Published online Feb 28, 2021. doi: 10.13105/wjma.v9.i1.64
Peer-review started: January 20, 2021
First decision: February 14, 2021
Revised: February 16, 2021
Accepted: February 25, 2021
Article in press: February 25, 2021
Published online: February 28, 2021
Processing time: 41 Days and 5.2 Hours
The novel coronavirus severe acute respiratory syndrome coronavirus 2 is associated with a severe disease known as coronavirus disease 2019 (COVID-19). A small percentage of patients with COVID-19 will require intensive care and possibly mechanical ventilation. The mortality of intensive care interventions in patients with COVID-19 remains unclear.
To identify mortality rate of COVID-19 patients receiving different interventions in the critical care unit.
We searched OVID Medline, SCOPUS, MedRxIv, preprints.org, and Centers for Disease Control databases from November 2019 to April 10, 2020 for articles on COVID-19. Teams of 2 independent reviewers reviewed titles and abstract for studies that reported mortality of human adults with COVID-19 and exposure to a critical care intervention [Intensive care admission, mechanical ventilation, acute hemodialysis, extracorporeal membrane oxygenation, or cardiopulmonary resuscitation (CPR)]. We used a descriptive analysis and unweighted averages of mortality across studies.
Our search identified 6973 articles and 20 met inclusion: 17 for intensive care, 13 for mechanical ventilation, 5 for hemodialysis, 2 for extracorporeal membrane oxygenation, and 1 for CPR. Mortality associated with intensive care admission ranged from 9%-83%, with overall mortality 32.5% (95%CI: 32.4%-32.6%). Mortality associated with intubation from 16.7%-100% with overall mortality 64.0% (95%CI: 62.4%-65.5%). In patients requiring hemodialysis, mortality ranged from 0%-100%, with average mortality 75.3% (95%CI: 72.6%-77.4%).
Patients with COVID-19 requiring intensive care have high mortality rates. Authorities can use this data to establish pharmacoeconomic studies to make decisions about allocation of scarce resources if necessary.
Core Tip: This systematic review identifies the mortality associated with critical care interventions in patients with novel coronavirus disease 2019. These include intensive care admission, mechanical ventilation, acute hemodialysis, extracorporeal membrane oxygenation, or cardiopulmonary resuscitation. Average mortality for intensive care admission was 32.5%. While mortality is high, this is lower than initially described in early reports of the pandemic. Physicians can hopefully use this data to inform decisions about goals of care or, if necessary, allocation of scarce resources.
- Citation: Davis J, Leff R, Patel A, Venkatesan S. Mortality of critical care interventions in the COVID-19: A systematic review. World J Meta-Anal 2021; 9(1): 64-73
- URL: https://www.wjgnet.com/2308-3840/full/v9/i1/64.htm
- DOI: https://dx.doi.org/10.13105/wjma.v9.i1.64
The novel coronavirus disease 2019 (COVID-19) has caused an international pandemic. The pandemic nature of this virus is largely attributed to its virulence and high mortality. Initial reports had mortality as high as 2% in China[1]; 4% in Wuhan, China (the site of initial outbreak)[2]; and 6% in Italy. Later data with widespread testing placed case fatality rate estimates closer to 1%[3]. Nonetheless, another major issue in the pandemic nature of this virus is its ability to overwhelm healthcare systems, particularly the critical care needs of healthcare systems[4]. This includes intensive care beds, ventilators, and dialysis units and was particularly evident in “hot spot” areas, for example Lombardy, Italy and New York City, New York early in the pandemic and many other areas since.
Patients in critical care have mortality rates as high as 50%[5], and patients who require mechanical ventilation have mortality as high as 80%[6]. This is higher than typical patients with viral pneumonia or acute respiratory distress syndrome, which has mortality closer to 35%-45%[7]. Mortality with COVID-19 is much higher in the elderly[3] and those with comorbid conditions, hypertension, diabetes, obesity, and heart disease[8,9]. However, there have been young cases, without any preexisting medical conditions, who required mechanical ventilation and died[10]. Further, patients admitted to intensive care have markedly long lengths of stay in the hospital, on the order of weeks to months[11].
This overwhelming burden on healthcare systems has led to unprecedented discussions about rationing of care[4] and universal Do Not Resuscitate orders[12-14]. These discussions arise in order to preserve precious healthcare resources in overburdened systems as well as to protect healthcare workers from increased exposure to potentially aerosolizing procedures like cardiopulmonary resuscitation, intubation, or bag ventilation. If interventions were universally futile, the decision to not perform them might be easier.
Nonetheless, a small percentage of patients do survive intensive care admission and mechanical ventilation. There are even case reports of patients surviving extracorporeal membrane oxygenation (ECMO)[15-17] and cardiopulmonary resuscitation (CPR)[18]. Thus, these interventions, when implemented in the correct patient population, can save lives.
In order to help inform decisions and discussions about critical care interventions in patients with COVID-19, the authors sought to perform a systematic review of the mortality rate of COVID-19 patients receiving different interventions in the critical care unit.
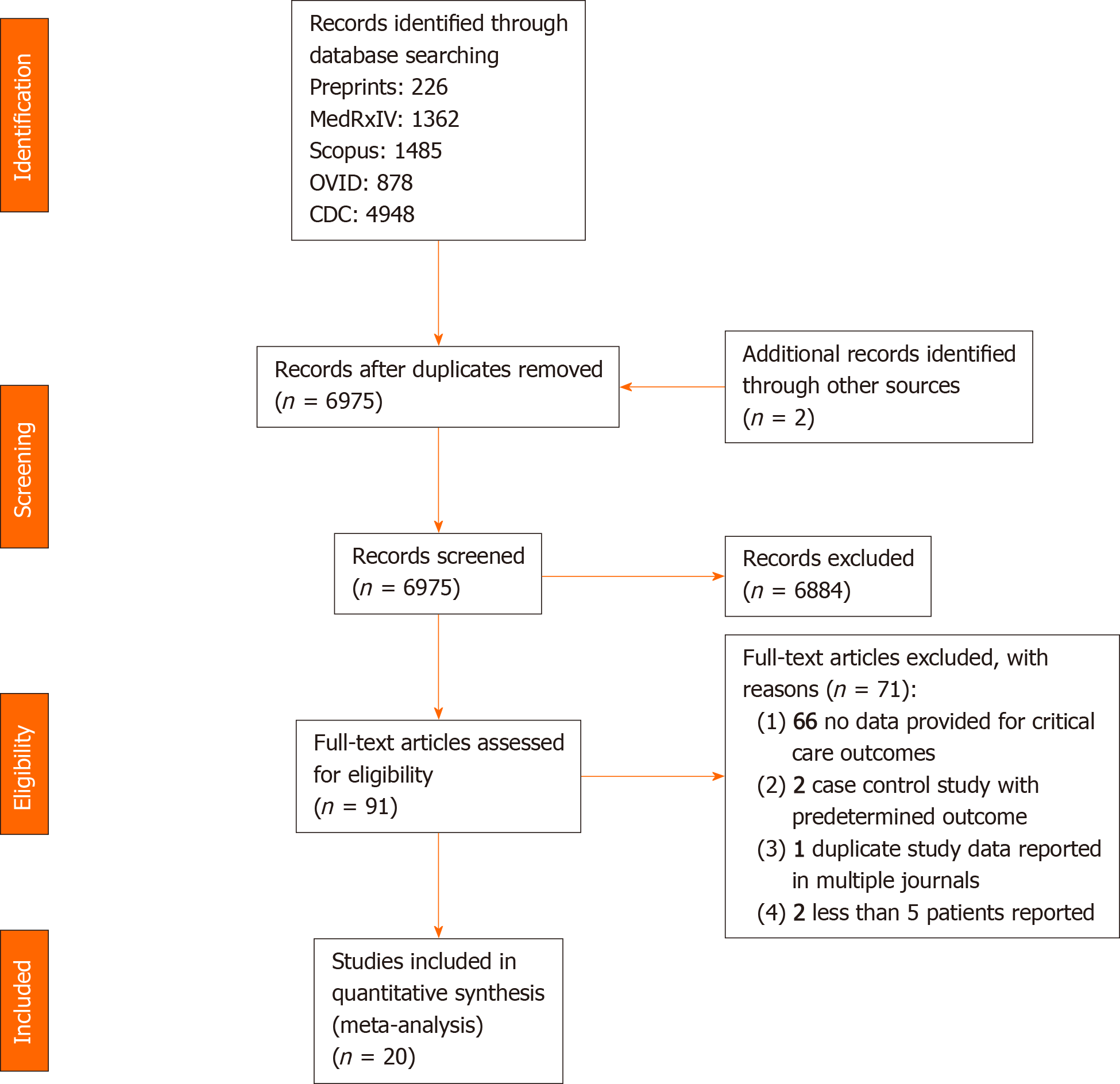
This study had no human subjects and was, therefore, exempt from review by th Institutional Review Board Review. This study was conducted in accordance with Preferred Reporting in Systematic Review and Meta-Analysis Guidelines (PRISMA)[19,20]. The PRISMA Checklist is available in Supplement and the research protocol is available from the authors upon request.
We searched OVID Medline, SCOPUS, MedRxIv, preprints.org, and Centers for Disease Control (CDC) databases from November 2019 to April 10, 2020. The search used keyword terms for “COVID-19”, “SARS”, and “coronavirus”. The CDC database was already compiled and was only filtered for English articles. An example search strategy is available in Supplementary material. We also reviewed citations from included articles, review articles, and suggestions from select content experts to find relevant articles that may have been missed. Titles and abstracts from these search methods were screened independently by 3 trained reviewers (Leff R, Patel A, Venkatesan S). If any reviewer thought an article was potentially relevant, a full text copy of the article was ordered and again reviewed for inclusion by these 3 authors. Inclusion criteria were studies that evaluated human adult patients with COVID-19 and exposure to a critical care intervention, defined as either (1) intensive care admission; (2) endotracheal intubation or mechanical ventilation; (3) acute hemodialysis or renal replacement; (4) ECMO; or (5) CPR. Exclusion criteria included opinions, abstracts, non-English papers, studies on children, studies with < 5 participants, or studies with not enough data to address the research question. We did plan to contact authors for updated data if data was incomplete. All authors independently identified articles for exclusion and any discrepancies were resolved with a consensus meeting among all 4 authors.
After title and abstract selection, a standardized abstraction form was developed by all of the authors. Two of three authors (Leff R, Patel A, Venkatesan S) abstracted data from the studies and compared their results for discrepancies. These were resolved by consensus among all authors. Data included author, publication year, population, setting, intervention, mortality, and other outcomes.
Data were tracked in Microsoft Excel® (Seattle, WA, United States). Inter-rater reliability was assessed using accuracy and Cohen’s kappa. We used the Newcastle-Ottawa Scale to assess risk of bias in the studies[21]. Given the observational nature of these studies without intervention, heterogeneity was not formally assessed. It is assumed to be high. Where applicable, simple meta-analysis was performed using raw, unweighted percentages.
We identified 6973 articles in our search and 20 met inclusion criteria[7,18,22-39] [17 for Intensive care unit (ICU) care[7,22-37], 13 for mechanical ventilation[7,23,24,29-32,34-39], 5 for hemodialysis[24,29,33,36,37], 2 for ECMO[30,36], and 1 for CPR[19], Figure 1]. Details of each study are presented in Table 1. We attempted to reach all authors for updated data and received responses from one author[31]. We also found an updated publication of the report from International Care National Audit and Research Centre (ICNARC) and used the May 1st version of this report[29]. All of the studies were published in 2020, with 15 from Asia[18,23-25,27,28,30-38], 2 from Europe[26,29], 2 from the United States[7,22], and one study which included multiple regions[39]. The ICNARC data was the largest reported cohort and greatly overwhelmed other studies’ sample size. Given this and that overall heterogeneity was subjectively high and there was a low number of studies, meta-analysis was not performed for any intervention other than ICU admission or intubation/mechanical ventilation. Quality scoring revealed generally moderate quality observational studies (Table 1). The accuracy among two selectors was 81%, and interrater reliability for selection was moderate at κ = 0.63 (95%CI: 0.39-0.87).
| Ref. | Data available | Newcastle-Ottawa quality scale | ||||
| Intensive care | Mechanical ventilation | Hemodialysis | ECMO | CPR | ||
| Bhatraju et al[6] | X | X | 4 | |||
| Shao et al[18] | X | 6 | ||||
| Arentz et al[22] | X | 4 | ||||
| Cai et al[23] | X | X | 6 | |||
| Cao et al[24] | X | X | X | 6 | ||
| Chen et al[25] | X | 5 | ||||
| Grasselli et al[26] | X | 5 | ||||
| Han et al[27] | X | 7 | ||||
| Huang et al[28] | X | 7 | ||||
| Intensive Care National Audit and Research Centre[29] | X | X | X | 5 | ||
| Li et al[30] | X | X | X | 4 | ||
| Ling et al[31] | X | X | 6 | |||
| Wang et al[32] | X | X | 7 | |||
| Wang et al[33] | X | X | 7 | |||
| Wang et al[34] | X | X | 6 | |||
| Wu et al[35] | X | X | 6 | |||
| Yang et al[36] | X | X | X | X | 7 | |
| Zhou et al[37] | X | X | X | 7 | ||
| Deng et al[38] | X | 6 | ||||
| Grein et al[39] | X | 5 | ||||
The 17 studies on mortality in COVID-19 patients requiring ICU admission included 9828 patients[7,22-37]. Mortality associated with ICU admission ranged from 9%[25] to 83%[36], with overall mortality of 32.5% (3198/9828, 95%CI: 32.4%-32.6%). However, it is important to note that several studies still had a significant number of patients in the hospital or ICU or did not report long term outcomes. Of studies that reported discharge to home, 242/401 (60.3%. 95%CI: 55.5%-65.1%) patients are clearly reported to be discharged home (Table 2). As mentioned, the ICNARC data is the largest sample and showed a mortality rate of 33% and contributed 7542 of the 9828 patients. The ICNARC sample only reports patients discharged from critical care (2642/7542, 35.0%, 95%CI: 33.9%-36.1%), and not long-term disposition to home. The mortality was similar when excluding ICNARC data (701/2286, 30.7%, 95%CI: 28.8%-32.6%).
| Ref. | Died | Sent home | Total patients | Mortality |
| Bhatraju et al[6] | 12 | 5 | 24 | 50.0% |
| Arentz et al[22] | 11 | 21 | 52.4% | |
| Cai et al[23] | 3 | 30 | 10.0% | |
| Cao et al[24] | 6 | 12 | 18 | 33.3% |
| Chen et al[25] | 2 | 22 | 9.1% | |
| Grasselli et al[26] | 405 | 1581 | 25.6% | |
| Han et al[27] | 3 | 12 | 15 | 20.0% |
| Huang et al[28] | 5 | 7 | 13 | 38.5% |
| Intensive Care National Audit and Research Centre[29] | 2497 | 7542 | 33.1% | |
| Li et al[30] | 4 | 8 | 50.0% | |
| Ling et al[31] | 1 | 1 | 8 | 12.5% |
| Wang et al[32] | 6 | 9 | 36 | 16.7% |
| Wang et al[33] | 7 | 11 | 63.6% | |
| Wang et al[34] | 133 | 185 | 344 | 38.7% |
| Wu et al[35] | 44 | 53 | 83.0% | |
| Yang et al[36] | 20 | 52 | 38.5% | |
| Zhou et al[37] | 39 | 11 | 50 | 78.0% |
| Total | 3198 | 242 | 9828 | 32.5% (average) |
The 13 studies on mortality in COVID-19 patients requiring mechanical ventilation included 3865 patients[7,23,24,29-32,34-39]. The mortality ranged from 16.7%[31] to 100%[38] with a mean of 64.1% (2422/3787, 95%CI: 62.4%-65.5%) (Table 3). Many patients remain intubated or in the ICU. Of studies reporting it, there were 14% (32/322, 95%CI: 10.6%-18.2%) of intubated patients who were eventually discharged to home. Again, the ICNARC data contributed 3,508 of these patients with a mortality of 62.0% (2175/3508, 95%CI: 63.6%-60.4%). The ICNARC data for this category only reports patient with an outcome of discharged from the ICU or death. Patient still receiving mechanical ventilation and long-term dispositions are not reported in this data. When not including the ICNARC data, the average mortality was 77.1% (262/340, 95%CI: 72.6%-81.6%).
| Ref. | Died | Total patients | Mortality |
| Bhatraju et al[6] | 9 | 18 | 50.0% |
| Cai et al[23] | 3 | 30 | 10.0% |
| Cao et al[24] | 12 | 14 | 33.3% |
| Intensive Care National Audit and Research Centre[29] | 2175 | 3508 | 33.1% |
| Li et al[30] | 4 | 8 | 50.0% |
| Ling et al[31] | 1 | 6 | 12.5% |
| Wang et al[32] | 6 | 17 | 35.2% |
| Wang et al[34] | 97 | 10 | 38.7% |
| Wu et al[35] | 44 | 67 | 83.0% |
| Yang et al[36] | 19 | 22 | 38.5% |
| Zhou et al[37] | 31 | 32 | 78.0% |
| Deng et al[38] | 21 | 21 | 100.00% |
| Grein et al[39] | 6 | 34 | 17.6% |
| Total | 2428 | 3787 | 64.1% (average) |
There were 5 studies of 1203 patients that reported outcomes of patient who received acute hemodialysis, which included continuous renal replacement therapy or intermittent hemodialysis[24,29,33,36,37] (Table 4). Mortality ranged from 0%[33] to 100%[37], with the average mortality being 75.3% (898/1193, 95%CI: 72.6%-77.4%), with ICNARC contributing 1163 of these patients and the ICNARC mortality being 75% (870/1163, 95%CI: 72.5%-77.5%)[29]. Mortality of studies not including ICNARC data was 80% (32/40, 95%CI: 92.4%-67.3%). Of the remaining 8 patients not in the ICNARC data, 7 were discharged from the hospital and one was discharged from the ICU.
Only 2 studies met our criteria for reporting more than 5 patients who received ECMO[30,36]. In these studies, the mortality was 50% (4/8)[30] in one and 83% (5/6)[36] in the other. Li et al[30] report of the remaining 4 patients, 3 were taken off ECMO and one is still on ECMO, and Yang et al[36] report their surviving patient to be discharged from the hospital. Several other studies included in our analysis report 100% mortality for small numbers of patients on ECMO: 1[35], 2[38], and 3[37] patients. Cao et al[24] report that of their 3 patients, 1 died and 2 were discharged from the hospital, and Grein et al[39] report that of their 4 patients, 1 was discharged home and 3 remain on ECMO.
Only 1 study reported of significant sample size on cardiac arrest[18]. In this study of 136 patients who received CPR in the hospital, ROSC was achieved in 18 (13.2%, 95%CI: 7.5%-18.9%) patients, of which 4 (2.9%, 95%CI: 0%-5.7%) patients were still alive at 30 days, and 1 was reported to have a good neurologic outcome (0.7%, 95%CI: 0%-2.1%) with a cerebral performance category score of 1 or 2.
Our study is the first systematic review on outcomes in critical care patients with COVID-19. We showed an average ICU mortality of 33% and mortality of intubated patients of 64%. The mortality rates we found are less than those initially reported out of China[2,36], but higher than similar reports of patients with acute respiratory distress syndrome or viral pneumonia[8]. Other, more intensive interventions (Hemodialysis, ECMO, and CPR) were associated with increasing mortality.
Given the nature and spread of COVID-19, healthcare resources have been overwhelmed. This has led some institutions to discuss appropriate allocation of these scarce resources (i.e., ventilators, ICU beds, healthcare personnel). Many long-term care facilities and hospitals have placed an appropriate emphasis on advanced directives among those patients most at risk for severe disease. Our data should help physicians quantify outcomes associated with various critical care interventions.
Some hospitals have controversially instituted universal “Do Not Resuscitate” orders in order to conserve resources and protect healthcare resources[12-14]. We only identified one study on a large data set of patients receiving CPR. This showed only 1/136 patients (0.7%) who required CPR survived neurologically intact. This supports the concept that CPR is largely, though not universally futile. Given that there is also risk to healthcare workers, institutions should proactively work to identify which patients with COVID-19 would benefit from CPR. For example, ventilated patients who suffer hypoxic arrest probably have little to gain from CPR, unless it is a bridge to some other form of oxygenation like ECMO.
Of course, decisions regarding patient care and limitations must also be personalized to individual patients. Unfortunately, given the summary nature of our data, it cannot be used to express a patient’s individual risk. This will be based on many factors, including age and comorbidities which are not included in our analysis. Mortality alone is also not the only prognostic outcome of interest to many patients. Further, beyond prognosis, decisions regarding care limitations must also consider a patient’s functional status and preferences and values.
One of the most important limitations of our analysis is that many patients remained in the ICU at the time of this analysis. This undoubtedly leads to incomplete estimates of mortality. Of the studies that reported data, we attempted to include data on patients discharged from the hospital, as well. We also attempted to reach authors for updated data in this regard, but only received a response from one author. There have also been reported concerns regarding duplicate publications of data, which could lead to overrepresentation of some samples[40]. Some analyses are influenced by a few large data sets (i.e., ICNARC), but it is reassuring that mortality estimated remain nearly the same when not including this data. Finally, the data on COVID-19 continues to rapidly evolve, and treatment paradigms continue to change. Therefore, it is possible that mortality may improve as treatments improve.
In conclusion, COVID-19 is a novel disease process, which is associated with high mortality in those patients requiring critical care. The intensity of intervention seems to be associated with increasing mortality. Clinicians should consider this data, along with patient-specific factors, when deciding which intensive care interventions to initiate. Complete data considering disposition of all patients will improve our understanding of the prognosis of this new disease process.
The novel coronavirus disease 2019 (COVID-19) has ravaged humans across the globe. Mortality is high, especially in the most critically ill patients. Due to the pandemic nature of the virus, some locations have been forced to ration resources.
Critical care is, by nature, highly resource intensive. With limited resources and an overwhelming number of critically ill patients in some communities, discussions about rationing limited resources have begun. Fundamental to these discussions is understanding the probability of survival of the most intensive interventions.
Our objective was to identify, via systematic review, the mortality rate of COVID-19 patients receiving different interventions in the critical care unit, namely intensive care admission, mechanical ventilation, acute hemodialysis, extracorporeal membrane oxygenation, or cardiopulmonary resuscitation.
We conducted a systematic review of several databases using accepted systematic review methods to identify the mortality rate of COVID-19 patients receiving intensive care admission, mechanical ventilation, acute hemodialysis, extracorporeal membrane oxygenation (ECMO), or cardiopulmonary resuscitation (CPR). Studies included were observational.
Our search identified 20 studies overall. Mortality associated with intensive care admission averaged 32.5%. Mortality associated with intubation averaged 64.0%. In patients requiring hemodialysis, mortality averaged 75.3%. There were limited studies on ECMO and CPR. The one study on CPR showed only 0.7% (1/136) had a good neurologic outcome.
Mortality among COVID-19 patients requiring intensive care is high, though not as high as initially reported. This information can be used to guide goals of care of individual patients and system level discussion about rationing scarce resources when locales are overwhelmed.
Critical care does have a high, but certainly not universal, mortality rate. Further research should identify individual risk factors for poor outcome among patients requiring critical care. CPR, though, appears to have low chance of survival. The decision to perform CPR on critically ill patients should be very carefully considered.
| 1. | Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239-1242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11409] [Cited by in RCA: 11617] [Article Influence: 1936.2] [Reference Citation Analysis (2)] |
| 2. | Mizumoto K, Chowell G. Estimating Risk for Death from Coronavirus Disease, China, January-February 2020. Emerg Infect Dis. 2020;26:1251-1256. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 127] [Cited by in RCA: 123] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 3. | Verity R, Okell LC, Dorigatti I, Winskill P, Whittaker C, Imai N, Cuomo-Dannenburg G, Thompson H, Walker PGT, Fu H, Dighe A, Griffin JT, Baguelin M, Bhatia S, Boonyasiri A, Cori A, Cucunubá Z, FitzJohn R, Gaythorpe K, Green W, Hamlet A, Hinsley W, Laydon D, Nedjati-Gilani G, Riley S, van Elsland S, Volz E, Wang H, Wang Y, Xi X, Donnelly CA, Ghani AC, Ferguson NM. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020;20:669-677. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2689] [Cited by in RCA: 2248] [Article Influence: 374.7] [Reference Citation Analysis (0)] |
| 4. | Emanuel EJ, Persad G, Upshur R, Thome B, Parker M, Glickman A, Zhang C, Boyle C, Smith M, Phillips JP. Fair Allocation of Scarce Medical Resources in the Time of Covid-19. N Engl J Med. 2020;382:2049-2055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1844] [Cited by in RCA: 1904] [Article Influence: 317.3] [Reference Citation Analysis (0)] |
| 5. | Ñamendys-Silva SA. Respiratory support for patients with COVID-19 infection. Lancet Respir Med. 2020;8:e18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 137] [Cited by in RCA: 124] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 6. | Bhatraju PK, Ghassemieh BJ, Nichols M, Kim R, Jerome KR, Nalla AK, Greninger AL, Pipavath S, Wurfel MM, Evans L, Kritek PA, West TE, Luks A, Gerbino A, Dale CR, Goldman JD, O'Mahony S, Mikacenic C. Covid-19 in Critically Ill Patients in the Seattle Region - Case Series. N Engl J Med. 2020;382:2012-2022. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1819] [Cited by in RCA: 1871] [Article Influence: 311.8] [Reference Citation Analysis (0)] |
| 7. | Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, Gattinoni L, van Haren F, Larsson A, McAuley DF, Ranieri M, Rubenfeld G, Thompson BT, Wrigge H, Slutsky AS, Pesenti A; LUNG SAFE Investigators; ESICM Trials Group. Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. JAMA. 2016;315:788-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2627] [Cited by in RCA: 3885] [Article Influence: 388.5] [Reference Citation Analysis (0)] |
| 8. | Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, Ji R, Wang H, Wang Y, Zhou Y. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91-95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2672] [Cited by in RCA: 2528] [Article Influence: 421.3] [Reference Citation Analysis (2)] |
| 9. | Lighter J, Phillips M, Hochman S, Sterling S, Johnson D, Francois F, Stachel A. Obesity in Patients Younger Than 60 Years Is a Risk Factor for COVID-19 Hospital Admission. Clin Infect Dis. 2020;71:896-897. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 810] [Cited by in RCA: 839] [Article Influence: 139.8] [Reference Citation Analysis (0)] |
| 10. | Mohamed S, Abo El-Hassan O, Rizk M, Ismail JH, Baioumy A. Death due to Cardiac Arrest in a Young Female With Highly Suspected COVID-19: A Case Report. Cureus. 2020;12:e10127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Du RH, Liu LM, Yin W, Wang W, Guan LL, Yuan ML, Li YL, Hu Y, Li XY, Sun B, Peng P, Shi HZ. Hospitalization and Critical Care of 109 Decedents with COVID-19 Pneumonia in Wuhan, China. Ann Am Thorac Soc. 2020;17:839-846. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 138] [Cited by in RCA: 152] [Article Influence: 25.3] [Reference Citation Analysis (9)] |
| 12. | Cha AE. Hospitals consider universal do-not-resuscitate orders for coronavirus patients. The Washington Post. 2020 Mar 25. Available from: https://www.washingtonpost.com/health/2020/03/25/coronavirus-patients-do-not-resucitate/. |
| 13. | Curtis JR, Kross EK, Stapleton RD. The Importance of Addressing Advance Care Planning and Decisions About Do-Not-Resuscitate Orders During Novel Coronavirus 2019 (COVID-19). JAMA. 2020;323:1771-1772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 186] [Article Influence: 31.0] [Reference Citation Analysis (0)] |
| 14. | Mahase E, Kmietowicz Z. Covid-19: Doctors are told not to perform CPR on patients in cardiac arrest. BMJ. 2020;368:m1282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 71] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 15. | Dillon N. Seattle ER doctor, nearly killed by coronavirus, ‘saved’ with experimental treatment: report. New York Daily News. 2020 Apr 14. Available from: https://www.nydailynews.com/coronavirus/ny-er-doctor-with-coronavirus-says-tocilizumab-saved-his-life-20200414-24bdl5m7fjfjpowkfedirbood4-story.html. |
| 16. | Bemtgen X, Krüger K, Supady A, Duerschmied D, Schibilsky D, Bamberg F, Bode C, Wengenmayer T, Staudacher DL. First Successful Treatment of Coronavirus Disease 2019 Induced Refractory Cardiogenic Plus Vasoplegic Shock by Combination of Percutaneous Ventricular Assist Device and Extracorporeal Membrane Oxygenation: A Case Report. ASAIO J. 2020;66:607-609. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 17. | Zhan WQ, Li MD, Xu M, Lu YB. Successful treatment of COVID-19 using extracorporeal membrane oxygenation, a case report. Eur Rev Med Pharmacol Sci. 2020;24:3385-3389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 18. | Shao F, Xu S, Ma X, Xu Z, Lyu J, Ng M, Cui H, Yu C, Zhang Q, Sun P, Tang Z. In-hospital cardiac arrest outcomes among patients with COVID-19 pneumonia in Wuhan, China. Resuscitation. 2020;151:18-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 221] [Cited by in RCA: 213] [Article Influence: 35.5] [Reference Citation Analysis (0)] |
| 19. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264-269, W64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21613] [Cited by in RCA: 18558] [Article Influence: 1091.6] [Reference Citation Analysis (0)] |
| 20. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52948] [Cited by in RCA: 48662] [Article Influence: 2862.5] [Reference Citation Analysis (3)] |
| 21. | Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. |
| 22. | Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, Lee M. Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State. JAMA. 2020;323:1612-1614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1511] [Cited by in RCA: 1637] [Article Influence: 272.8] [Reference Citation Analysis (0)] |
| 23. | Cai Q, Huang D, Ou P, Yu H, Zhu Z, Xia Z, Su Y, Ma Z, Zhang Y, Li Z, He Q, Liu L, Fu Y, Chen J. COVID-19 in a designated infectious diseases hospital outside Hubei Province, China. Allergy. 2020;75:1742-1752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 330] [Article Influence: 55.0] [Reference Citation Analysis (0)] |
| 24. | Cao J, Tu WJ, Cheng W, Yu L, Liu YK, Hu X, Liu Q. Clinical Features and Short-term Outcomes of 102 Patients with Coronavirus Disease 2019 in Wuhan, China. Clin Infect Dis. 2020;71:748-755. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 345] [Cited by in RCA: 337] [Article Influence: 56.2] [Reference Citation Analysis (0)] |
| 25. | Chen J, Qi T, Liu L, Ling Y, Qian Z, Li T, Li F, Xu Q, Zhang Y, Xu S, Song Z, Zeng Y, Shen Y, Shi Y, Zhu T, Lu H. Clinical progression of patients with COVID-19 in Shanghai, China. J Infect. 2020;80:e1-e6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 536] [Cited by in RCA: 524] [Article Influence: 87.3] [Reference Citation Analysis (0)] |
| 26. | Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, Cereda D, Coluccello A, Foti G, Fumagalli R, Iotti G, Latronico N, Lorini L, Merler S, Natalini G, Piatti A, Ranieri MV, Scandroglio AM, Storti E, Cecconi M, Pesenti A; COVID-19 Lombardy ICU Network. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574-1581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3537] [Cited by in RCA: 3876] [Article Influence: 646.0] [Reference Citation Analysis (0)] |
| 27. | Han H, Xie L, Liu R, Yang J, Liu F, Wu K, Chen L, Hou W, Feng Y, Zhu C. Analysis of heart injury laboratory parameters in 273 COVID-19 patients in one hospital in Wuhan, China. J Med Virol. 2020;92:819-823. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 152] [Cited by in RCA: 180] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 28. | Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35178] [Cited by in RCA: 30485] [Article Influence: 5080.8] [Reference Citation Analysis (13)] |
| 29. | Intensive Care National Audit and Research Centre. ICNARC report on COVID-19 in critical care: 01 May 2020. London: Intensive Care National Audit and Research Centre, 2020. |
| 30. | Li X, Guo Z, Li B, Zhang X, Tian R, Wu W, Zhang Z, Lu Y, Chen N, Clifford SP, Huang J. Extracorporeal Membrane Oxygenation for Coronavirus Disease 2019 in Shanghai, China. ASAIO J. 2020;66:475-481. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 127] [Cited by in RCA: 129] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 31. |
Ling L, So C, Shum HP, Chan PKS, Lai CKC, Kandamby DH, Ho E, So D, Yan WW, Lui G, Leung WS, Chan MC, Gomersall CD.
Critically ill patients with COVID-19 in Hong Kong: a multicentre retrospective observational cohort study |
| 32. | Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323:1061-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14113] [Cited by in RCA: 14869] [Article Influence: 2478.2] [Reference Citation Analysis (1)] |
| 33. | Wang L, Li X, Chen H, Yan S, Li D, Li Y, Gong Z. Coronavirus Disease 19 Infection Does Not Result in Acute Kidney Injury: An Analysis of 116 Hospitalized Patients from Wuhan, China. Am J Nephrol. 2020;51:343-348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 235] [Cited by in RCA: 272] [Article Influence: 45.3] [Reference Citation Analysis (29)] |
| 34. | Wang Y, Lu X, Li Y, Chen H, Chen T, Su N, Huang F, Zhou J, Zhang B, Yan F, Wang J. Clinical Course and Outcomes of 344 Intensive Care Patients with COVID-19. Am J Respir Crit Care Med. 2020;201:1430-1434. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 369] [Cited by in RCA: 363] [Article Influence: 60.5] [Reference Citation Analysis (0)] |
| 35. | Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, Huang H, Zhang L, Zhou X, Du C, Zhang Y, Song J, Wang S, Chao Y, Yang Z, Xu J, Zhou X, Chen D, Xiong W, Xu L, Zhou F, Jiang J, Bai C, Zheng J, Song Y. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:934-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4960] [Cited by in RCA: 5580] [Article Influence: 930.0] [Reference Citation Analysis (1)] |
| 36. | Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475-481. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6231] [Cited by in RCA: 6710] [Article Influence: 1118.3] [Reference Citation Analysis (1)] |
| 37. | Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054-1062. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17476] [Cited by in RCA: 18406] [Article Influence: 3067.7] [Reference Citation Analysis (13)] |
| 38. | Deng Y, Liu W, Liu K, Fang YY, Shang J, Zhou L, Wang K, Leng F, Wei S, Chen L, Liu HG. Clinical characteristics of fatal and recovered cases of coronavirus disease 2019 in Wuhan, China: a retrospective study. Chin Med J (Engl). 2020;133:1261-1267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 407] [Cited by in RCA: 446] [Article Influence: 74.3] [Reference Citation Analysis (0)] |
| 39. | Grein J, Ohmagari N, Shin D, Diaz G, Asperges E, Castagna A, Feldt T, Green G, Green ML, Lescure FX, Nicastri E, Oda R, Yo K, Quiros-Roldan E, Studemeister A, Redinski J, Ahmed S, Bernett J, Chelliah D, Chen D, Chihara S, Cohen SH, Cunningham J, D'Arminio Monforte A, Ismail S, Kato H, Lapadula G, L'Her E, Maeno T, Majumder S, Massari M, Mora-Rillo M, Mutoh Y, Nguyen D, Verweij E, Zoufaly A, Osinusi AO, DeZure A, Zhao Y, Zhong L, Chokkalingam A, Elboudwarej E, Telep L, Timbs L, Henne I, Sellers S, Cao H, Tan SK, Winterbourne L, Desai P, Mera R, Gaggar A, Myers RP, Brainard DM, Childs R, Flanigan T. Compassionate Use of Remdesivir for Patients with Severe Covid-19. N Engl J Med. 2020;382:2327-2336. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1926] [Cited by in RCA: 1900] [Article Influence: 316.7] [Reference Citation Analysis (0)] |
| 40. | Bauchner H, Golub RM, Zylke J. Editorial Concern-Possible Reporting of the Same Patients With COVID-19 in Different Reports. JAMA. 2020;323:1256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 18] [Reference Citation Analysis (1)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Health care sciences and services
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fan Y, Kurniawan A S-Editor: Wang JL L-Editor: A P-Editor: Li JH