Published online Oct 28, 2021. doi: 10.13105/wjma.v9.i5.462
Peer-review started: April 13, 2021
First decision: June 24, 2021
Revised: July 1, 2021
Accepted: August 23, 2021
Article in press: August 23, 2021
Published online: October 28, 2021
Processing time: 198 Days and 6.5 Hours
Minimally invasive hepatectomy techniques have developed rapidly since 2000. Pure laparoscopic liver resection (LLR) has become the primary approach for managing liver tumors and procuring donor organs for liver transplantation. Robotic liver resection (RLR) has emerged during the last decade. The technical status of RLR seems to be improving.
To conduct a systematic review and meta-analysis comparing the short-term clinical outcomes of LLR and RLR over two 5-year periods.
A systematic literature search was performed using PubMed and Medline, including the Cochrane Library. The following inclusion criteria were set for the meta-analysis: (1) Studies comparing LLR vs RLR; and (2) Studies that described clinical outcomes, such as the operative time, intraoperative bleeding, intraoperative conversion rate, and postoperative complications.
A total of 25 articles were included in this meta-analysis after 40 articles had been subjected to full-text evaluations. The studies were divided into early (n = 14) and recent (n = 11) groups. In the recent group, the operative time did not differ significantly between LLR and RLR (P = 0.70), whereas in the early group the operative time of LLR was significantly shorter than that of RLR (P < 0.001).
The initial disadvantages of RLR, such as its long operation time, have been overcome during the last 5 years. The other clinical outcomes of RLR are comparable to those of LLR. The cost and quality-of-life outcomes of RLR should be evaluated in future studies to promote its routine clinical use.
Core Tip: A systematic review and meta-analysis comparing the clinical outcomes of laparoscopic liver resection (LLR) and robotic liver resection (RLR) was conducted. A total of 25 studies were included in the meta-analysis. In the recent studies, operative time did not differ significantly between LLR and RLR (P = 0.70), whereas in the early studies LLR was associated with significantly shorter operative times than RLR (P < 0.001). The initial disadvantages of RLR have been overcome during the last 5 years.
- Citation: Ishinuki T, Ota S, Harada K, Meguro M, Kawamoto M, Kutomi G, Tatsumi H, Harada K, Miyanishi K, Takemasa I, Ohyanagi T, Hui TT, Mizuguchi T. Maturation of robotic liver resection during the last decade: A systematic review and meta-analysis. World J Meta-Anal 2021; 9(5): 462-473
- URL: https://www.wjgnet.com/2308-3840/full/v9/i5/462.htm
- DOI: https://dx.doi.org/10.13105/wjma.v9.i5.462
Surgery is a curative treatment for liver tumors[1]. The development of surgical devices has promoted minimally invasive surgery (MIS), including minimally invasive liver resection[2]. Therefore, the concept of ‘big surgeons, big incision’ has become a myth[3]. Minimal skin wounds are preferable, and patients who undergo laparoscopic liver resection (LLR) recover faster without somatic pain than those that undergo open liver resection[1,4].
MIS has significant clinical benefits, e.g., it results in faster recovery, less pain, and shorter hospital stays[5]. On the other hand, long operation times and the associated higher costs were reported as disadvantages of the MIS approach[4,5]. However, the disadvantages of the MIS approach might be ameliorated as surgeons gain experience[6]. Initially, LLR was reported to have various clinical benefits but result in longer operation times[4].
Robotic surgery has gained popularity since 2000[7]. Although robotic towers occupy space in the operating room, the skill of surgeons can be enhanced by robotic technology, such as “wristed instruments”, “tremor cancellation”, “enhanced dexterity”, and “3D vision”[8,9]. These technologies are considered to reduce 93% of errors associated with human skill[8].
Total robotic liver resection (RLR) is limited to minor liver resection, which does not require the liver to be mobilized[10]. Furthermore, the robotic approach is only used for parenchymal dissection during laparoscopic surgery[11]. Therefore, the clinical outcomes of LLR and RLR should be similar[5,12]. We systematically reviewed the literature in which the clinical outcomes of LLR and RLR were compared. We divided the studies according to the year of publication to determine how the clinical outcomes of these techniques have changed over time. Early studies were defined as those published in 2016 or earlier. Recent studies were defined as those published in 2017 or later. We also examined the current status of RLR through a meta-analysis.
The Preferred Reporting Items for Systematic Reviews And Meta-Analyses (PRISMA) statement guidelines were followed when obtaining and reporting the meta-analysis data[13]. The PICOS scheme was employed when reporting the inclusion criteria. A systematic literature search of PubMed and MEDLINE, including the Cochrane Library, was performed independently by two authors (Ishinuki T and Ota S). The search was limited to human studies whose findings were reported in English. No restriction was set with regard to the type of publication, the publication date, or publication status. Patients of any age or sex who underwent liver resection for any hepatic lesion were considered, as outlined in the PICOS scheme. The search strategy was based on different combinations of words for each database. For the PubMed database the following combination was used: ("hepatectomy"[MeSH Terms] OR "hepatectomy"[All Fields] OR ("liver"[All Fields] AND "resection"[All Fields]) OR "liver resection"[All Fields]) AND ("laparoscopie"[All Fields] OR "laparoscopy"[MeSH Terms] OR "laparoscopy"[All Fields] OR "laparoscopies"[All Fields]) AND ("robot"[All Fields] OR "robot s"[All Fields] OR "robotically"[All Fields] OR "robotics"[MeSH Terms] OR "robotics"[All Fields] OR "robotic"[All Fields] OR "robotization"[All Fields] OR "robotized"[All Fields] OR "robots"[All Fields]). For the MEDLINE database, including the Cochrane Library database, the following combination was used: #1. liver.mp. [mp=title, abstract, full text, caption text], #2. resection.mp. [mp=title, abstract, full text, caption text], #3. robot.mp. [mp=title, abstract, full text, caption text], #4. 1 and 2 and 3.
The independent authors have read the primary studies searched in the database. Similar studies and unrelated studies were excluded. The inclusion criteria for the statistical analysis were following: (1) Studies comparing LLR and RLR; (2) Studies reporting at least one clinical result or variable; and (3) If any institution reported multiple studies, only the recent and the excellent study was selected. The policies of the exclusion were following: (1) The studies dealing with liver transplantation; (2) Reviews, opinions, comments, letters, and case reports; and (3) The studies were impossible to reproduce. The Cohen kappa statistic was used to quantify assess the agreement among the researchers.
PROSPERO was used for the protocol registration (#CRD42021234405).
The independent authors extracted the following initial data: (1) The name of authors, year, and quality of study; (2) The etiology of the disease; and (3) The period of the evaluations.
The publication bias was assessed by the Newcastle–Ottawa Scale: NOS (http://www.ohri.ca/), as they included observational studies. The NOS consists of domains for the patient selection, comparability of study groups, and outcome assessment. The low risk of bias results in a score of 9 points. We considered studies that scored ≥ 7, 4-6, and < 4 to be high, moderate, and low quality, respectively[14].
RevMan software (version 5.3.; The Cochrane Collaboration) was used for the meta-analysis. For continuous variables, the differences between groups were compared using the inverse-variance method. On the other hand, dichotomous outcomes were compared using the Mantel-Haenszel method. The Egger’s test for publication bias was performed using EZR (version 1.54; https://www.softpedia.com/get/Science-CAD/EZR.shtml)[15].
The χ2 test was used to evaluate heterogeneity, and the Cochran Q and I2 statistics were reported. The I2 value describes the percentage variation between studies in degrees of freedom. Low, moderate, and high heterogeneity were defined based on cut-off values of 25%, 50%, and 75%, respectively[16].
All results were considered significant at P values of < 0.05.
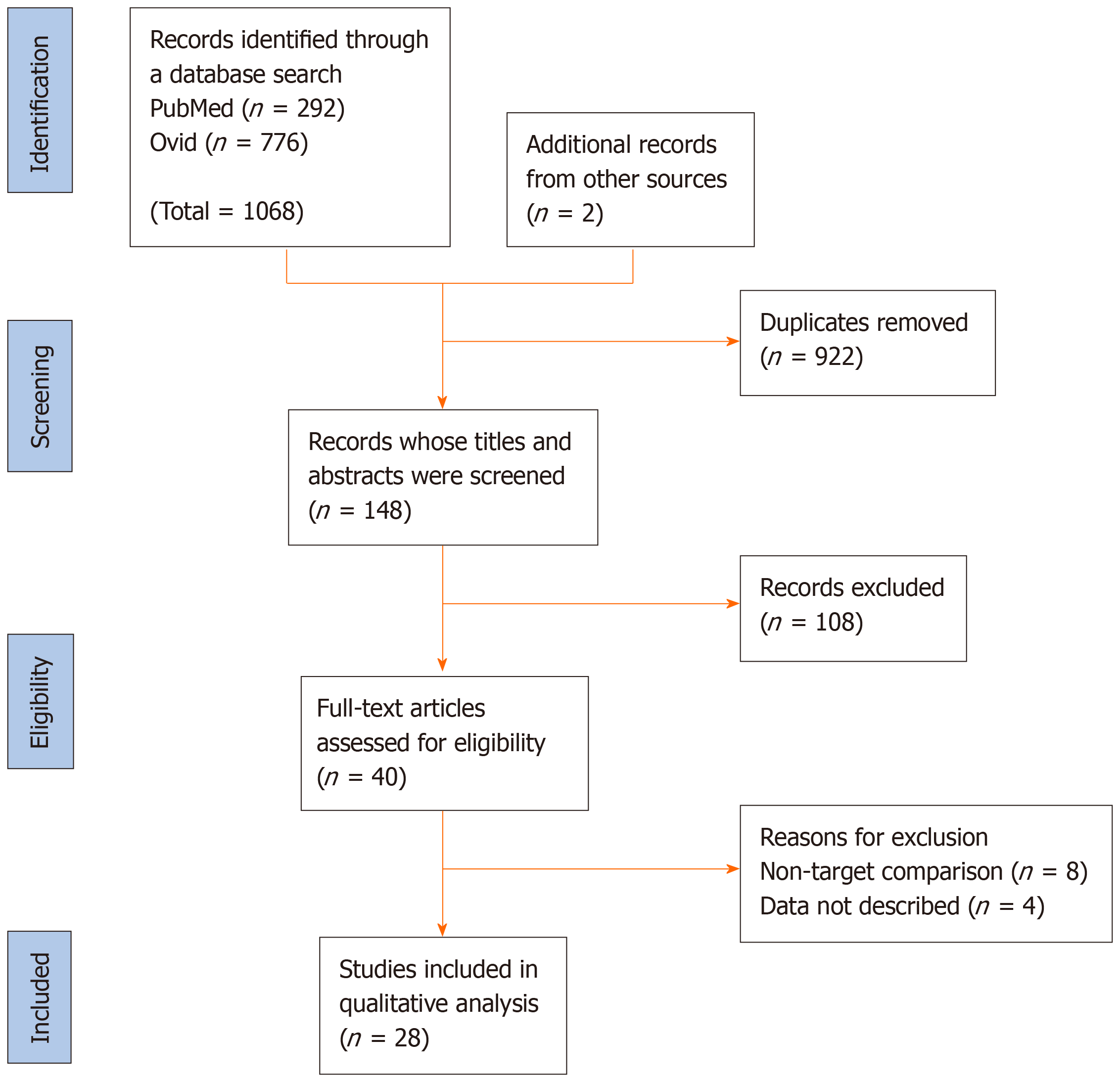
The PRISMA flow diagram for this study is shown in Figure 1. The database search for relevant studies resulted in 1,068 studies being identified. We excluded 922 studies because of duplication, and the titles and abstracts of the remaining 148 studies were screened. As a result, we reviewed 40 full-text articles to evaluate their eligibility further. We excluded 8 studies for which the outcome involved a non-target comparison, and 4 studies for which the data were not available. Finally, we included 28 studies in our meta-analysis.
The data regarding the frequency of each type of liver resection in the selected studies are shown in Tables 1 and 2. Table 1 shows the data for the studies published in 2016 or earlier[9,12,17-30]. Table 2 shows the data for the studies published in 2017 or later[31-42]. No randomized controlled trials (RCT) comparing the clinical outcomes of LLR and RLR were identified. All of the selected publications related to observational studies. The types of liver resection performed did not differ significantly between the early (Table 1) and recent (Table 2) studies.
| Ref. | Laparoscopic liver resection | Robotic liver resection | |||||||||
| Seg | LLS | LH | RH | EH | Seg | LLS | LH | RH | EH | ||
| Berber et al[17], 2010 | Case | 12 | 11 | 6 | 3 | ||||||
| Ji et al[18], 2011 | Case | 9 | 7 | 3 | 1 | 1 | 4 | 6 | 2 | 1 | |
| Lai et al[19], 2011 | Cohort | 6 | 4 | 6 | 3 | ||||||
| Lai et al[20], 2012 | Cohort | 9 | 8 | 12 | 17 | 2 | 1 | ||||
| Packiam et al[21], 2012 | Case | 18 | 11 | ||||||||
| Troisi et al[9], 2013 | Case | 149 | 39 | 16 | 17 | 2 | 38 | 2 | |||
| Spampinato et al[22], 2014 | Case | 9 | 15 | 1 | 8 | 16 | 1 | ||||
| Tranchart et al[23], 2014 | Case | 22 | 5 | 1 | 22 | 5 | 1 | ||||
| Tsung et al[12], 2014 | Case | 72 | 21 | 36 | 21 | ||||||
| Wu et al[24], 2014 | Case | 28 | 31 | 8 | 2 | 8 | 24 | 7 | 12 | 1 | |
| Yu et al[25], 2014 | Case | 6 | 11 | 10 | 3 | ||||||
| Croner et al[26], 2016 | Case | ND | ND | ||||||||
| Kim et al[27], 2016 | Case | 31 | 12 | ||||||||
| Lai et al[28], 2016 | Cohort | 25 | 9 | 1 | 45 | 29 | 6 | 20 | 1 | ||
| Lee et al[29], 2016 | Case | 34 | 30 | 2 | 17 | 39 | 10 | 4 | |||
| Montalti et al[30], 2016 | Case | 72 | 36 | ||||||||
| Ref. | Laparoscopic liver resection | Robotic liver resection | |||||||||
| Seg | LLS | LH | RH | EH | Seg | LLS | LH | RH | EH | ||
| Efanovet al[31], 2017 | Cohort | ND | ND | ||||||||
| Magistriet al[32], 2017 | Case | 24 | 14 | 6 | 2 | ||||||
| Salloumet al[33], 2017 | Case | ND | ND | ||||||||
| Fruscioneet al[34], 2019 | Case | 48 | 22 | 46 | 17 | 20 | 20 | ||||
| Marinoet al[35], 2019 | Cohort | 20 | 14 | ||||||||
| Huet al[36], 2019 | Case | 54 | 58 | ||||||||
| Leeet al[37], 2019 | Case | 7 | 3 | 8 | 5 | ||||||
| Limet al[38], 2019 | Case | ND | ND | ||||||||
| Wanget al[39], 2019 | Case | 29 | 19 | 48 | 44 | ||||||
| Chonget al[40], 2020 | Case | 47 | 40 | 3 | 1 | 34 | 39 | 12 | 6 | ||
| Mejiaet al[41], 2020 | Case | ND | ND | ||||||||
| Rahimliet al[42], 2020 | Case | ND | ND | ||||||||
The data regarding complications of grade ≥ 3 according to the Clavien-Dindo (CD) classification are shown in Figure 2. There was no significant difference in the frequency of such complications between LLR and RLR in the early or recent studies. Scores of I2 in both analyses were 0%, which indicated no heterogeneity. The funnel plots were shown in Supplementary Figure 1.
The data regarding the intraoperative conversion rate are shown in Figure 3. There was no significant difference in the intraoperative conversion rate between LLR and RLR in the early or recent studies. Score of I2 in the early studies was 20% and the one in the recent studies was 44%. The heterogeneities were acceptable in the both analyses. The funnel plots were shown in Supplementary Figure 2.
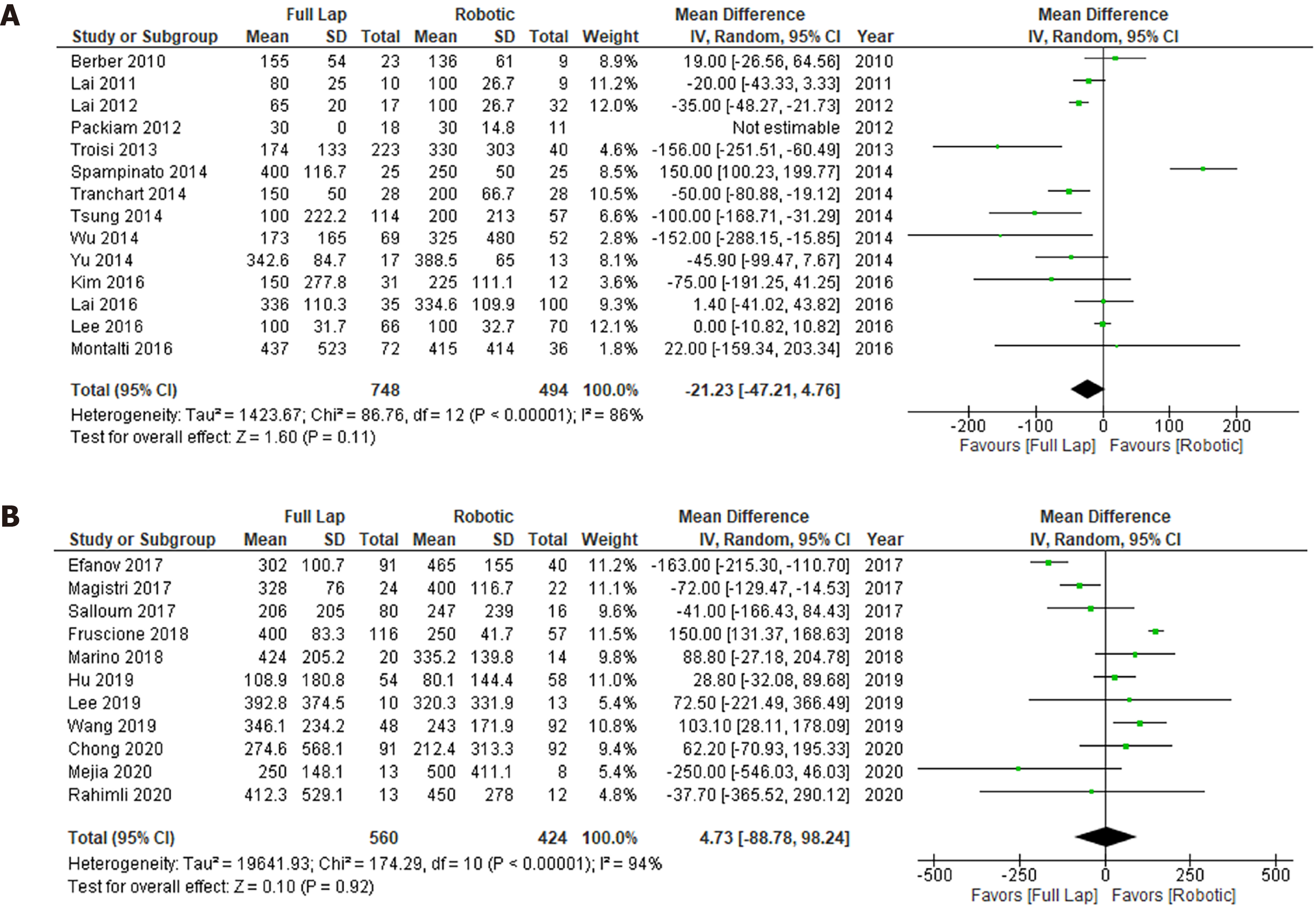
The data regarding intraoperative blood loss are shown in Figure 4. Although LLR tended to cause less intraoperative blood loss than RLR in the early studies, no marked difference in intraoperative blood loss between LLR and RLR was seen in the recent studies. Scores of I2 in the early and recent studies were 88% and 94%, respectively. Severe heterogeneities were observed in both the early and recent analyses. The funnel plots were shown in Supplementary Figure 3.
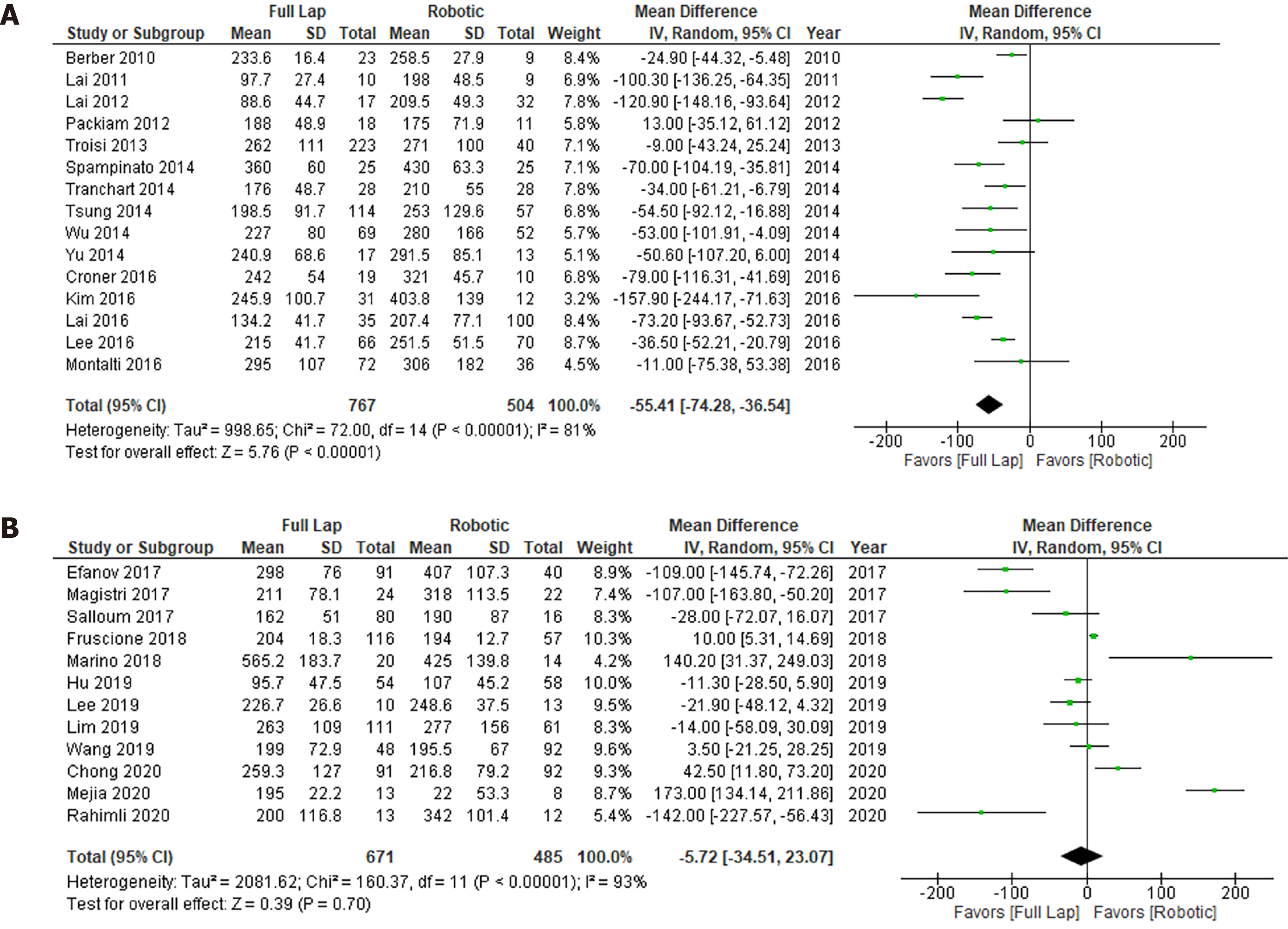
The data regarding the operation time are shown in Figure 5. Although in the early studies the operation time of LLR was significantly shorter than that of RLR (P < 0.0001), there was no significant difference between the operation times of LLR and RLR in the recent studies. Scores of I2 in the early and recent studies were 81% and 93%, respectively. Severe heterogeneities were observed in both the early and recent analyses. The funnel plots were shown in Supplementary Figure 4.
The quality assessment was conducted using the NOS score (Supplementary Table 1 and 2). There was no significant difference in the NOS score between the early and recent studies, although the quality of the studies varied. Summary of the publication bias in each analysis was shown in Supplementary Table 3.
MIS has become the standard approach for liver resection[1,4]. The initial disad
The CD classification is the standard grading system for surgical complications[43]. The definitions of the grades in the CD classification are based on how the complications are managed, e.g., with pharmacological interventions, surgical interventions, or intensive care. These are indirect signs of complications. Furthermore, the grading system is divided into 5 grades plus 2 sub-grades. We did not find any difference in the types of complications encountered according to the CD classification between LLR/RLR or the early/recent period. This may have been because the CD classification is not suitable for identifying differences between clinical studies due to its use of indirect definitions and a relatively large number of grades. Ideally, surgical complications should be analyzed based on direct symptoms of the actual complications and a simple grading system[44].
LLR and RLR exhibited similar intraoperative conversion rates in both periods. The background data for each study varied, as they were all observational studies. The selection criteria for LLR and RLR were also unclear. Therefore, we could not conclude which type of surgery was safer. The maximum intraoperative conversion rate of LLR was about 25% among the recent studies. The maximum intraoperative conversion rate of RLR was about 20% among the early studies, although the mean conversion rate was < 10% in both study periods. In future, these rates could be used as standard clinical goals in order to ensure that surgical quality is maintained.
In the early studies, LLR tended to result in less intraoperative blood loss than RLR, although no marked differences in intraoperative blood loss were seen between LLR and RLR in the recent studies. Several strategies can reduce blood loss during pneumoperitoneum, such as using the head-up position, inducing a high peritoneal pressure, reducing the intratracheal pressure to increase the respiration time, reducing the respiratory volume, using a low central venous pressure, and employing inflow blood control based on the Pringle maneuver[2,45,46]. In addition, it is easier to change the body positions of patients during LLR than during RLR, which could help to control bleeding from veins. Various hemostatic devices are available, such as ultrasonic dissectors, and various hemostatic surgical devices were used for RLR in the recent studies, which may have counteracted the positional disadvantages of RLR. In addition to technical improvements associated with experience, various surgical devices can be used to reduce blood loss during RLR.
In the early studies, the operation time of the RLR was longer than that of the LLR. This is reasonable because it takes time to install robotic towers for robotic procedures. However, the difference in the operation time between the surgical procedures disappeared in the recent studies. It could be that the surgeons became familiar with the robotic procedures, which reduced the time required to set up the robot. Visual support and human-error-canceling functions could also have reduced the operation time[8]. Therefore, the initial disadvantages of RLR have recently been ameliorated.
One advantage of RLR is that it can be used to approach the dorsal segment and caudate lobe of the liver[47,48]. In addition, RLR is superior to LLR for bile duct reconstruction[49]. Therefore, separate tumor location- and surgical procedure-dependent indications need to be developed for RLR and LLR. The differences in the cost and quality-of-life outcomes of RLR and LLR should also be elucidated in the future.
This study had several limitations. First, all of the included studies were observational studies, and no RCT were identified. In addition, the indications for each procedure were not described clearly. The number of subjects recruited for each study varied, as did the quality of each study. In addition, the clinical backgrounds of the studies differed. Although a few studies involved prospective protocols, at present there is no international registration system for such studies.
In conclusion, the initial disadvantages of RLR have been ameliorated. The clinical outcomes of LLR and RLR are comparable. Separate indications for each approach should be developed based on their cost and quality-of-life outcomes. A reliable international registration system for such cases needs to be established.
Robotic liver resection (RLR) has emerged during the last decade. But the clinical outcome of the RLR has been debated.
Clinical outcomes among the laparoscopic liver resection (LLR) and RLR should be compared regarding merit and demerit.
The objective of this study was to conduct a systematic review and meta-analysis comparing the clinical outcomes of LLR and RLR over two 5-year periods.
A systematic literature search was performed using PubMed and Medline, including the Cochrane Library.
A total of 25 articles were included in this meta-analysis after 40 articles had been subjected to full-text evaluations.
The initial disadvantages of RLR, such as its long operation time, have been overcome during the last 5 years. The other clinical outcomes of RLR are comparable to those of LLR.
The cost and quality-of-life outcomes of RLR should be evaluated in future studies to promote its routine clinical use.
| 1. | Meguro M, Mizuguchi T, Kawamoto M, Ota S, Ishii M, Nishidate T, Okita K, Kimura Y, Hirata K. Clinical comparison of laparoscopic and open liver resection after propensity matching selection. Surgery. 2015;158:573-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Mizuguchi T, Kawamoto M, Nakamura Y, Meguro M, Hui TT, Hirata K. New technique of extracorporeal hepatic inflow control for pure laparoscopic liver resection. Surg Laparosc Endosc Percutan Tech. 2015;25:e16-e20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Ogiso S, Hatano E, Nomi T, Uemoto S. Laparoscopic liver resection: Toward a truly minimally invasive approach. World J Gastrointest Endosc. 2015;7:159-161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Mizuguchi T, Kawamoto M, Meguro M, Shibata T, Nakamura Y, Kimura Y, Furuhata T, Sonoda T, Hirata K. Laparoscopic hepatectomy: a systematic review, meta-analysis, and power analysis. Surg Today. 2011;41:39-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Swaid F, Geller DA. Minimally Invasive Primary Liver Cancer Surgery. Surg Oncol Clin N Am. 2019;28:215-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Chua D, Syn N, Koh YX, Goh BKP. Learning curves in minimally invasive hepatectomy: systematic review and meta-regression analysis. Br J Surg. 2021;108:351-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 104] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 7. | Buess GF, Schurr MO, Fischer SC. Robotics and allied technologies in endoscopic surgery. Arch Surg. 2000;135:229-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 36] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Moorthy K, Munz Y, Dosis A, Hernandez J, Martin S, Bello F, Rockall T, Darzi A. Dexterity enhancement with robotic surgery. Surg Endosc. 2004;18:790-795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 182] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 9. | Troisi RI, Patriti A, Montalti R, Casciola L. Robot assistance in liver surgery: a real advantage over a fully laparoscopic approach? Int J Med Robot. 2013;9:160-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 108] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 10. | Giulianotti PC, Bianco FM, Daskalaki D, Gonzalez-Ciccarelli LF, Kim J, Benedetti E. Robotic liver surgery: technical aspects and review of the literature. Hepatobiliary Surg Nutr. 2016;5:311-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 82] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 11. | Zhang L, Yuan Q, Xu Y, Wang W. Comparative clinical outcomes of robot-assisted liver resection vs laparoscopic liver resection: A meta-analysis. PLoS One. 2020;15:e0240593. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 50] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 12. | Tsung A, Geller DA, Sukato DC, Sabbaghian S, Tohme S, Steel J, Marsh W, Reddy SK, Bartlett DL. Robotic vs laparoscopic hepatectomy: a matched comparison. Ann Surg. 2014;259:549-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 262] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 13. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11206] [Cited by in RCA: 11310] [Article Influence: 665.3] [Reference Citation Analysis (0)] |
| 14. | Islam MM, Iqbal U, Walther B, Atique S, Dubey NK, Nguyen PA, Poly TN, Masud JH, Li YJ, Shabbir SA. Benzodiazepine Use and Risk of Dementia in the Elderly Population: A Systematic Review and Meta-Analysis. Neuroepidemiology. 2016;47:181-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 163] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 15. | Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplantation. 2013;48:452-458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9275] [Cited by in RCA: 14478] [Article Influence: 1113.7] [Reference Citation Analysis (0)] |
| 16. | Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39087] [Cited by in RCA: 48538] [Article Influence: 2110.3] [Reference Citation Analysis (4)] |
| 17. | Berber E, Akyildiz HY, Aucejo F, Gunasekaran G, Chalikonda S, Fung J. Robotic vs laparoscopic resection of liver tumours. HPB (Oxford). 2010;12:583-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 144] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 18. | Ji WB, Wang HG, Zhao ZM, Duan WD, Lu F, Dong JH. Robotic-assisted laparoscopic anatomic hepatectomy in China: initial experience. Ann Surg. 2011;253:342-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 144] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 19. | Lai EC, Tang CN, Yang GP, Li MK. Multimodality laparoscopic liver resection for hepatic malignancy--from conventional total laparoscopic approach to robot-assisted laparoscopic approach. Int J Surg. 2011;9:324-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 20. | Lai EC, Tang CN, Li MK. Conventional laparoscopic and robot-assisted laparoscopic liver resection for benign and malignant pathologies: a cohort study. J Robot Surg. 2012;6:295-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Packiam V, Bartlett DL, Tohme S, Reddy S, Marsh JW, Geller DA, Tsung A. Minimally invasive liver resection: robotic vs laparoscopic left lateral sectionectomy. J Gastrointest Surg. 2012;16:2233-2238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 105] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 22. | Spampinato MG, Coratti A, Bianco L, Caniglia F, Laurenzi A, Puleo F, Ettorre GM, Boggi U. Perioperative outcomes of laparoscopic and robot-assisted major hepatectomies: an Italian multi-institutional comparative study. Surg Endosc. 2014;28:2973-2979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 89] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 23. | Tranchart H, Ceribelli C, Ferretti S, Dagher I, Patriti A. Traditional vs robot-assisted full laparoscopic liver resection: a matched-pair comparative study. World J Surg. 2014;38:2904-2909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 64] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 24. | Wu YM, Hu RH, Lai HS, Lee PH. Robotic-assisted minimally invasive liver resection. Asian J Surg. 2014;37:53-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 70] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 25. | Yu YD, Kim KH, Jung DH, Namkoong JM, Yoon SY, Jung SW, Lee SK, Lee SG. Robotic vs laparoscopic liver resection: a comparative study from a single center. Langenbecks Arch Surg. 2014;399:1039-1045. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 81] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 26. | Croner RS, Perrakis A, Hohenberger W, Brunner M. Robotic liver surgery for minor hepatic resections: a comparison with laparoscopic and open standard procedures. Langenbecks Arch Surg. 2016;401:707-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 77] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 27. | Kim JK, Park JS, Han DH, Choi GH, Kim KS, Choi JS, Yoon DS. Robotic vs laparoscopic left lateral sectionectomy of liver. Surg Endosc. 2016;30:4756-4764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 54] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 28. | Lai EC, Tang CN. Long-term Survival Analysis of Robotic Versus Conventional Laparoscopic Hepatectomy for Hepatocellular Carcinoma: A Comparative Study. Surg Laparosc Endosc Percutan Tech. 2016;26:162-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 29. | Lee KF, Cheung YS, Chong CC, Wong J, Fong AK, Lai PB. Laparoscopic and robotic hepatectomy: experience from a single centre. ANZ J Surg. 2016;86:122-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 30. | Montalti R, Scuderi V, Patriti A, Vivarelli M, Troisi RI. Robotic vs laparoscopic resections of posterosuperior segments of the liver: a propensity score-matched comparison. Surg Endosc. 2016;30:1004-1013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 98] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 31. | Efanov M, Alikhanov R, Tsvirkun V, Kazakov I, Melekhina O, Kim P, Vankovich A, Grendal K, Berelavichus S, Khatkov I. Comparative analysis of learning curve in complex robot-assisted and laparoscopic liver resection. HPB (Oxford). 2017;19:818-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 99] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 32. | Magistri P, Tarantino G, Guidetti C, Assirati G, Olivieri T, Ballarin R, Coratti A, Di Benedetto F. Laparoscopic vs robotic surgery for hepatocellular carcinoma: the first 46 consecutive cases. J Surg Res. 2017;217:92-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 49] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 33. | Salloum C, Lim C, Lahat E, Gavara CG, Levesque E, Compagnon P, Azoulay D. Robotic-Assisted Versus Laparoscopic Left Lateral Sectionectomy: Analysis of Surgical Outcomes and Costs by a Propensity Score Matched Cohort Study. World J Surg. 2017;41:516-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 34. | Fruscione M, Pickens R, Baker EH, Cochran A, Khan A, Ocuin L, Iannitti DA, Vrochides D, Martinie JB. Robotic-assisted vs laparoscopic major liver resection: analysis of outcomes from a single center. HPB (Oxford). 2019;21:906-911. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 71] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 35. | Marino MV, Shabat G, Guarrasi D, Gulotta G, Komorowski AL. Comparative Study of the Initial Experience in Performing Robotic and Laparoscopic Right Hepatectomy with Technical Description of the Robotic Technique. Dig Surg. 2019;36:241-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 36. | Hu M, Liu Y, Li C, Wang G, Yin Z, Lau WY, Liu R. Robotic vs laparoscopic liver resection in complex cases of left lateral sectionectomy. Int J Surg. 2019;67:54-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 37. | Lee SJ, Lee JH, Lee YJ, Kim SC, Hwang DW, Song KB, Shin SH, Kwon JW, Park GS, Park YJ, Park KM. The feasibility of robotic left-side hepatectomy with comparison of laparoscopic and open approach: Consecutive series of single surgeon. Int J Med Robot. 2019;15:e1982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 38. | Lim C, Salloum C, Tudisco A, Ricci C, Osseis M, Napoli N, Lahat E, Boggi U, Azoulay D. Short- and Long-term Outcomes after Robotic and Laparoscopic Liver Resection for Malignancies: A Propensity Score-Matched Study. World J Surg. 2019;43:1594-1603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 39. | Wang ZZ, Tang WB, Hu MG, Zhao ZM, Zhao GD, Li CG, Tan XL, Zhang X, Lau WY, Liu R. Robotic vs laparoscopic hemihepatectomy: A comparative study from a single center. J Surg Oncol. 2019;120:646-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 40. | Chong CCN, Lok HT, Fung AKY, Fong AKW, Cheung YS, Wong J, Lee KF, Lai PBS. Robotic vs laparoscopic hepatectomy: application of the difficulty scoring system. Surg Endosc. 2020;34:2000-2006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 57] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 41. | Mejia A, Cheng SS, Vivian E, Shah J, Oduor H, Archarya P. Minimally invasive liver resection in the era of robotics: analysis of 214 cases. Surg Endosc. 2020;34:339-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 42. | Rahimli M, Perrakis A, Schellerer V, Gumbs A, Lorenz E, Franz M, Arend J, Negrini VR, Croner RS. Robotic and laparoscopic liver surgery for colorectal liver metastases: an experience from a German Academic Center. World J Surg Oncol. 2020;18:333. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 43. | Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18532] [Cited by in RCA: 26103] [Article Influence: 1186.5] [Reference Citation Analysis (2)] |
| 44. | Ishii M, Mizuguchi T, Harada K, Ota S, Meguro M, Ueki T, Nishidate T, Okita K, Hirata K. Comprehensive review of post-liver resection surgical complications and a new universal classification and grading system. World J Hepatol. 2014;6:745-751. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 45. | Otsuka Y, Katagiri T, Ishii J, Maeda T, Kubota Y, Tamura A, Tsuchiya M, Kaneko H. Gas embolism in laparoscopic hepatectomy: what is the optimal pneumoperitoneal pressure for laparoscopic major hepatectomy? J Hepatobiliary Pancreat Sci. 2013;20:137-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 72] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 46. | Pan YX, Wang JC, Lu XY, Chen JB, He W, Chen JC, Wang XH, Fu YZ, Xu L, Zhang YJ, Chen MS, Lai RC, Zhou ZG. Intention to control low central venous pressure reduced blood loss during laparoscopic hepatectomy: A double-blind randomized clinical trial. Surgery. 2020;167:933-941. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 47. | Zhao ZM, Yin ZZ, Meng Y, Jiang N, Ma ZG, Pan LC, Tan XL, Chen X, Liu R. Successful robotic radical resection of hepatic echinococcosis located in posterosuperior liver segments. World J Gastroenterol. 2020;26:2831-2838. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 27] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 48. | Vanbrugghe C, Fara R, Camerlo A. Robotic anatomical resection of segment 7 by caudate lobe approach for colorectal metastasis (with video). Surg Oncol. 2021;37:101548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 49. | Giulianotti PC, Sbrana F, Bianco FM, Addeo P. Robot-assisted laparoscopic extended right hepatectomy with biliary reconstruction. J Laparoendosc Adv Surg Tech A. 2010;20:159-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 90] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Corresponding Author's Membership in Professional Societies: The Japanese Society of Gastroenterology.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Wang K S-Editor: Liu M L-Editor: Filipodia P-Editor: Yu HG