery, while the remaining studies (8) focused on VSP or the combined use of both technologies. These studies involved a wide range of patient demographics, with both adult and pediatric populations included.
Several 3D imaging modalities are used in hepatobiliary surgery, each having their own advantages and limitations. Multidetector CT (MDCT) is the most frequent technique employed for the construction of 3D representations because of its high spatial resolution and short acquisition time[6]. This enables precise demonstration of the vascular anatomy including the portal vein, hepatic veins and hepatic arteries. Contrast-enhanced MDCT also gives important data on tumor nature and vascular invasion, which are important in surgery. The opposite is true for MRI, which offers better soft tissue contrast and is particularly useful in evaluating the liver parenchyma in hepatocellular carcinoma. Magnetic resonance cholangiopancreatography is an MRI sequence that gives a clear view of the biliary tree and is therefore used to plan bile duct resections[7]. 3D rotational angiography gives a high-resolution view of the vasculature, which is particularly helpful in the assessment of hepatic arterial variations, a critical determinant in LDLT and complex hepatectomies. Finally, imaging fusion, which is the combination of data from different modalities such as MDCT and MRI, gives a better understanding of the anatomy by incorporating the best features of each modality[8].
In hepatobiliary surgeries, the shift from traditional surgical planning techniques to advanced technologies such as 3D imaging and VSP has significantly enhanced surgical precision, patient outcomes, and safety. Traditional methods predominantly depend on 2D imaging techniques like ultrasound, X-rays, and CT scans, which offer limited views of the liver, bile ducts, and surrounding structures. Surgeons interpret complex anatomical relationships from these flat images, often relying on their experience to deduce optimal surgical approaches, which may lead to less favorable outcomes, especially in complex cases. Manual surgical planning, which involves marking key anatomical landmarks and predicting potential risks, is also dependent on the surgeon’s expertise and the quality of available imaging, which may vary across institutions and settings.
By contrast, 3D imaging and VSP offer more dynamic, interactive, and accurate ways to plan surgeries. Using advanced CT or MRI scans, 3D imaging creates volumetric models that provide a clearer view of the liver, bile ducts, and blood vessels, improving the surgeon’s understanding of spatial relationships between organs. This technology is especially valuable in complex surgeries, such as liver resections or bile duct reconstructions, where a precise understanding of anatomy is critical. VSP further enhances this by allowing surgeons to simulate different surgical approaches in a virtual environment, helping to anticipate challenges like vascular anomalies and difficult access points. This preoperative tool enables more personalized and precise surgical strategies, which can reduce operative time and complications.
The primary advantage of 3D imaging and VSP over traditional methods lies in their ability to offer comprehensive, 3D visualizations of intricate anatomical structures, facilitating better preoperative assessments and more accurate planning. For instance, 3D imaging allows surgeons to map out tumor locations, blood vessels, bile ducts, and other crucial structures, thereby minimizing surgical risks. VSP also offers the benefit of rehearsing various surgical approaches in a virtual setting, reducing the chances of unforeseen challenges during the actual procedure. This is particularly beneficial in complex cases, such as liver transplants and resections, where meticulous planning is essential for success.
VSP is a multistep process, starting with image acquisition, which is usually from MDCT, to obtain high-quality 3D data. Using specialized software, 3D reconstructed models of the liver, biliary tree, and associated vasculature are created from the 2D image data. For individual anatomical structures, segmentation is done to allow for independent manipulation and visualization. These 3D models demonstrate various surgical approaches, determine resectability and define the best resection margins. It can include simulations of virtual liver resection, vascular clamping, and remaining liver volume. Sometimes, 3D-printed models (3DPMs) of the liver can be created, to provide a physical copy of the anatomy for preoperative planning, and intraoperative guidance[9].
Yao et al[2] stated that 3D planning in dry-laboratory conditions can decrease the rate of perioperative complications in laparoscopic surgery for complex hepatobiliary diseases. Their study included 100 patients who underwent laparoscopic hepatectomy and the control group received standard preoperative planning. The study revealed that the use of 3DPMs for planning led to a decrease in the operative time, blood loss, and postoperative complications in the experimental group.
Park et al[10] reported that 3D printing of the intra-abdominal cavity reduced the risk of large for size syndrome and improved graft survival in liver transplantation. Their research involved 50 liver transplant recipients and they concluded that the use of 3DPMs models in preoperative planning increased the one-year graft survival rates by 20% compared to the control group.
A multicentric study was conducted by Lopez-Lopez et al[11] to assess the accuracy of 3DPMs derived from original imaging sources for use in teaching, patient communication, and hepatobiliary surgery planning. The study included 35 patients from eight centers. Testing between 3DPMs and CT/MRI images showed a high degree of similarity in vascular calibers and distances between the tumor and vessels. There was a good correlation between 3DPMs and surgical specimens regarding the resection margin distance. Students demonstrated a higher success rate with 3DPMs compared to CT/MRI or 3D digital imaging. The findings suggest that 3DP hepatic models correlate well with CT/MRI and surgical pathology and are valuable for education, understanding, and surgical planning, although they do not necessarily influence surgical outcomes.
Joo et al[12] assessed the effectiveness of a personalized, 3DP transparent liver model with focal liver lesions (FLLs) for lesion-by-lesion imaging-pathologic matching. Twenty patients with multiple FLLs were included. After digital segmentation of the hepatobiliary phase MRI, a transparent, 3DP liver model was created, featuring colored anatomical structures and FLLs. The per-lesion detection rates were compared between gross examination using the 3DP liver model and routine protocol. The detection rate during gross examination with the 3DP liver model was 99.0%, which was significantly higher than the routine examination rate of 82.7%. The authors concluded that a personalized, 3DP liver model with FLLs significantly improved lesion-by-lesion imaging-pathologic matching, particularly for small FLLs, thus enhancing accurate pathologic tumor staging and provided a reliable reference for imaging-detected lesions.
Role of 3D printing in preoperative planning was also reinforced by Xiang et al[13] in their study on the role of liver 3D printing for the treatment of complex massive hepatocarcinoma with rare variations of the portal vein. The authors observed that the 3DP liver model accurately reflected the medical image 3D visualization system model. Surgical planning was based on the relationship between the tumor and portal vein variation. The residual liver volume calculated by 3D printing was only 21.37% due to the variant segment 4 portal vein (S4PV) originating from the right anterior portal vein. After optimization, the residual liver volume increased to 57.25% by performing a narrow-margin right hemihepatectomy with the variant S4PV preserved. The final resection was confirmed as a narrow-margin right hemihepatectomy, and the actual surgical procedure matched the preoperative planning. They concluded that the liver 3D printing is a safe and effective technique for improving surgical outcomes and reducing risks in patients with complex massive hepatocarcinoma and variations in the portal vein.
A study by Zeng et al[14] explored the construction and clinical efficacy of a 3D visualization platform for the diagnosis and treatment of hilar cholangiocarcinoma. A total of 32 patients with hilar cholangiocarcinoma were analyzed. The 3D visualization platform proved valuable in optimizing the preoperative surgical plan and provided a real-time intraoperative navigation, which enhanced surgical precision. This approach contributed to improved operational accuracy and facilitated better recovery outcomes for the patients.
Hepatobiliary tumors, which include liver and gallbladder cancers, are marked by a complex tumor microenvironment and extensive cellular heterogeneity. Conventional 2D culture models cannot fully mimic the real life tumor microenvironment. 3D bioprinting can be used to develop high throughput high fidelity multicellular models and is therefore potentially highly relevant for hepatobiliary surgery. Although it is still in the experimental stage, this subset of 3D printing, has a significant potential to improve hepatobiliary surgeries. The bionic organ models with advanced biological structures can also be important for medical training, but they have mechanical property, surgical feedback, and reproducibility deficiencies. Current studies are focused on creation of functional liver tissues by bioprinting for transplantation, and bile duct constructs for repair or replacement of damaged biliary structures[15].
In a study by Xiang et al[16], an artificial bile duct using 3D printing was successfully fabricated. It was composed of poly (lactic-co-glycolic acid) (PLGA) and gelatin methacrylate (GelMA). The PLGA inner layer provided adequate strength to support bile duct contraction, while the GelMA outer layer offered good biocompatibility for cell growth. Additionally, IKVAV laminin peptide (Ile-Lys-Val-Ala-Val) and ultrasmall superparamagnetic iron oxide (USPIO) were incorporated to enhance scaffold cell adhesion and enable MRI detection. Co-culture of bone marrow-derived stem cells (BMSCs) with IKVAV at a specific concentration significantly increased BMSC survival and adhesion. The fabricated scaffold exhibited a tensile modulus between 17.19 MPa and 29.05 MPa and a compressive modulus between 0.042 MPa and 0.066 MPa, suitable for human implantation. In an in vivo pig model of bile duct regeneration, the PLGA/GelMA/IKVAV/USPIO conduits promoted bile duct regeneration and enhanced cytokeratin 19 expression. This composite bile duct scaffold, with excellent MRI imaging functionality and biocompatibility, holds promise for the development of bioactive artificial bile ducts.
A study by Xu et al[17] presented a tissue-mimicking dual-network hydrogels with customizable stiffness, achieved by adjusting the hydrogel matrix composition and immersion time. Using 3D printing, models of the kidney, liver, pancreas, and vascular tissues were fabricated, simulating surgical scenarios such as suture handling, ultrasonic cutting, blood vessel coagulation, ultrasound visualization, and liver tumor ablation. These advanced biomimetic organ models with tunable properties have the potential to enhance surgical training, medical device testing, and medical education.
Similarly, Al-Thani et al[18] proposed a method to create a soft phantom model of the human liver using a 3DP mold, silicone, ballistic gel, and a blender. The elastic modulus of seven different silicone base-to-hardener ratios was tested, while ballistic gel models were created with 20% gelatin for the tumor and 10% gelatin for the healthy liver tissue. The results showed that the silicone modulus closely matched that of real liver tissue, and the 10% gelatin model effectively emulated healthy liver characteristics. The 3D liver phantom, made from a 10% gelatin-water mixture, demonstrated good texture and elasticity, making it a valuable tool for medical training, preoperative planning, and surgical research.
In a study by Jin et al[19], a concentric cylindrical tetra-culture model was developed to replicate the spatial or
3DP models are also used in the field of patient education and informed consent for real patients. Therefore, surgeons can actually give patients their own anatomy and the expected surgery in the form of a model to improve patients' understanding of their medical situation and the treatments to be expected. This can lead to greater patient satisfaction and anxiety reduction[1].
Giehl-Brown et al[1] found out that patients who underwent 3D modeling of the liver and tumors fared better in terms of disease and treatment understanding as compared to those who only relied on imaging. 3DPMs have found their use in surgical training and education and are a good imitation of the actual scenarios for the trainees to learn from and practice complicated maneuvers without necessarily putting a patient’s life at risk.
In their study, Yang et al[20] designed a new 3DP educational model for laparoscopic bile duct exploration and found it to be useful for beginners. This study involved 50 surgical residents who were allocated to two groups: Traditional training and training with 3DPMs. The participants who learned from the 3DPMs enhanced their procedural competency by 40% and shortened their learning curve by 30%[20]. In their work, they designed a portable and soft 3DP cast for laparoscopic choledochojejunostomy training. This new model can be used many times and the 40 surgical trainees who used it to train for three months showed 50% improvement in their technical skills.
In an attempt to facilitate surgical training Cheng et al[21] analyzed three laparoscopic hepatectomy cases using MDCT data to create 3D virtual reconstructions (3DVRs) and 3DPMs. Sixty-two interns were randomly assigned to three groups (3DPM, 3DVR, and MDCT) for a study following lecture-based education on hepatocellular carcinoma (HCC). After selecting an HCC model, the interns were tested on tumor location, adjacent vessels, surgical planning, and test time using a centesimal system within 90 minutes. A questionnaire assessed satisfaction, interest, and perceived effectiveness in improving liver anatomy and 3D spatial understanding. Results showed that the 3DPM group outperformed the 3DVR and MDCT groups in test scores, particularly in identifying tumor locations, tumor-vessel relationships, and surgical planning. The 3DPM group also reported higher satisfaction, interest, and helpfulness in improving understanding of liver anatomy and 3D spatial structures. These findings suggest that clinical teaching with 3DPM significantly enhances theoretical knowledge, clinical thinking, and teaching outcomes for medical interns studying HCC.
Shen et al[22] conducted a study on simulation training for laparoscopic bilioenteric anastomosis using a 3DP dry lab model. The study highlighted that an appropriate biliary-enteric anastomosis model can significantly aid surgeons in simulation training, helping them accumulate experience and refine skills for future real operations. The 3DP model performed effectively in this study, demonstrating its capability to fulfill this training objective.
Wei et al[23] conducted a study on reusable modular 3DP dry lab training models designed to simulate minimally invasive choledochojejunostomy (MICJ). The models were identified as a potentially valuable tool for improving surgeons' MICJ skills. These models offer several advantages, including modular structures that help reduce training costs while maintaining the quality and effectiveness of the training.
A major strength of VSP and 3D imaging is that it may increase the accuracy of surgical procedures. It has been established that the use of 3D imaging can assist the surgeon to visualize complex liver anatomy and other structures including the vascular and biliary systems. It has the potential to enhance preoperative planning, including the identification of tumors and blood vessels that may not be well seen in two dimensions.
According to Gussago et al[24], 3D models were most helpful in complex liver resections, and using them helped to avoid important blood vessels by improving the liver anatomy mapping.
Similarly, Fang et al[25] observed that VSP could help surgeons try different resection techniques, thus leading to more accurate cut lines with less need for intraoperative adjustments. These advantages were most evident in surgeries for tumors in difficult locations or with anatomical variants.
Using 3DPMs from CT or MRI, Oshiro et al[26] stated that the surgeon’s performance was enhanced in terms of liver resections and transplantations. This gave the surgeon a feel of what to expect in difficult cases and therefore made for better and more confident decisions in the actual operation.
Cheng et al[27] in their study explored the use of 3DP and indocyanine green (ICG) fluorescence imaging technology in complex laparoscopic hepatectomy (CLH) to assess the impact and value of this approach. A total of 30 patients underwent CLH using the conventional method, while 24 patients received CLH with 3DP and ICG fluorescence navigation. They concluded that 3DP and ICG fluorescence navigation allow for the selection of optimal surgical strategies for CLH, offering a safe and effective modification, though without significant improvements in intraoperative and short-term outcomes.
Qin et al[28] conducted a study on the efficacy of 3DP assisted percutaneous transhepatic one-step biliary fistulation (PTOBF) combined with rigid choledochoscopy for the treatment of intrahepatic bile duct stones. The study compared this approach with simple PTOBF combined with rigid choledochoscopy. The results indicated that the 3DPM-assisted PTOBF combined with rigid choledochoscopy is a safer and more effective method for treating intrahepatic bile duct stones.
The studies reviewed also evaluated the impact of 3D imaging and VSP on postoperative complications. The results were promising, with many studies reporting a reduction in complications such as bleeding, bile leaks, and prolonged recovery times.
Gavriilidis et al[29] and Zhang et al[30] highlighted that 3D imaging reduced the risk of intraoperative bleeding, as it provided more accurate visualization of the liver's vascular structures.
Liu et al[31] noted that VSP allowed for the identification and avoidance of critical bile ducts, significantly lowering the occurrence of bile duct injuries—a common complication in liver surgeries.
Moreover, Pereira da Silva et al[6] and Fukumitsu et al[32] both found that 3D imaging models improved surgical outcomes by minimizing the need for intraoperative adjustments, which typically contribute to complications. The enhanced ability to predict the course of surgery and visualize the patient’s specific anatomical features allowed for more controlled and less invasive procedures, ultimately reducing postoperative complications.
The studies also focused on patient outcomes such as recovery time, morbidity, and mortality. Several studies have indicated that 3D imaging and VSP result in better patient outcomes including shorter recovery times, fewer complications, and improved long term survival rates.
Yang et al[33] and Park et al[10] both observed that patients who underwent surgeries with preoperative planning based on 3D models had faster recovery times and fewer incidences of postoperative complications such as infections and biliary leaks. In particular, the studies showed that 3D imaging provided more accurate resections, reducing the need for additional surgeries or prolonged hospital stays.
Tomiyama et al[5] reported that the use of 3DP liver models for rehearsing complex surgeries before the actual procedure led to improved outcomes in terms of both immediate recovery and long-term survival. These findings suggest that better preoperative planning and visualization of the patient’s anatomy directly contribute to improved surgical outcomes.
Xia et al[34] used 3D models in laparoscopic choledochojejunostomy surgeries, which resulted in better alignment of surgical strategies, contributing to reduced operative times and enhanced patient satisfaction.
Li et al[35] and Yang et al[36] also found that these technologies improved the comprehension of liver anatomy by trainees, suggesting that incorporating 3D models into education could lead to more competent surgeons and better outcomes in the long term.
The integration of artificial intelligence (AI), augmented reality (AR), and robotic surgery with 3D imaging and VSP can transform hepato-pancreato-biliary (HPB) surgeries by enhancing the accuracy, efficiency, and safety of surgical procedures.
AI plays a crucial role in improving the processing and analysis of medical images, significantly enhancing the efficiency and accuracy of 3D imaging and VSP. AI-driven tools, through deep learning and machine learning models, automate image processing by segmenting and classifying anatomical structures such as tumors, blood vessels, and bile ducts. This automation speeds up image interpretation, reduces the risk of errors, and improves surgical planning. Moreover, AI can predict potential complications or anatomical variations based on large datasets, optimizing surgical decision-making[30]. AI algorithms can also suggest the most effective surgical approaches by analyzing patient-specific features and historical data, allowing surgeons to focus on high-level decisions while relying on AI for routine tasks like image analysis and planning.
AR, on the other hand, enhances 3D imaging and VSP by providing real-time, interactive visualizations during surgery. AR overlays digital 3D models of the patient's anatomy onto the surgeon's view of the operative field, allowing for real-time navigation of complex tissue layers and structures. In HPB surgeries, AR can assist in visualizing critical structures such as the liver, bile ducts, and blood vessels in three dimensions during the operation. This is particularly valuable in intricate procedures like liver resections or bile duct reconstructions, where precision is paramount. AR technology also adapts in real-time to intraoperative data, adjusting visualizations based on changes in tissue color or shape, which allows surgeons to make informed decisions during the surgery[31]. This dynamic visualization is especially beneficial in minimally invasive surgeries, where direct visualization of the surgical field is limited.
Robotic surgery, when integrated with 3D imaging and VSP, provides enhanced precision and control, especially in the complex anatomy of HPB surgeries. Robotic systems like the da Vinci Surgical System offer superior dexterity, fine motor control, and the ability to make precise movements in confined spaces. These systems allow surgeons to interact with virtual 3D models during the procedure, providing real-time feedback and enabling adjustments based on the preo
The combination of AI, AR, and robotic surgery creates a synergistic effect that optimizes 3D imaging and VSP. AI improves the accuracy of preoperative planning by analyzing medical images and suggesting surgical strategies, while AR provides real-time, interactive visualizations during surgery. Robotic systems further enhance precision by executing the planned surgical movements with millimeter accuracy. Together, these technologies enable surgeons to make real-time decisions and adapt to unexpected challenges during complex HPB surgeries, improving surgical outcomes, minimizing complications, reducing recovery times, and enhancing overall patient safety. By integrating AI, AR, and robotic surgery with 3D imaging and VSP, the landscape of hepatobiliary surgeries is being reshaped, providing more personalized and effective care for patients.
Based on the results of this review, it appears that 3D imaging and VSP may hold promise in enhancing the accuracy of hepatobiliary surgeries, limiting complications, and improving patients’ results. These technologies provide a better individualized method for surgery than the current standard of care, which is based on 2D images. This can lead to better surgeries, fewer complications, and faster recovery times. Therefore, healthcare institutions should embrace 3D imaging and VSP into their regular clinical practice. Preoperative rehearsals are particularly useful for surgeons to identify potential problems and design the best strategy to tackle them. Also, surgical residents and fellows should be trained in the use of 3D imaging and VSP technologies to enhance their performance in the performance of complex procedures.
The implementation of advanced technologies like 3D imaging and VSP in low- and middle-income countries (LMICs) faces significant financial and resource-related challenges, including high equipment costs, ongoing maintenance expenses, and the need for specialized training. Acquiring imaging systems such as CT and MRI scanners is prohibitively expensive for many LMICs, where public healthcare budgets are limited, and maintenance costs further strain resources, particularly in settings with a shortage of trained personnel. Additionally, VSP and 3D imaging require specialized training for healthcare professionals, but the scarcity of qualified personnel and the difficulty in recruiting experts to underserved areas hinder widespread adoption. Infrastructure limitations, such as unreliable electricity, poor internet connectivity, and inadequate data management systems, further impede the integration of these technologies, while weak cybersecurity measures pose risks to patient data. Moreover, healthcare spending in LMICs is often prioritized for immediate needs like infectious disease control and maternal health, making costly technological investments less feasible within constrained national budgets. Given these barriers, overcoming the financial and logistical hurdles to implementing 3D imaging and VSP in LMICs will require innovative financing strategies, international collaboration, and context-specific solutions that align with the realities of resource-limited healthcare systems.
The integration of 3D imaging and VSP in HPB surgeries presents various regulatory, standardization, and legal challenges that need to be addressed to ensure safe and effective implementation. These challenges are crucial in facilitating the widespread adoption of these technologies, ensuring patient safety, and protecting both healthcare providers and patients. The regulatory approval is critical to ensuring their safety and efficacy in clinical practice. Agencies such as the United States Food and Drug Administration, European Medicines Agency, and India's Central Drugs Standard Control Organization oversee the approval processes for medical technologies, including imaging devices and surgical planning software.
For 3D imaging technologies, such as CT and MRI scans, and VSP software, the approval process typically involves ensuring the accuracy, reliability, and clinical utility of these tools. Regulatory bodies often require clinical trials and substantial evidence to validate the technology's safety and effectiveness before it can be used in clinical settings. This includes ensuring that the software used for VSP can produce precise, reproducible 3D reconstructions from medical images and accurately simulate surgical outcomes. However, the approval process can vary significantly across different regions. For instance, in the United States, VSP software might be classified as “software as a medical device,” which requires regulatory approval. Similarly, the introduction of the Medical Devices Regulation in Europe in 2021 has raised the standards for medical software, including VSP applications[15].
As the use of 3D imaging and VSP becomes more widespread in HPB surgeries, the need for standardization grows. Standardization ensures that these technologies meet universal quality and safety benchmarks and facilitates their integration across various healthcare institutions, regardless of their geographic location or resources. It also promotes interoperability, allowing for better data exchange and collaboration between healthcare providers.
Currently, there is no universally accepted standard for using 3D imaging and VSP, particularly concerning data processing, image reconstruction, and virtual simulation[15]. The lack of standard protocols can lead to discrepancies in image quality and surgical planning accuracy, which may negatively impact surgical outcomes. Standardizing practices for imaging acquisition, data processing, and virtual simulation is critical to ensuring that every healthcare provider follows best practices. Additionally, it would make these technologies more accessible and usable, particularly in low-resource settings, such as LMICs, where technology adoption and training might be limited.
Several legal challenges are associated with the use of 3D imaging and VSP in HPB surgeries. One of the main concerns is the question of liability in case of surgical errors or complications. Traditionally, surgeons are held accountable for the outcomes of their procedures, but the introduction of advanced technologies complicates this responsibility. In cases where complications arise due to inaccurate 3D imaging or VSP systems, it may be unclear whether the surgeon, the software provider, or the healthcare institution should be held responsible[12]. Legal frameworks need to be developed to assign clear responsibility for technological failures and errors, taking into account whether the system was properly validated and if the surgeon was adequately trained to use the technology.
Another key legal concern involves patient data privacy and security. The collection, storage, and transmission of sensitive medical data are integral components of 3D imaging and VSP systems. Legal frameworks such as the General Data Protection Regulation (GDPR) in Europe and the Health Insurance Portability and Accountability Act (HIPAA) in the United States govern the protection of patient data. Any breach of confidentiality or unauthorized access to medical data could result in legal consequences, including lawsuits and regulatory penalties. Healthcare institutions must ensure robust cybersecurity measures and adherence to data protection laws to prevent potential breaches and protect patient privacy.
Future work should continue to standardize 3D printing protocols so that they can be compared and repeated in other institutions and applications. Enhancing the material properties to mimic more closely the feel of tissue, making the simulations and planning models more realistic. Perform more extensive clinical trials to determine the long term effectiveness of 3D printing in improving surgical outcome, including the cost analysis. Investigate the possibility of combing 3D printing with other modern technologies like augmented reality and artificial intelligence to develop better surgical planning and training resources. Investigate the possibility of applying 3D bioprinting for the fabrication of a functional liver tissue for transplantation and thus open new opportunities for the field of organ transplantation. 3D printing is showing a great potential in hepatobiliary surgery but there are several key challenges that exist; the variability in the models produced, the high costs of developing patient specific models and the relative novelty of the field for surgeons. The cost of the 3D printing technology and the time needed to build the patient's model may be unfeasible in limited resource settings. The use of 3DPMs and guides in surgery demands a high degree of accuracy which needs to be proven before they can be used in practice. Additionally, the ability of bioprinting to create transplantable tissues has an ethical dimension concerning the source of cells and the effects of such procedures in the long run.
The integration of 3D imaging and VSP into HPB surgeries has led to significant advancements in surgical precision and patient outcomes. However, these technologies also introduce several ethical concerns, particularly regarding patient consent, data privacy, and surgeon responsibility. As medical technology continues to evolve, these issues must be carefully addressed to ensure that patient rights and medical integrity are not compromised.
One of the primary ethical concerns is patient consent. Traditional surgical planning involves a straightforward informed consent process, where patients are briefed about the procedure, risks, and expected outcomes. However, with the advent of 3D imaging and VSP, patients must be informed about how these technologies contribute to the treatment planning. Informed consent should extend beyond general surgical risks to include details about the creation of anatomical models from imaging and the simulation of surgical approaches through VSP. Healthcare providers must ensure that patients understand the potential risks, such as errors in imaging or virtual simulations, which could affect surgical accuracy[37]. Given the complexity of these technologies, patients need clear and accessible explanations of how their medical data will be used and the implications of its use, particularly in educational or research contexts.
Data privacy and security present another critical ethical issue. The collection, storage, and transmission of sensitive medical data, such as CT scans, MRIs, and virtual models of anatomy, require robust protections against unauthorized access, cyberattacks, and data breaches. Medical data is often governed by stringent privacy laws, such as HIPAA in the United States or the GDPR in Europe. However, the digital nature of 3D imaging and VSP heightens the risk of data exposure. In particular, global or cross-border sharing of patient data can complicate adherence to varying data protection regulations, potentially jeopardizing patient confidentiality[14]. Therefore, healthcare institutions must implement strong cybersecurity protocols to ensure that patient data is encrypted, securely stored, and accessible only to authorized personnel. Transparent data handling practices are essential to maintain patient trust and address privacy concerns.
Finally, the responsibility placed on surgeons using 3D imaging and VSP must be considered. While these technologies enhance surgical planning and execution, they also create the risk of overreliance on digital models, potentially diminishing the surgeon’s clinical judgment. Surgeons must remain vigilant, particularly when unexpected anatomical variations or intraoperative complications arise that the virtual models may not have anticipated. Overdependence on technology could lead to missed critical observations that are not captured by digital simulations[32]. Additionally, the accuracy of 3D imaging and VSP depends on the quality of the data and software used to create the models. Any flaws in the data, such as an inaccurate scan or malfunctioning software, could lead to incorrect surgical plans. Surgeons must be trained to recognize the limitations of these technologies and ensure that their decisions remain adaptable to the realities of the operating room
This systematic review demonstrates the potential of 3D imaging and VSP to change the practice of hepatobiliary surgery. 3D imaging can be an useful tool in modern hepatobiliary surgery, especially in complicated operations. It increases the surgical accuracy, decreases the complications and enhances the patients' results. However, there are some limitations of the current evidence based on the findings of this review, it can be argued that these technologies may be capable of changing the practice by offering specific, precise and timely surgical planning. The current study is also consistent with the previous studies that have established the effectiveness of VSP in improving patients’ QoL after surgery and reducing post-operative complications. Further developments in 3D imaging, AI and augmented reality will likely expand the role of VSP in the future to produce better results for patients with complex hepatobiliary surgeries. Table 1 depicts the summary of included studies.
| S.No | Ref. | Study title | Conclusion/Key |
| 1 | Giehl-Brown et al[1] | 3D liver model-based surgical education improves preoperative decision-making and patient satisfaction | 3D liver model-based education improves preoperative decision-making and patient satisfaction |
| 2 | Yao et al[2] | Precise planning based on 3D-printed dry-laboratory models | 3D-printed models help reduce perioperative complications in laparoscopic surgery |
| 3 | Tomiyama et al[5] | Patient-specific rehearsals for complex liver surgeries with 3D-printed model | Highlights the use of patient-specific 3D models for complex liver surgeries |
| 4 | Pereira da Silva et al[6] | Advanced hepatic vasculobiliary imaging segmentation and 3D reconstruction | Describes the role of 3D imaging in managing high biliary stenosis |
| 5 | Park et al[10] | Improved graft survival by using 3D printing of intra-abdominal cavity to prevent large-for-size syndrome in liver transplantation | 3D printing helps prevent large-for-size syndrome in liver transplantation |
| 6 | Lopez-Lopez et al[11] | Applicability of 3D-printed models in hepatobiliary surgery: Results from 'LIV3DPRINT' multicenter study | 3D-printed models are useful in hepatobiliary surgery |
| 7 | Joo et al[12] | Personalized 3D-printed transparent liver model using the hepatobiliary phase MRI | Highlights the usefulness of MRI-guided 3D-printed liver models for lesion-pathology matching |
| 8 | Xiang et al[13] | Application of liver 3D printing in hepatectomy for complex massive hepatocarcinoma with rare variations of portal vein: Preliminary experience | Shows the application of 3D printing in hepatectomy for complex hepatocarcinoma |
| 9 | Zeng et al[14] | The construction of 3D visualization platform and its application in diagnosis and treatment for hilar cholangiocarcinoma | Describes the role of 3D visualization in diagnosing and treating hilar cholangiocarcinoma. |
| 10 | Xiang et al[16] | Production and characterization of an integrated multilayer 3D-printed PLGA/GelMA scaffold aimed for bile duct restoration and detection | Focuses on the development of a multilayer 3D scaffold for bile duct restoration |
| 11 | Xu et al[17] | Multifunctional high-simulation 3D-printed hydrogel model manufacturing engineering for surgical training | Explores the use of high-simulation 3D-printed hydrogel models in surgical training |
| 12 | Al-Thani et al[18] | Development of a flexible liver phantom for hepatocellular carcinoma treatment planning: A useful tool for training & education | Introduces a flexible liver phantom as a tool for hepatocellular carcinoma treatment planning |
| 13 | Jin et al[19] | Multicellular 3D-bioprinted human gallbladder carcinoma for in vitro mimicking of tumor microenvironment and intratumoral heterogeneity | Describes the creation of a bioprinted gallbladder carcinoma for in vitro tumor environment modeling |
| 14 | Yang et al[20] | A novel 3D-printed educational model for the training of laparoscopic bile duct exploration: A pilot study for beginning trainees | Introduces a novel 3D-printed model for laparoscopic bile duct exploration training |
| 15 | Cheng et al[21] | Comparison of 3D printing model to 3D virtual reconstruction and 2D imaging for the clinical education of interns in hepatocellular carcinoma | Compares 3D printing models with virtual reconstruction for teaching hepatocellular carcinoma to interns |
| 16 | Shen et al[22] | A study of simulation training in laparoscopic bilioenteric anastomosis on a 3D-printed dry lab model | Explores simulation training for laparoscopic bilioenteric anastomosis using 3D models |
| 17 | Wei et al[23] | Reusable modular 3D-printed dry lab training models to simulate minimally invasive choledochojejunostomy | 3D-printed models for training minimally invasive choledochojejunostomy |
| 18 | Gussago et al[24] | 3D printing and liver surgery: Scenic gadget or useful tool? | Examines the effectiveness of 3D printing in liver surgery |
| 19 | Fang et al[25] | Consensus recommendations of 3D visualization for diagnosis and management of liver diseases | Provides consensus on the use of 3D visualization for liver disease management |
| 20 | Oshiro et al[26] | A novel 3D print of liver vessels and tumors in hepatectomy | Describes the use of 3D printing for liver vessels and tumors in hepatectomy |
| 21 | Cheng et al[27] | Value of 3D printing technology combined with indocyanine green fluorescent navigation in complex laparoscopic hepatectomy | Shows the value of combining 3D printing with indocyanine green fluorescence in laparoscopic hepatectomy |
| 22 | Qin et al[28] | Efficacy of 3D-printed assisted percutaneous transhepatic one-step biliary fistulation combined with rigid choledochoscopy for intrahepatic bile duct stones | Examines 3D-printed models in assisting biliary fistulation for intrahepatic bile duct stones |
| 23 | Gavriilidis et al[29] | Navigated liver surgery: State of the art and future perspectives | Explores the state-of-the-art and future perspectives of navigated liver surgery |
| 24 | Zhang et al[30] | Fabrication of agarose concave petridish for 3D-culture microarray method for spheroids formation of hepatic cells | Discusses a 3D-culture method for hepatic cell spheroid formation |
| 25 | Liu et al[31] | 3D modeling in complex liver surgery and liver transplantation | Describes the application of 3D modeling in complex liver surgery and transplantation |
| 26 | Fukumitsu et al[32] | Impact of patient-specific 3D-printed liver models on hepatic surgery safety: A pilot study | Pilot study on the impact of patient-specific 3D liver models on surgery safety |
| 27 | Yang et al[33] | Application of VR and 3D printing in liver reconstruction | Discusses the application of VR and 3D printing in liver reconstruction |
| 28 | Xia et al[34] | Development and evaluation of a portable and soft 3D-printed cast for laparoscopic choledochojejunostomy model in surgical training | Evaluates a portable 3D-printed model for laparoscopic choledochojejunostomy training |
| 29 | Li et al[35] | The use of 3D printing model in the training of choledochoscopy techniques | Explores the use of 3D models in choledochoscopy technique training |
| 30 | Yang et al[36] | Impact of 3D printing technology on the comprehension of surgical liver anatomy | Studies the impact of 3D printing on understanding liver anatomy in surgery |
This review provides a complete assessment of the current research on 3D imaging and VSP in hepatobiliary surgery. In analyzing data from 30 studies, it offers a general view on the impact of these technologies on surgical practice. The inclusion of studies with different methodologies and patient populations increases the credibility of the findings. Moreover, the review follows the PRISMA guidelines, which ensures that the reporting of the study is transparent and consistent. The concentration on surgical accuracy, complications, and patient results are important aspects of clinical practice and give a comprehensive view of the possible advantages and disadvantages of applying 3D imaging and VSP in hepatobiliary surgery.
As a result of this review, the results are quite encouraging, however there are several limitations that cannot be overlooked. The research that has been carried out up to this day has been mainly descriptive or retrospective in nature and a very few numbers of randomized controlled trials. However, such studies are liable to certain limitations, such as selection bias and information bias. A definite statement of the causal relationship and the conclusions should be treated with some reserve. Also, the great majority of the research reviewed for the present article had limited sample sizes, which hampers the extent to which the findings can be applied elsewhere. Larger, more representative studies are required to replicate the results and extend them to other forms of hepatobiliary surgery. Another is the fact that there are no established guidelines for applying 3D imaging and VSP technologies. The tools, software, and techniques employed in the cited studies were quite diverse, which makes it challenging to identify the most effective approaches. Many studies reviewed have small sample sizes, limiting their generalizability and reducing statistical power. This increases the risk of Type II errors, making it harder to detect meaningful differences in surgical outcomes. Small, homogeneous study groups fail to reflect real-world clinical diversity, where variations in age, comorbidities, and disease stages influence treatment effectiveness. Consequently, findings may not accurately represent broader patient populations. To overcome these limitations, future research should focus on large-scale, multicenter studies that include diverse demographic backgrounds, disease etiologies, and comorbidities. Such studies would improve the applicability of findings in heterogeneous clinical settings. Additionally, meta-analyses or pooled data analyses could aggregate data from smaller studies, increasing statistical power and providing stronger conclusions on the efficacy and safety of 3D imaging and VSP. By addressing these limitations, future research can offer more definitive evidence, improving clinical decision-making and enhancing patient outcomes in surgical practice.
The variability in imaging technologies and methodologies across studies is a significant challenge in establishing a standardized approach for 3D imaging and VSP. Different studies utilize a range of imaging modalities and software platforms, leading to heterogeneity in outcomes. To minimize the impact of this variability, we advocate for the development of standardized protocols for 3D imaging acquisition and VSP. Multicenter studies with consistent methodologies would provide more robust data on the efficacy of these technologies in clinical practice.
| 1. | Giehl-Brown E, Dennler S, Garcia SA, Seppelt D, Oehme F, Schweipert J, Weitz J, Riediger C. 3D liver model-based surgical education improves preoperative decision-making and patient satisfaction-a randomized pilot trial. Surg Endosc. 2023;37:4545-4554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 2. | Yao WF, Huang XK, Fu TW, Jin L, Du CF, Gao ZY, Wang KD, Dai MG, Liu SY, Liu JW, Zhang CW, Liang L, Huang DS. Precise planning based on 3D-printed dry-laboratory models can reduce perioperative complications of laparoscopic surgery for complex hepatobiliary diseases: a preoperative cohort study. BMC Surg. 2024;24:148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 3. | Wang Y, Cao D, Chen SL, Li YM, Zheng YW, Ohkohchi N. Current trends in three-dimensional visualization and real-time navigation as well as robot-assisted technologies in hepatobiliary surgery. World J Gastrointest Surg. 2021;13:904-922. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 28] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (2)] |
| 4. | Berardi G, Colasanti M, Meniconi RL, Ferretti S, Guglielmo N, Mariano G, Burocchi M, Campanelli A, Scotti A, Pecoraro A, Angrisani M, Ferrari P, Minervini A, Gasparoli C, Wakabayashi G, Ettorre GM. The Applications of 3D Imaging and Indocyanine Green Dye Fluorescence in Laparoscopic Liver Surgery. Diagnostics (Basel). 2021;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Tomiyama K, Ghazi A, Hernandez-Alejandro R. Looking Beyond the Horizon: Patient-Specific Rehearsals for Complex Liver Surgeries With 3D Printed Model. Ann Surg. 2021;273:e28-e30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Pereira da Silva N, Abreu I, Serôdio M, Ferreira L, Alexandrino H, Donato P. Advanced hepatic vasculobiliary imaging segmentation and 3D reconstruction as an aid in the surgical management of high biliary stenosis. BMC Med Imaging. 2020;20:120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Aseni P, Santaniello T, Rizzetto F, Gentili L, Pezzotta F, Cavaliere F, Vertemati M, Milani P. Hybrid Additive Fabrication of a Transparent Liver with Biosimilar Haptic Response for Preoperative Planning. Diagnostics (Basel). 2021;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Oshiro Y, Ohkohchi N. Three-Dimensional Liver Surgery Simulation: Computer-Assisted Surgical Planning with Three-Dimensional Simulation Software and Three-Dimensional Printing. Tissue Eng Part A. 2017;23:474-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Ahmed F, Jahagirdar V, Gudapati S, Mouchli M. Three-dimensional visualization and virtual reality simulation role in hepatic surgery: Further research warranted. World J Gastrointest Surg. 2022;14:723-726. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Park S, Choi GS, Kim JM, Lee S, Joh JW, Rhu J. Improved graft survival by using three-dimensional printing of intra-abdominal cavity to prevent large-for-size syndrome in liver transplantation. Ann Hepatobiliary Pancreat Surg. 2025;29:21-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 11. | Lopez-Lopez V, Robles-Campos R, García-Calderon D, Lang H, Cugat E, Jiménez-Galanes S, Férnandez-Cebrian JM, Sánchez-Turrión V, Fernández-Fernández JM, Barrera-Gómez MÁ, de la Cruz J, Lopez-Conesa A, Brusadin R, Gomez-Perez B, Parrilla-Paricio P. Applicability of 3D-printed models in hepatobiliary surgey: results from "LIV3DPRINT" multicenter study. HPB (Oxford). 2021;23:675-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 12. | Joo I, Kim JH, Park SJ, Lee K, Yi NJ, Han JK. Personalized 3D-Printed Transparent Liver Model Using the Hepatobiliary Phase MRI: Usefulness in the Lesion-by-Lesion Imaging-Pathologic Matching of Focal Liver Lesions-Preliminary Results. Invest Radiol. 2019;54:138-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Xiang N, Fang C, Fan Y, Yang J, Zeng N, Liu J, Zhu W. Application of liver three-dimensional printing in hepatectomy for complex massive hepatocarcinoma with rare variations of portal vein: preliminary experience. Int J Clin Exp Med. 2015;8:18873-18878. [PubMed] |
| 14. | Zeng N, Fang CH, Fan YF, Yang J, Xiang N, Zhu W, Liu J, Cai W, Mo ZK. [The construction of three-dimensional visualization platform and its application in diagnosis and treatment for hilar cholangiocarcinoma]. Zhonghua Wai Ke Za Zhi. 2016;54:680-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 15. | Bangeas P, Tsioukas V, Papadopoulos VN, Tsoulfas G. Role of innovative 3D printing models in the management of hepatobiliary malignancies. World J Hepatol. 2019;11:574-585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 16. | Xiang Y, Wang W, Gao Y, Zhang J, Zhang J, Bai Z, Zhang S, Yang Y. Production and Characterization of an Integrated Multi-Layer 3D Printed PLGA/GelMA Scaffold Aimed for Bile Duct Restoration and Detection. Front Bioeng Biotechnol. 2020;8:971. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 17. | Xu X, Yu S, Ma L, Mao J, Chen H, Zhu Z, Wang L, Lin H, Zhang J, Wang Z. Multifunctional high-simulation 3D-printed hydrogel model manufacturing engineering for surgical training. Int J Bioprint. 2023;9:766. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 18. | Al-Thani A, Sharif A, El Borgi S, Abdulla S, Ahmed Saleh MR, Al-Khal R, Velasquez C, Aboumarzouk O, Dakua SP. Development of a flexible liver phantom for hepatocellular carcinoma treatment planning: a useful tool for training & education. 3D Print Med. 2024;10:24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 19. | Jin Y, Zhang J, Xing J, Li Y, Yang H, Ouyang L, Fang Z, Sun L, Jin B, Huang P, Yang H, Du S, Sang X, Mao Y. Multicellular 3D bioprinted human gallbladder carcinoma forin vitromimicry of tumor microenvironment and intratumoral heterogeneity. Biofabrication. 2024;16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 20. | Yang Z, Tong Y, Duan D, Xin W, Li H, Yi J, He X, Bao G. A novel 3D-printed educational model for the training of laparoscopic bile duct Exploration:a pilot study for beginning trainees. Heliyon. 2024;10:e36689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 21. | Cheng J, Wang ZF, Yao WF, Liu JW, Lu Y, Wang Q, Cai XJ. Comparison of 3D printing model to 3D virtual reconstruction and 2D imaging for the clinical education of interns in hepatocellular carcinoma: a randomized controlled study. J Gastrointest Oncol. 2023;14:325-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 22. | Shen J, Chen M, Jin R, Wang Z, Yang J. A study of simulation training in laparoscopic bilioenteric anastomosis on a 3D-printed dry lab model. Surg Endosc. 2023;37:337-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | Wei F, Wang W, Gong H, Cao J, Chen J, Chen H, Wang Z. Reusable Modular 3D-Printed Dry Lab Training Models to Simulate Minimally Invasive Choledochojejunostomy. J Gastrointest Surg. 2021;25:1899-1901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (1)] |
| 24. | Gussago S, Fournier I. 3D printing and liver surgery: scenic gadget or useful tool? Reponse to "applicability of 3D-printed models in hepatobiliary surgey: results from "LIV3DPRINT" multicenter study". HPB (Oxford). 2022;24:1585. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 25. | Fang C, An J, Bruno A, Cai X, Fan J, Fujimoto J, Golfieri R, Hao X, Jiang H, Jiao LR, Kulkarni AV, Lang H, Lesmana CRA, Li Q, Liu L, Liu Y, Lau W, Lu Q, Man K, Maruyama H, Mosconi C, Örmeci N, Pavlides M, Rezende G, Sohn JH, Treeprasertsuk S, Vilgrain V, Wen H, Wen S, Quan X, Ximenes R, Yang Y, Zhang B, Zhang W, Zhang P, Zhang S, Qi X. Consensus recommendations of three-dimensional visualization for diagnosis and management of liver diseases. Hepatol Int. 2020;14:437-453. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 90] [Article Influence: 15.0] [Reference Citation Analysis (1)] |
| 26. | Oshiro Y, Mitani J, Okada T, Ohkohchi N. A novel three-dimensional print of liver vessels and tumors in hepatectomy. Surg Today. 2017;47:521-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 27. | Cheng J, Wang Z, Liu J, Dou C, Yao W, Zhang C. Value of 3D printing technology combined with indocyanine green fluorescent navigation in complex laparoscopic hepatectomy. PLoS One. 2022;17:e0272815. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 28. | Qin J, He Y, Ma L, Duan J, Duan R, Liu R, Zhou J, Yang N, Li Y, Xiong Y, Li H, Zeng X, Li C, Li X. Efficacy of 3D-printed assisted percutaneous transhepatic one-step biliary fistulation combined with rigid choledochoscopy for intrahepatic bile duct stones. Dig Liver Dis. 2023;55:1699-1704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 29. | Gavriilidis P, Edwin B, Pelanis E, Hidalgo E, de'Angelis N, Memeo R, Aldrighetti L, Sutcliffe RP. Navigated liver surgery: State of the art and future perspectives. Hepatobiliary Pancreat Dis Int. 2022;21:226-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 30. | Zhang B, Li Y, Wang G, Jia Z, Li H, Peng Q, Gao Y. Fabrication of agarose concave petridish for 3D-culture microarray method for spheroids formation of hepatic cells. J Mater Sci Mater Med. 2018;29:49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (1)] |
| 31. | Liu JP, Lerut J, Yang Z, Li ZK, Zheng SS. Three-dimensional modeling in complex liver surgery and liver transplantation. Hepatobiliary Pancreat Dis Int. 2022;21:318-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 32. | Fukumitsu K, Ishii T, Ogiso S, Yoh T, Uchida Y, Ito T, Seo S, Hata K, Uemoto S, Hatano E. Impact of patient-specific three-dimensional printed liver models on hepatic surgery safety: a pilot study. HPB (Oxford). 2023;25:1083-1092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 33. | Yang J, Li E, Wu L, Liao W. Application of VR and 3D printing in liver reconstruction. Ann Transl Med. 2022;10:915. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 34. | Xia J, Mao J, Chen H, Xu X, Zhang J, Yang J, Wang Z. Development and evaluation of a portable and soft 3D-printed cast for laparoscopic choledochojejunostomy model in surgical training. BMC Med Educ. 2023;23:77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 35. | Li A, Tang R, Rong Z, Zeng J, Xiang C, Yu L, Zhao W, Dong J. The Use of Three-Dimensional Printing Model in the Training of Choledochoscopy Techniques. World J Surg. 2018;42:4033-4038. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 36. | Yang T, Lin S, Xie Q, Ouyang W, Tan T, Li J, Chen Z, Yang J, Wu H, Pan J, Hu C, Zou Y. Impact of 3D printing technology on the comprehension of surgical liver anatomy. Surg Endosc. 2019;33:411-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 49] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 37. | Boyer CJ, Boktor M, Samant H, White LA, Wang Y, Ballard DH, Huebert RC, Woerner JE, Ghali GE, Alexander JS. 3D Printing for Bio-Synthetic Biliary Stents. Bioengineering (Basel). 2019;6:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/