Published online Aug 28, 2021. doi: 10.13105/wjma.v9.i4.333
Peer-review started: March 27, 2021
First decision: June 15, 2021
Revised: July 1, 2021
Accepted: September 1, 2021
Article in press: September 1, 2021
Published online: August 28, 2021
Processing time: 159 Days and 20.3 Hours
A series of changes occur in the remaining alveolar process after whole tooth extraction. The basic question is, why do the bony walls (especially the labial/buccal) get resorbed immediately after the tooth is removed? This could be because, with cementum of the concerned tooth and its periodontal ligament, the supporting bundle bone is dependent on the presence of the tooth. This loss can be compensated using numerous techniques, such as socket grafting using various biomaterials to preserve the alveolar bone and buccal grafting with guided tissue regeneration to increase the thickness of buccal bone or placement of implant immediately. However, none of these techniques prevent the modelling of the alveolar bone post-extraction. Few studies have demonstrated that preservation of the roots in the alveolar process maintains the bone volume and facilitates vertical bone growth. A histological study in animals and humans has shown that the retained root shell does not pose any interference in the osseointegration of the implant (if placed simultaneously). Although various names have been proposed to describe the concept of retaining full or part of the root to prevent the resorption of the ridge, socket-shield and pontic-shield are the two most commonly used terms worldwide. The extraction of the whole tooth might be the choice of therapy when socket-shield or pontic-shield is not possible due to anatomical variations, infections, or lack of clinical expertise. Irrespective of the size, when a whole root or a root fragment (is left in situ), it is the dentist’s ethical duty to advise/inform the patient and ensure repeated clinical and radiographic follow-up. The present study aimed to highlight the current status of these techniques, their benefits, and possible complications and address whether the paradigm of the teeth extraction methods should be altered.
Core Tip: The phrase ‘prevention is better than cure’ holds very true when it comes to alveolar ridge resorption. A significant bone is lost within 3 mo after extraction of the whole tooth. Socket/pontic shield techniques can preserve the alveolar bone and prevent a lot of surgical and economic burden to the patient in restoring what could have been saved in a very economical and natural way. Although these procedures are technique sensitive, clinicians must expertise in these techniques, since preserving what can be preserved is not only scientifically desirable but also ethically advisable.
- Citation: Agrawal AA. Fate of root shell after pontic/socket shield techniques, is it better to extract the whole tooth? World J Meta-Anal 2021; 9(4): 333-341
- URL: https://www.wjgnet.com/2308-3840/full/v9/i4/333.htm
- DOI: https://dx.doi.org/10.13105/wjma.v9.i4.333
Subsequent to whole tooth extraction, a series of changes occur in the remaining alveolar process. This may prevent or pose difficulty in implant installation at a prosthetically driven position. Also, there is an increasing demand for functional restoration and its aesthetic aspect. This emphasizes the importance of retaining sufficient alveolar ridge volume to deliver a functionally and aesthetically acceptable implant-supported prosthesis.
The basic question is, why do the bony walls (especially the labial/buccal) get resorbed rapidly after the tooth is removed? The answer is that with the cementum of the concerned tooth and its periodontal ligament (PDL), the supporting bundle bone is dependent on the presence of the tooth. The structure of the buccal bony wall of anterior teeth also has the same structure, and it is also tooth-dependent[1]. Interestingly, the bundle bone has the potential to exist in a thinner dimension compared to the alveolar/basal bone because of the PDL that provides the functional, nutritional, and cellular source existence and maintenance.
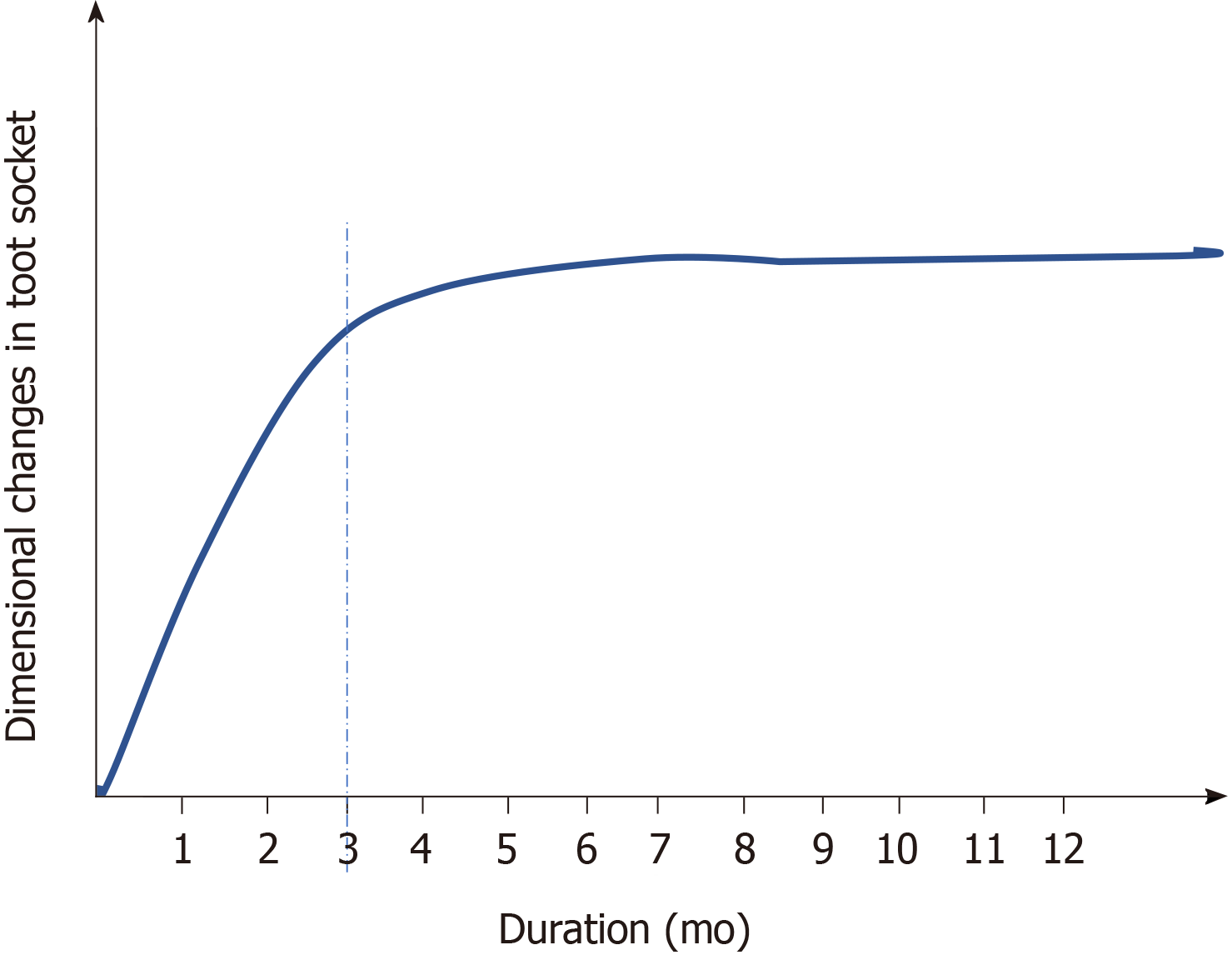
The majority of the dimensional changes that occur as a part of socket healing are primarily observed in the first 3 mo after extraction. However, the reorganization of the alveolar ridge can continue for almost a year[2], indicating a greater degree of bone modelling in the first 3 mo, followed by remodelling (Figure 1). However, the rate and pattern of socket healing could be attributed to the biological differences among individuals, the size of the socket under consideration, the prominence of root in the arch, and the degree of surgical trauma induced during extraction. In addition, the reflection of mucoperiosteal flap/full-thickness flap might lead to bone resorption of the thin buccal bone walls[3-5]. However, various human clinical and animal studies could not conclude that extraction without reflection of full-thickness flap prevents the resorption of alveolar bone/crest. The studies highlighted that the extraction procedure induces significant surgical trauma that exceeds the effect (if any) of full-thickness flap reflection[6-9]. Since there is more bundle bone at the crest of the buccal bone than the lingual, bone loss is pronounced in the buccal wall.
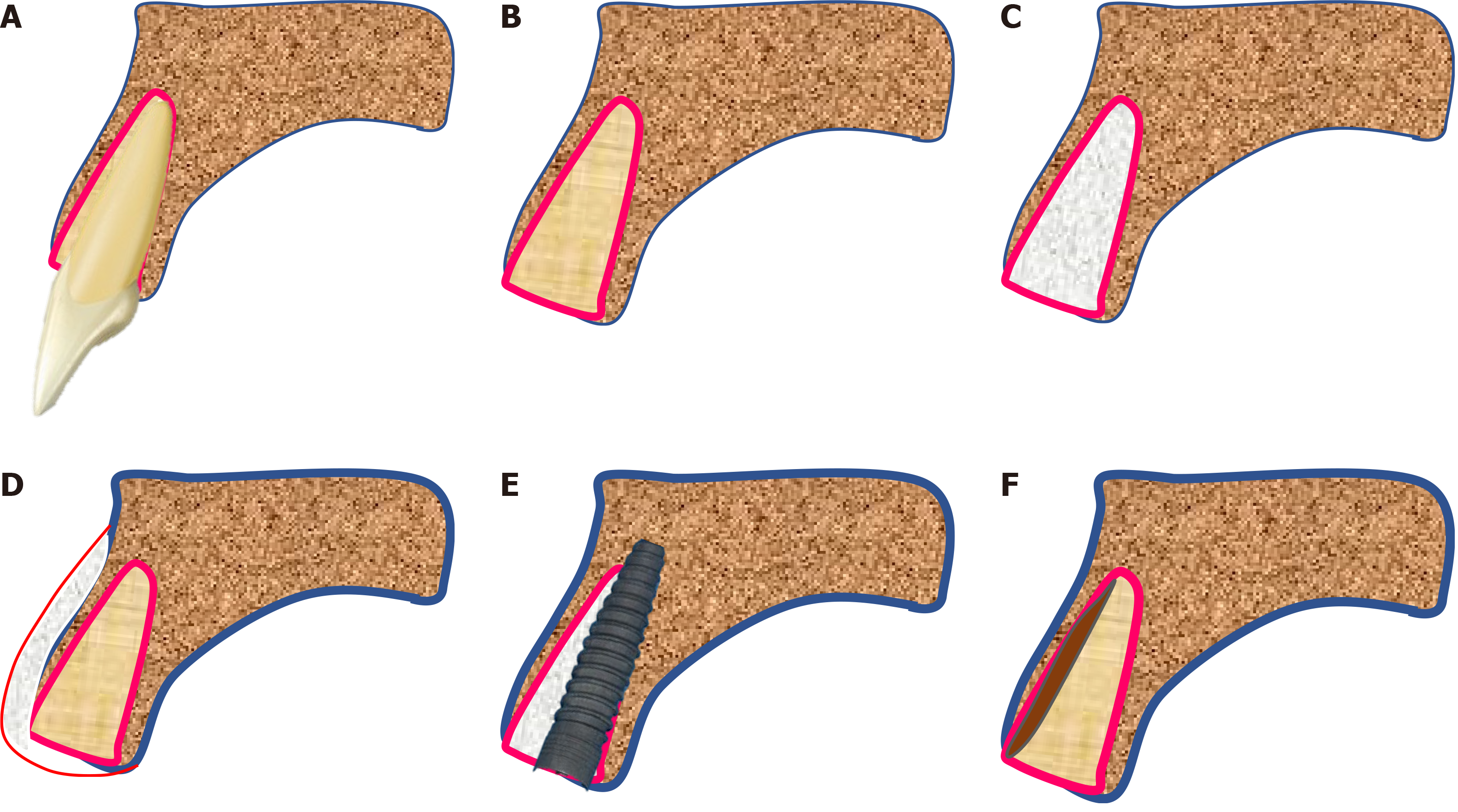
To compensate for this loss, there are numerous techniques described in the literature. Socket grafting (with various biomaterials) to preserve the alveolar bone (Figure 2C), buccal grafting with guided tissue regeneration (GTR) to increase the thickness of the buccal bone (Figure 2D), or placement of immediate implant (Figure 2E). However, none of these techniques truly prevent the modelling of the alveolar bone post-extraction[10-12]. This could be ascribed to significant alterations after tooth extraction due to the loss of PDL and subsequent trauma to the buccal bone. Thus, it could be hypothesized that root retention (vital/pulpless) may avoid tissue alterations that usually occur after whole tooth extraction. Few studies have demonstrated that preservation of the roots in the alveolar process maintains the existing bone volume and helps vertical bone growth[13]. Eventually, instead of retaining the whole root, retaining only a part of the root in contact with the buccal bone plate could be acceptable as only the buccal bone site is at a major risk of resorption (Figure 2F). These methods, termed as ‘socket shield’ or ‘pontic-shield’ techniques, were examined in an investigation in beagle dogs. The histological results of this study revealed that there was no bone modelling observed on the buccal wall, indicating that no resorption occurred[14]. In this study, we described the pros and cons of leaving the root fragment behind intentionally. Although it might be rational to adopt this technique, whether extracting the whole tooth would is beneficial or leaving a part of the root is justified is yet to be investigated.
During extraction, root pieces/root fragments might get retained inadvertently, which is the most common finding on routine radiographs[15]. Partial extraction therapies (PET) is a wide term that encompasses the different types and modifications of complete and partial root fragment retention. It is one of the earliest attempts of PET, wherein the submergence’ technique has been successfully demonstrated for the preservation of alveolar ridge post-extraction, as well as the development of pontic sites. The crown of the tooth is sectioned at the bone crest, and the coronal aspect of the remaining root is hollowed out to mimic the future ovate pontic. Primary soft tissue closure is recommended to encourage healing by primary intention. In a human study, Garver and Fenster[16] demonstrated that the resorption of the alveolar bone is reduced significantly when the root is retained in the alveolar process. Although the concept might be traditional, root submergence is still considered an advantageous method for the development of a pontic-site in clinical practice, wherein the majority of the treatments involve implant prosthesis[17]. Scheuber et al[18] published a technique to preserve the alveolar ridge following posttraumatic ankylosis and external root resorption by retaining the de-crowned root parts. Davarpanah et al[19] conducted a case series study of unconventional implant treatment and demonstrated that immediate implants in direct contact with ankylosed teeth fragments were successfully preserved without any abnormalities over 2 years.
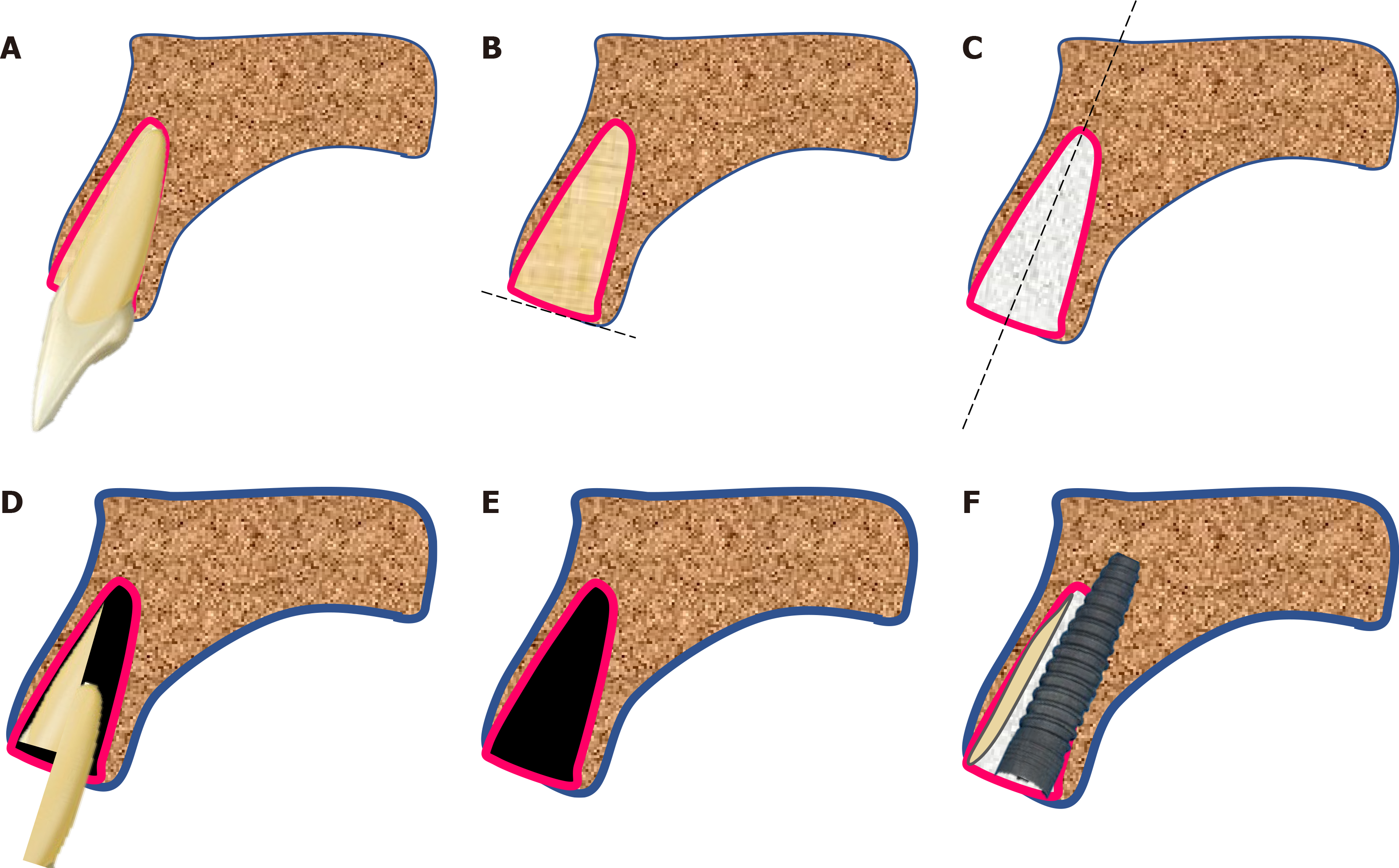
The socket-shield technique introduced by Hürzeler et al[14] involves the facial/buccal root fragment alone to retain the resorption of thin bundle bones. The tooth in concern is sectioned horizontally 1 mm above the bone crest (Figure 3B) and then sectioned longitudinally in facial and palatal halves (Figure 3C). Next, the palatal section was extracted (Figure 3D), and the facial root section is concaved with a long shank dental bur (Figure 3E). It also involves immediate placement of dental implant palatal to the retained root fragment. The jumping space, if any, can be grafted as possible (Figure 3F).
The widespread clinical use of the root-membrane technique started after the outcomes of the first longitudinal study published by Siormpas et al[20]. The study claimed that root membrane is an appropriate term as it focuses on the retention of root fragment in the form of a membrane.
A modification of socket-shield technique is termed the pontic shield technique[21]. The surgical procedure is the same as a socket shield, with the only difference being that an immediate implant is not placed. It facilitates space-filling with maximum bone, and then the implant may or may not be placed. Mitsias et al[22] advocated that root-membrane techniques, such as socket shield and others, could be termed as ‘PDL-mediated ridge preservation for immediate implant placement’. In addition to the preservation of alveolar bone or buccal bone, the proximal socket-shield has been used to preserve the interdental papillae. It is useful when two or more adjacent implants are planned.
The partial extraction therapies, socket-shield or pontic-shield or their various modifications, are technique-sensitive. The procedure is associated with the risk of displacement of the retained root fragment or the buccal lamellar bone. In either of these different techniques, no consensus has been achieved with respect to the height or thickness of the root fragment. Glocker et al[23] advocated keeping the root fragment at the same level of the buccal alveolar ridge, which prevents the risk of fracture of the root fragment. On the other hand, Mitsias et al[22] preferred the root fragment to be at least 1 mm higher than the buccal crest, which would retain more PDL fibers and support more soft tissue at the crest. In an animal study, Tan et al[24] demonstrated that the degree of bone resorption is not affected by the height of the root fragment. However, it was positively correlated when the thickness of the root fragment was between 0.5 mm and 1.5 mm, and the bone resorption may decrease significantly. Extremely thick root fragment is stable but occupies more space leaving less for the implant. On the other hand, an overly reduced shield is unstable. Gluckman et al[25] recommended reducing the thickness of the retained fragment to approximately half its thickness from the root canal to the tooth’s labial limit.
In a 4-mo histological examination study, O’Neal et al[26] submerged 16 endodonti
Gray and Vernino[30] conducted an animal study in baboons to evaluate the effect of unintentional placement of the root form implants into or near retained root fragments. The study found that many implants were placed through the retained roots while others were placed through the PDL of the other root fragments. Histologically they did not find any inflammation at any site. At the locations where the implant was in direct contact with PDL, fibrous encapsulations of the implants were detected, while in some areas, calcified material was deposited on the implant surface.
Buser et al[31] and Hürzeler et al[14] evaluated the effects of placement of endosseous titanium implant fixture in the presence of retained roots in monkeys and Beagle dogs, respectively. Buser et al[31] reported that immediate implant placement over apical portions of the fractured retained roots resulted in cementum apposition between the fractured root and the implant surface. Hürzeler et al[14] modified this idea further and intentionally fractured the roots axially preserving the buccal portion of the root and placed an enamel matrix derivative in the socket before placing an implant. Similar results were reported showing that cementum covered the surface of both the retained root fragment and the implant. Bäumer et al[32] further evaluated the socket-shield using vertically separated root fragments in beagle dogs (without Emdogain). A new bone was found between the dentine layer and the implant surface; however, converse to the previous study, wherein Emdogain was coated on the root fragment, the present study did not find any cementum formation up to 4-mo follow-up period.
This might lead to the speculation that if one root fragment can prevent the resorption of buccal bone, then it would be beneficial to leave the root-membrane-type wall along all the socket walls and place the implant in the centre. Calvo-Guirado et al[33] conducted a histological animal study, wherein 36 implants were inserted in the mandible of 6 American Foxhound dogs using the principle of ‘root-t-belt’, i.e., the crowns were sliced at the bone crest, and implant beds were prepared in the centre of the roots passing 3 mm apically. At the 3-mo histological evaluation, all fixtures were osseointegrated; however, three samples demonstrated inflammatory reaction, and some radicular fragments were detected in the resorption state.
Mitsias et al[34] presented histological evidence for a root-membrane case. The human sample analysis revealed that even after 5 years of post-implant placement, the buccal bone plate was perfectly maintained, and no resorption was evident. The buccal bone was supported and nourished by a healthy, intact PDL. Moreover, the implant showed good osseointegration, with a high amount of compact, mature bone on the surface. At the apical region of the root fragment, where the implant was in direct contact with the root membrane, the authors also noted cementum, which may have migrated from the root to the implant surface[34]. Schwarz et al[35] presented histological evidence of the integration of an implant in the dentin of an unintentionally retained root fragment. The authors discovered that subsequent to trauma during implant site preparation, a layer of reparative dentin was formed on the surface of the retained root fragment that bridged the space between the implant and the root fragment. This type of mineralized integration led them to coin the term ‘dentointegration’, and its pace was equivalent to that of osseointegration seen on the other parts of the implant[35].
Siormpas et al[20] presented one of the largest longitudinal studies on the survival of immediate implants placed adjacent to a root fragment. The data from 46 patients concluded that all implants successfully maintained osseointegration till the end of the follow-up period, giving a cumulative survival rate of 100%. Regarding the fate of the root fragment, the authors found only one patient with the apical root resorption, which was also self-arrested and did not interfere with the osseointegration of the dental implant. In addition, Bäumer et al[32] also raised a genuine clinical question as to what type of tissue would be formed following resorption of the retained root? A previous study demonstrated that the resultant space would be healed by bone fill. Bäumer et al[32] further conducted a study to evaluate whether the socket-shield technique could be successful if the buccal root fragment shows a vertical fracture line. Leaving the fracture line untreated is detrimental to the overall prognosis as it acts like a recess for bacteria, ultimately leading to infection. Therefore, the authors recommended surgical separation of the buccal shield into two halves along the fracture line. At the follow-up visit, the animal histological data showed a higher buccal alveolar crest height with healthy peri-implant soft tissue and no resorption at the apical end of the tooth fragment. The gap between the root fragment and the implant and the vertically drilled space between the two parts of the buccal shield was filled with the bone in the horizontal section[32].
Approximately, 4-wk are required post-extraction to cover the socket with epithelium. It may be assumed that a similar process occurs between the implant and the retained root fragment. Initially, a blood clot is filled between the implant and the buccal root fragment. This clot prevents the epithelium from growing along the internal root surface. Thus, it may seem that the cells from the remaining PDL are capable of colonizing the root surface and regenerating a new periodontal attachment.
In the previous root submergence technique, gingival tissue perforation and cyst formation were documented complications. To prevent perforation, the roots should be excised at a position slightly apical to the bony edge and beveled and smoothened to avoid any sharp edges.
The earliest histological finding showed a failed, plasma-sprayed titanium implant in contact with an undetected residual root presented with hypercementosis and no PDL[36]. The study also hypothesized that the unintentionally retained root might be a putative source of pathogenic bacteria from the PDL or the root canal itself, which compromises the osseointegration of the implant. Thus, it can be the potential cause of retrograde peri-implantitis, a term introduced by McAllister et al[37]. It is characterized by symptomatic periapical lesions with a healthy coronal bone-implant interface that develops within months of implant fixture placement.
In partial extraction therapy cases, where infection of the root fragment/section is coupled with mobility, removing the root membrane is mandatory. The mobility of the root shield, with or without infection, necessitates its removal. If the implant fails to osseointegrate, but the socket-shield is stable, immobile, and free of infection, the implant can be removed, leaving the shield in-situ for healing as a pontic-shield concept. The subsequent re-evaluation could be conducted to deduce whether an implant should be placed palatal to the shield or used as a pontic site.
With additional literature that would be published on the success of socket-shield and pontic-shield techniques in the future, the procedure would be deemed an ideal requirement. Thus, there would be no more whole tooth extraction, and if not indicated, such whole tooth extraction would be deemed as an act of negligence.
Furthermore, simple and sophisticated technological advances would make the procedure easy and predictable. Thus, there is a dire need to develop a predictable and reproducible set of protocols for socket-shield and/or pontic-shield procedures.
The extraction of a tooth, which for long is regarded as a simple and uncomplicated procedure, should hereon be performed with an understanding that significant ridge resorption will follow. Surgical techniques performed later to compensate for the lost bone (guided bone regeneration/GTR/socket grafting/immediate implant) are not completely effective in preventing the alveolar bone resorption. Previous studies have shown that retaining the root fragment (along with its healthy PDL) is the most economical and successful therapy and should be recommended as required. However, the socket-shield/pontic-shield technique is a sensitive procedure, and its success depends on the operating clinician's expertise. The extraction of the whole tooth might be the choice of therapy when socket-shield or pontic-shield is not possible due to anatomical variations, infections, or lack of clinical expertise. Regardless of the size, whenever it is decided to leave a root fragment (or whole root for that matter) in situ (for whatever reasons), it is the dentist’s ethical duty to advise/inform the patient and ensure repeated clinical, radiographic follow-up in the future.
Although socket-shield technique offers promising results, supporting clinical data are limited due to the lack of well-designed prospective randomised controlled studies. Thus, according to the review by Blaschke and Schwass[38], at this stage, it is not clear whether the socket-shield/pontic-shield techniques provide a long-term stable clinical outcome.
Further clinical research studies, preferably prospective randomised controlled trials involving power analysis to determine an adequate cohort size for statistical interpretation, would draw reliable conclusions.
| 1. | Araújo MG, Silva CO, Misawa M, Sukekava F. Alveolar socket healing: what can we learn? Periodontol 2000. 2015;68:122-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 291] [Article Influence: 32.3] [Reference Citation Analysis (0)] |
| 2. | Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003;23:313-323. [PubMed] |
| 3. | Wilderman MN. Repair after a periosteal retention procedure. J Periodontol. 1963;34:487-503. |
| 4. | Wood DL, Hoag PM, Donnenfeld OW, Rosenfeld LD. Alveolar crest reduction following full and partial thickness flaps. J Periodontol. 1972;43:141-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 182] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 5. | Yaffe A, Fine N, Binderman I. Regional accelerated phenomenon in the mandible following mucoperiosteal flap surgery. J Periodontol. 1994;65:79-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 179] [Article Influence: 5.6] [Reference Citation Analysis (1)] |
| 6. | Araújo MG, Lindhe J. Ridge alterations following tooth extraction with and without flap elevation: an experimental study in the dog. Clin Oral Implants Res. 2009;20:545-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 95] [Article Influence: 5.6] [Reference Citation Analysis (2)] |
| 7. | Blanco J, Nuñez V, Aracil L, Muñoz F, Ramos I. Ridge alterations following immediate implant placement in the dog: flap versus flapless surgery. J Clin Periodontol. 2008;35:640-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 108] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 8. | Chen ST, Darby IB, Reynolds EC, Clement JG. Immediate implant placement postextraction without flap elevation. J Periodontol. 2009;80:163-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 119] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 9. | Fickl S, Zuhr O, Wachtel H, Bolz W, Huerzeler M. Tissue alterations after tooth extraction with and without surgical trauma: a volumetric study in the beagle dog. J Clin Periodontol. 2008;35:356-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 175] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 10. | Fickl S, Zuhr O, Wachtel H, Bolz W, Huerzeler MB. Hard tissue alterations after socket preservation: an experimental study in the beagle dog. Clin Oral Implants Res. 2008;19:1111-1118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 85] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 11. | Fickl S, Schneider D, Zuhr O, Hinze M, Ender A, Jung RE, Hürzeler MB. Dimensional changes of the ridge contour after socket preservation and buccal overbuilding: an animal study. J Clin Periodontol. 2009;36:442-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 67] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 12. | Araújo MG, Sukekava F, Wennström JL, Lindhe J. Ridge alterations following implant placement in fresh extraction sockets: an experimental study in the dog. J Clin Periodontol. 2005;32:645-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 506] [Cited by in RCA: 502] [Article Influence: 23.9] [Reference Citation Analysis (0)] |
| 13. | Andersson L, Emami-Kristiansen Z, Högström J. Single-tooth implant treatment in the anterior region of the maxilla for treatment of tooth loss after trauma: a retrospective clinical and interview study. Dent Traumatol. 2003;19:126-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 45] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Hürzeler MB, Zuhr O, Schupbach P, Rebele SF, Emmanouilidis N, Fickl S. The socket-shield technique: a proof-of-principle report. J Clin Periodontol. 2010;37:855-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 178] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 15. | Sumer AP, Sumer M, Güler AU, Biçer I. Panoramic radiographic examination of edentulous mouths. Quintessence Int. 2007;38:e399-e403. [PubMed] |
| 16. | Garver DG, Fenster RK. Vital root retention in humans: a final report. J Prosthet Dent. 1980;43:368-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Salama M, Ishikawa T, Salama H, Funato A, Garber D. Advantages of the root submergence technique for pontic site development in esthetic implant therapy. Int J Periodontics Restorative Dent. 2007;27:521-527. [PubMed] |
| 18. | Scheuber S, Bosshardt D, Brägger U, von Arx T. [Implant therapy following trauma of the anterior teeth – a new method for alveolar ridge preservation after post-traumatic ankylosis and external root resorption]. Schweiz Monatsschr Zahnmed. 2013;123:417-439. [PubMed] |
| 19. | Davarpanah M, Szmukler-Moncler S. Unconventional implant treatment: I. Implant placement in contact with ankylosed root fragments. A series of five case reports. Clin Oral Implants Res. 2009;20:851-856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 20. | Siormpas KD, Mitsias ME, Kontsiotou-Siormpa E, Garber D, Kotsakis GA. Immediate implant placement in the esthetic zone utilizing the "root-membrane" technique: clinical results up to 5 years postloading. Int J Oral Maxillofac Implants. 2014;29:1397-1405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 68] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 21. | Gluckman H, Du Toit J, Salama M. The Pontic-Shield: Partial Extraction Therapy for Ridge Preservation and Pontic Site Development. Int J Periodontics Restorative Dent. 2016;36:417-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 22. | Mitsias ME, Siormpas KD, Kontsiotou-Siormpa E, Prasad H, Garber D, Kotsakis GA. A Step-by-Step Description of PDL-Mediated Ridge Preservation for Immediate Implant Rehabilitation in the Esthetic Region. Int J Periodontics Restorative Dent. 2015;35:835-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 23. | Glocker M, Attin T, Schmidlin PR. Ridge preservation with modified “socket-shield” technique: a methodological case series. Dent J. 2014;2:11-21. [RCA] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 24. | Tan Z, Kang J, Liu W, Wang H. The effect of the heights and thicknesses of the remaining root segments on buccal bone resorption in the socket-shield technique: An experimental study in dogs. Clin Implant Dent Relat Res. 2018;20:352-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 25. | Gluckman H, Salama M, Du Toit J. Partial Extraction Therapies (PET) Part 2: Procedures and Technical Aspects. Int J Periodontics Restorative Dent. 2017;37:377-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 26. | O'Neal RB, Gound T, Levin MP, del Rio CE. Submergence of roots for alveolar bone preservation. I. Endodontically treated roots. Oral Surg Oral Med Oral Pathol. 1978;45:803-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 27. | Guyer SE. Selectively retained vital roots for partial support of overdentures: a patient report. J Prosthet Dent. 1975;33:258-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 32] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 28. | Plata RL, Kelln EE, Linda L. Intentional retention of vital submerged roots in dogs. Oral Surg Oral Med Oral Pathol. 1976;42:100-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 54] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 29. | Johnson DL, Kelly JF, Flinton RJ, Cornell MT. Histologic evaluation of vital root retention. J Oral Surg. 1974;32:829-833. [PubMed] |
| 30. | Gray JL, Vernino AR. The interface between retained roots and dental implants: a histologic study in baboons. J Periodontol. 2004;75:1102-1106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 31. | Buser D, Warrer K, Karring T, Stich H. Titanium implants with a true periodontal ligament: an alternative to osseointegrated implants? Int J Oral Maxillofac Implants. 1990;5:113-116. [PubMed] |
| 32. | Bäumer D, Zuhr O, Rebele S, Schneider D, Schupbach P, Hürzeler M. The socket-shield technique: first histological, clinical, and volumetrical observations after separation of the buccal tooth segment – a pilot study. Clin Implant Dent Relat Res. 2015;17:71-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 33. | Calvo-Guirado JL, Troiano M, López-López PJ, Ramírez-Fernandez MP, de Val JEMS, Marin JMG, Gehrke SA. Different configuration of socket shield technique in peri-implant bone preservation: An experimental study in dog mandible. Ann Anat. 2016;208:109-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 34. | Mitsias ME, Siormpas KD, Kotsakis GA, Ganz SD, Mangano C, Iezzi G. The Root Membrane Technique: Human Histologic Evidence after Five Years of Function. Biomed Res Int. 2017;2017:7269467. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 35. | Schwarz F, Mihatovic I, Golubovic V, Becker J. Dentointegration of a titanium implant: a case report. Oral Maxillofac Surg. 2013;17:235-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 36. | Guarnieri R, Giardino L, Crespi R, Romagnoli R. Cementum formation around a titanium implant: a case report. Int J Oral Maxillofac Implants. 2002;17:729-732. [PubMed] |
| 37. | McAllister BS, Masters D, Meffert RM. Treatment of implants demonstrating periapical radiolucencies. Pract Periodontics Aesthet Dent. 1992;4:37-41. [PubMed] |
| 38. | Blaschke C, Schwass DR. The socket-shield technique: a critical literature review. Int J Implant Dent. 2020;6:52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Corresponding Author's Membership in Professional Societies: Indian Dental Association; Indian Society of Periodontology; Indian Society of Oral Implantologist; Society of Oral Laser Applications; Indian Society of Clinical Research
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Arisan V, Pan J S-Editor: Liu M L-Editor: A P-Editor: Li JH