Published online Jun 28, 2020. doi: 10.13105/wjma.v8.i3.275
Peer-review started: April 23, 2020
First decision: April 30, 2020
Revised: May 4, 2020
Accepted: June 17, 2020
Article in press: June 17, 2020
Published online: June 28, 2020
Processing time: 75 Days and 9.4 Hours
A diagnosis of gestational diabetes mellitus (GDM) negatively influences maternal mental health. There is a lack of systematic review and meta-analysis on prevalence of anxiety among GDM women.
To pool data from existing literature to determine the pooled estimates for the prevalence of anxiety among women diagnosed with GDM.
We searched multiple databases including MEDLINE, Cinahl, PubMed and Scopus to identify studies published up to 31 October 2019 with data on the prevalence of anxiety among women diagnosed with GDM. Data were extracted from published reports. Estimates were pooled using random-effects meta-analyses.
We reviewed 19 abstracts, retrieved 10 articles and included three studies incorporating 12744 GDM women from three countries. The pooled prevalence of anxiety was 29.5% (95%CI: 6.9, 52.0) among GDM women.
Prevalence of anxiety among GDM women was high. We suggest that epidemiological studies on anxiety should be conducted urgently as it merits clinical attention. In addition, it is important to identify factors associated with anxiety among women diagnosed with GDM.
Core tip: This is a systematic review and meta-analysis reporting the pooled prevalence of anxiety among gestational diabetes mellitus patients which stood at 29.5%.
- Citation: Lee KW, Loh HC, Chong SC, Ching SM, Devaraj NK, Tusimin M, Abdul Hamid H, Hoo FK. Prevalence of anxiety among gestational diabetes mellitus patients: A systematic review and meta-analysis. World J Meta-Anal 2020; 8(3): 275-284
- URL: https://www.wjgnet.com/2308-3840/full/v8/i3/275.htm
- DOI: https://dx.doi.org/10.13105/wjma.v8.i3.275
The prevalence of gestational diabetes mellitus (GDM) has been increasing over the past decades[1,2]. Globally, GDM has been reported as a leading cause of morbidity and mortality among both the infants and their mother[3,4]. Mothers with GDM are at increased risk of getting pregnancy complications such as preterm delivery, preeclampsia, abnormal birth weight, metabolic and electrolyte disorders[5]. Studies also indicated that GDM may persist after postpartum and subsequently develop into overt diabetes mellitus, and it was estimated that the risk for developing diabetes mellitus after GDM increased linearly with the duration of follow-up ranged from 19.72% at 10 years. The estimated risks for type-2 diabetes mellitus ranged from 19.7% at 10 years to 39.0% at 30 years[6]. Neonates born to GDM mothers are at higher risk of suffering from adverse neonatal outcomes such as abnormal birth weight, congenital anomalies, hypoglycaemia and longer duration in neonatal intensive care unit for further investigation[7-9].
Previous studies showed that the prevalence of depression among mothers with GDM were ranging from 25.9% to 56.7%[10,11] and the prevalence of anxiety was within a range of 4.8% to 57.7%[12,13]. Anxiety is a normal reaction to stress which involves both psychological and physical reactions. It becomes clinically significant when the anxiety grows out of proportion to the situation and causes functional impairment. Anxiety disorders are among the most common mental illnesses, and are characterized by feelings of tension, worrying thoughts and physical changes such as increased blood pressure. People with anxiety disorders usually have recurring intrusive thoughts or concerns. They may avoid certain situations out of worry. They may also have physical symptoms such as sweating, trembling, dizziness or a rapid heartbeat[14]. With a remarkable increase in lifetime prevalence, anxiety has become a public health burden worldwide, causing increased use of mental health services and loss of productivity[15]. In particular, anxiety is a common psychiatric condition that affects up to one-fifth of the pregnant mothers[16] and is significantly associated with postpartum depression (odds ratio = 2.6, 95%CI: 2.0, 3.5) and reduced odds of breastfeeding (odds ratio = 0.63, 95%CI: 0.5, 0.7)[17]. Thus, anxiety and related mental conditions could pose negative effects on child development[18]. A high state of anxiety is found in 15.8% of pregnant women, while 12.5% of women suffer high trait anxiety[19]. Similarly, pregnant mothers with GDM were more anxious than pregnant women with other medical problems or healthy pregnant women[20].
There are multiple factors associated with anxiety during pregnancy, including current or past pregnancy-related complications, previous pregnant loss and personal history of mental illness[21]. Study have also shown that women with GDM experience significantly worse quality of life[22]. However, findings from previous studies indicate that there is a lack of data on the epidemiology of antenatal anxiety among GDM patients. Therefore, we aimed to determine the pooled prevalence of anxiety among GDM patients by conducting a meta-analysis.
This present study was registered in the Medical Research and Ethics Committee, Ministry of Health Malaysia (registration number: NMRR-20-117-52644), and conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses[23]. As this work only involved secondary data retrieval and analysis, no ethical approval was sought.
Two investigators (Lee KW and Loh HC) independently searched MEDLINE, Cinahl, PubMed and Scopus databases for potential studies published in journals from inception to 31 October 2019. We used following search terms: (Anxiety OR anxiety symptom OR anxiety disorder OR generalized anxiety disorder OR panic disorder OR panic attack OR agoraphobia OR phobia OR specific phobia OR specific phobic disorder OR medication-induced anxiety disorder OR medical condition induced anxiety disorder OR social anxiety disorder) AND (prevalence) AND (gestational diabetes OR GDM OR gestational diabetes mellitus OR diabetes in pregnancy). The search strategies with the Boolean or phrase operators were shown in the Supplementary material 1. Studies in English, available in full-text and conducted among humans were searched. Then, we removed duplications using Endnote, after that we screened the title and abstracts for its suitability. Finally, articles with their full text were assessed for eligibility to be recruited into the quantitative analysis.
Any studies that reported the prevalence or percentage for anxiety symptoms or anxiety disorders among GDM patients and fulfilled the inclusion criteria were analysed. The inclusion criteria were as follows: (1) Diagnosing or screening of anxiety was made according to Diagnostic and Statistical Manual of Mental Disorders/International Classification of Diseases diagnostic criteria or by any screening tools; (2) Participants in the study were diagnosed with GDM; and (3) Studies were published in English peer-reviewed journal from inception to 31 October 2019. Other related studies were also included through careful review of the reference lists of related review articles and reverse-forward citation tracking. Studies were excluded if they included only pregnant mothers with pre-existing diabetes mellitus, were of case-control design or examined anxiety prior to the diagnosis of GDM.
All relevant articles identified through the above databases were imported into Endnote programme X5 version. Initially, we performed de-duplication. Two investigators independently screened each title and abstract for suitability based on the search strategies mentioned above. Then, full-text articles were assessed based on the inclusion criteria mentioned above. Any disagreements between the investigators were resolved through discussions before the final consensus for quantitative analysis was reached.
The following data were extracted from every study: The last name of the first author, year of publication, country, sample size, study design, recruitment duration, timing of GDM diagnosis, GDM diagnosis guidelines, assessment of anxiety guidelines, and timing of anxiety assessment. The outcomes measures included the numbers of GDM patients with anxiety symptoms or disorders and total number of GDM patients. Two investigators (Lee KW and Loh HC) individually extracted the data and assessed the study quality, with differences resolved through discussion with the third and fourth investigators (Ching SM and Hoo FK).
The quality of the individual studies was determined using the checklist of Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)[24]. The aim and use of STROBE were to assess the strengths and weaknesses of the studies reported in the medical literature. STROBE results also helps readers to know what was planned, done and found, as well as what is incomplete and inadequate in the reporting of the articles. The tool consists of 22 items to help assess the important components found in observational studies. In certain instances where the information provided was insufficient in order to make judgement for a certain item, that item was graded with a “0”, rendering the item as having a high risk of bias. Each article’s quality was graded as “good” if the STROBE score was ≥ 14; or graded as “poor” if the STROBE score was < 14. Two investigators (Devaraj NK and Maiza T) individually assessed the study quality, with differences resolved by discussion with the third and fourth investigators (Ching SM and Hoo FK). Studies were included in analysis regardless of STROBE score and grade.
A random-effects (DerSimonian and Laird Method) meta-analysis method was employed to pool the prevalence estimated from these related studies and was reported with a 95%CI. I2 index was used to assess the studies heterogeneity (i.e. low is < 25%, moderate 25%–50%, and high > 50%) that indicated the total percent of discrepancy due to variation in the included studies[25]. For statistical analysis, Open Meta (Analyst) software was used, this software can be accessed and downloaded from http://www.cebm.brown.edu/openmeta/index.html[26]. Funnel plot was generated using The Jamovi project computer Software which can be retrieved from https://www.jamovi.org[27].
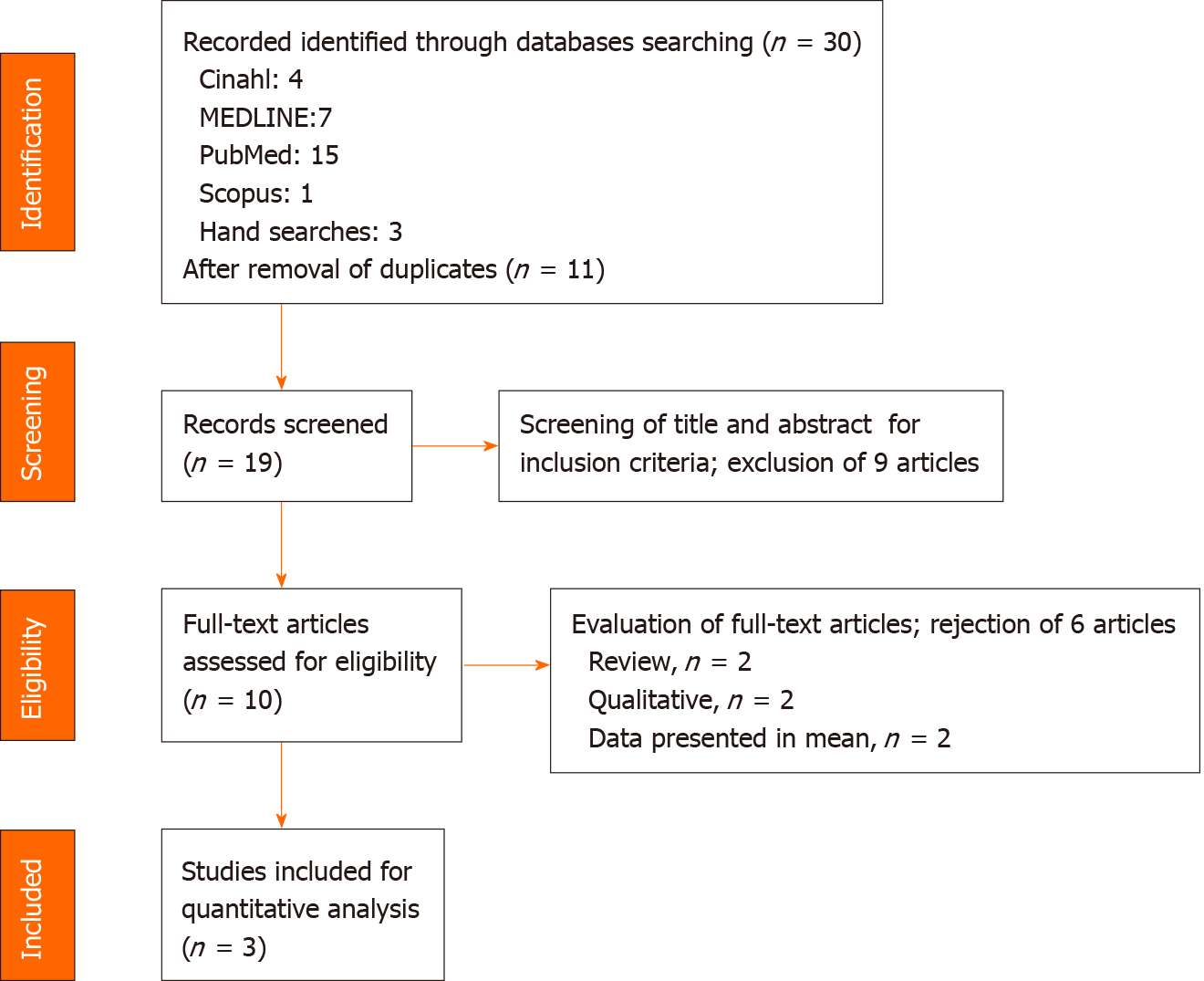
Thirty manuscripts were identified in the initial screening as shown in Figure 1. After removal of duplicate articles (n = 11), a total of 19 studies were retrieved for further assessment. After screening for its suitability through title and abstract, 10 studies fulfilled both our inclusion and exclusion criteria. After careful evaluation of the 10 articles, only three studies were eligible for quantitative analysis in this study.
The main characteristics of the included studies are shown in Table 1. A total sample of 12744 women diagnosed with GDM was included in the analysis. The respondents were diagnosed using either American Diabetes Association or World Health Organization guidelines. These studies were conducted in Canada[13], Ireland[12] and Malaysia[28]. In terms of diagnosing or screening for anxiety, Beka et al[13] (2018) used the diagnostic criteria of the International Classification of Diseases- Ninth version (ICD-9) (prior to 2002) and the International Classification of Diseases- Tenth version (ICD-10) (2002 onward); while Egan et al[12] (2017) and Lee et al[28] (2019) used 21-item Depression Anxiety Stress Scale (DASS-21). For quality assessment, we assigned each study with an overall rating based on the tool derived from STROBE checklist. The overall quality of included studies appeared to be good.
| Ref. | Year | Country | Study setting | Diagnostic guidelines for GDM | Diagnostic or screening methods for anxiety | Mean age of GDM patients | Ethnicity among GDM | Number of GDM patients with anxiety | Total number of GDM patients | Prevalence of anxiety | Quality (score) |
| Beka et al[13] | 2018 | Canada | Population | ADA | ICD-9 (Prior to 2002) and ICD-10 (2002 onward) | 32.1 ± 5.3 | Aboriginal (6.9%); Caucasian (70.8%), Chinese (6.9%), South Asian (15.5%) | 584 | 12140 | 4.8 | Good (18) |
| Egan et al[12] | 2017 | Ireland | Hospital | N/A | 21-item Depression Anxiety Stress Scale | 33.6 ± 4.8 | Caucasian (89.7); Non-Caucasian (9%) | 45 | 78 | 57.7 | Good (14) |
| Lee et al[28] | 2019 | Malaysia | Hospital | WHO | 21-item Depression Anxiety Stress Scale | 32.3 ± 4.9 | Malay (82.3%); Non-Malay (17.7%) | 147 | 526 | 27.9 | Good (15) |
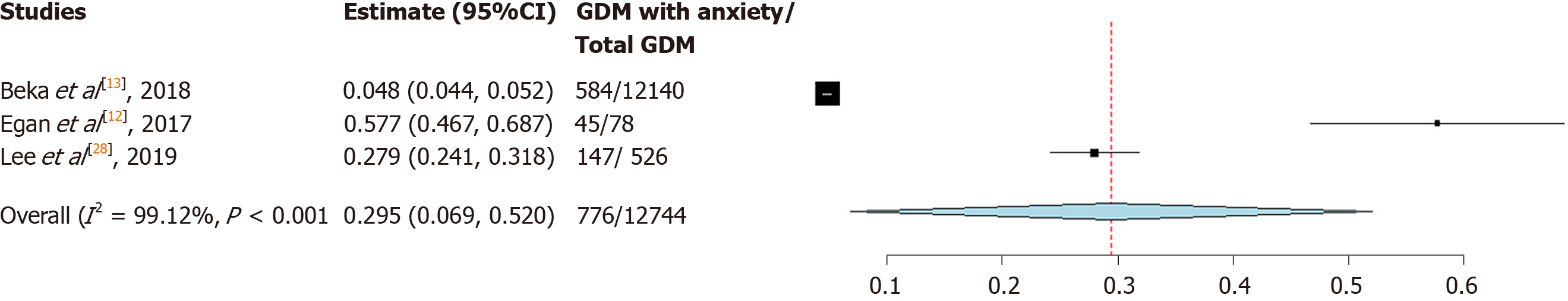
The overall pooled prevalence of anxiety was 29.5% (95%CI: 6.9, 52.0) (Figure 2). The pooled prevalence of anxiety using DASS-21 was higher than prevalence of anxiety using ICD-9/10 (42.4% vs 4.8%). Sensitivity analysis reveals that study by Beka et al[13] had substantial influences on the overall prevalence, which caused prevalence of anxiety to increase from 29.5% (95%CI: 6.9, 52.0) to 42.4% (95%CI: 13.2, 71.5). On the other hand, removal of studies by Egan et al[12], 2017 or Lee et al[28], 2019, it did not cause statistically significant changes to the overall prevalence of anxiety (Supplementary material 2). Indeed, funnel plot (Supplementary material 3) suggested that there was publication bias. Nevertheless, we did not exclude any studies from the meta-analysis in view there was only three studies available.
We assigned the studies with an overall rating based on STROBE checklist. All three studies received an overall “Good” quality with a score of ≥ 14 over 22 (Supplementary materials 4-6). In summarizing the results, we concluded that all studies had methodological issues such as not describing any efforts to address potential sources of bias, how the missing data were addressed, and lacking of sensitivity analysis.
Our systematic review and meta-analysis offer preliminary evidence regarding the prevalence of anxiety among GDM patients. The results indicated that the pooled prevalence of anxiety among GDM patients was 29.5%.
Several reasons may have contributed to the high heterogeneity (I2 = 99.12%) in the pooled prevalence that was seen in our systematic review and meta-analysis. First, there are differences in terms of the methodological approach used in different studies for the detection of anxiety. The diagnostic method would identify specific anxiety disorders with more stringent criteria, while the screening method served as case identification. Diagnostic versus screening criteria used by different studies for the clinically significant anxiety symptoms were omitted. For instance, Beka et al[13] (2018) used ICD-9 and ICD-10 to diagnose anxiety disorder while Egan et al[12] (2017) and Lee et al[28] (2019) used DASS-21 for screening of anxiety symptoms. Unlike ICD, DASS-21 is a screening tool with 21 items which consists of three domains assessing depression, anxiety and stress[29]. DASS-21 English version has been translated and validated into Malay version by Musa et al[30]. DASS-21 has distinctive cut-off value for severity rating; anxiety is detected if anxiety domain score is ≥ 8 (Mild and above)[29], however it should be noted that clinically significant anxiety symptoms should be of moderate and above in its severity.
The vast disparity of anxiety prevalence between study population may be one of the reasons for the discrepancy. Study by Beka et al[13] (2018) was a population-based study, while studies by Egan et al[12] (2017) and Lee et al[28] (2019) were hospital-based study. In the study by Beka et al[13] (2018), there was no sample size calculation, and the patients’ medical information were obtained via health services databases. The weakness of health services databases is that it contains information about formal diagnosis and healthcare services provided for patients, yet it didn’t provide results of mental health screening, therefore the prevalence of anxiety (4.8%) reported by Beka et al[13] (2018) may not reflect the prevalence of clinically significant anxiety faced by GDM patients. We noted that two studies which conducted in hospital (Egan et al[12], 2017 and Lee et al[28], 2019) had sample size calculation; these two studies achieved sufficient sample number. However, Egan et al[12] (2017) had a sample size of less than 100 for GDM patients. Hence, the prevalence of clinically significant anxiety symptoms in Egan et al[12] (2017) (57.7%) was higher compared to Lee et al[28] (2019) (27.9%). Sample size remains an important criteria when determining the prevalence of anxiety, as studies have shown the positive correlation between sample size and prevalence[31,32]. Hence, all these reasons might have contributed to the high heterogeneity in the prevalence of anxiety in our study.
More than half of pregnant women showed moderate anxiety during their pregnancy[33,34]. Anxiety during pregnancy could be due to worries about health and well-being of the babies and the mothers themselves. The worries also extend to the concern of parenting and the transition to maternal role after birth[28]. A meta-analysis reported that antenatal anxiety could increase the risk for adverse birth outcomes such as preterm delivery (relative risk = 1.50, 95%CI: 1.33, 1.70) and low birth weight (relative risk = 1.76, 95%CI: 1.32, 2.33)[35].
Around 11.5% of pregnant women in Asia are affected by GDM[36]. Recent meta-analysis reported that hyperglycaemia in pregnancy increases the risk for adverse outcomes such as caesarean section (OR = 1.59, 95%CI: 1.49, 1.70), large for gestational age (OR = 2.11, 95%CI: 1.73, 2.58), macrosomia (OR = 2.06, 95%CI: 1.86, 2.28), neonatal hypoglycaemia (OR = 1.37, 95%CI: 1.20, 1.57), gestational hypertension (OR = 1.91, 95%CI: 1.49, 2.43) and pre-eclampsia (OR = 2.15, 95%CI: 1.45, 3.19)[5]. GDM patients are at higher risk for experiencing anxiety as compared to pregnant women without medical complications[20]. Similarly, the adverse birth outcomes could be exacerbated if women with GDM experiences anxiety during pregnancy.
Antenatal anxiety is an evolving field, and unlike depression, only a few studies have been conducted among GDM patients. However, studies have reported that antenatal anxiety is more prevalent than antenatal depression[28,34], and this study reports anxiety symptoms are prevalent in GDM patients. In order to promote the detection of antenatal anxiety, several screening tools have been recently recommended by National Institute for Health and Care Excellence, which include Generalized Anxiety Disorder scale, GAD-2[37]. GAD-2 can be used as an ultra-brief screening scale for antenatal anxiety. Even so, other screening scales are more commonly used in clinical setting as compared to GAD-2, such as DASS-21[29], Edinburgh Postnatal Depression Scale[38], Hospital Anxiety and Depression Scale – Anxiety subscale[39], State-Trait Anxiety Inventory[40], GAD-7[41], Brief Measure of Worry Severity[42], Cambridge Worry Scale[43] and Wijma Delivery Expectancy/Experience Questionnaire –Version A[44].
Mental illness is a leading cause of maternal morbidity and even endangers maternal life especially in high -income countries[45]. Indirectly it also impacts new-born babies, causing perinatal morbidity and mortality as well as the impact on the long-term child development[46,47]. The National Institute for Health and Clinical Excellence (NICE) has emphasised that perinatal mental illness is one of the most important issues in women’s health that need to be highlighted, especially in the postpartum period[48,49].
The prevalence of postpartum anxiety disorders varies. Reck et al[50] (2008) and Miller et al[51] (2006) found a comparable percentage of postpartum women having anxiety disorder, at 11.1 % and 10 % respectively. Matthey et al[52] documented that 16.2% of mothers were diagnosed with a pure anxiety disorder while Wenzel et al[53] (2005) noted a prevalence rate of 8.2% for generalized anxiety disorder.
There were many reviews confined to maternal depression in postpartum period but there were scarcity of data on anxiety disorder despite of the high health risks for both mother and child associated with postpartum disorders[50]. Maternal anxiety disorder is part of a broad spectrum condition comprising of mild to severe mental illnesses such as bipolar disorder and psychotic disorder. It is common that both anxiety and depression co-exist in postpartum women[51,54].
Socio-demographic factors and socioeconomically deprived status have important impacts on maternal mental illness. The most common risk factors include age of more than 35 year old, single parent, lower educational level and low -income family[47,55]. Women with greater socioeconomic deprivation are more likely to have maternal mental illness than those with lesser degree of socioeconomic deprivation[56,57]. An early recognition of women at risk and implementation of effective intervention are essential as preventive measures to treat maternal mental illness accordingly, aiming to reduce the complications related to maternal mental illness.
To date, this is the first systematic and meta-analysis on anxiety among patient with GDM. This study clearly indicates that anxiety is prevalent among GDM patients. The finding of this review is consistent with the previous literature pertaining to anxiety among pregnant women experiencing medical complications. However, there are several limitations. Strict inclusion/exclusion criteria and a paucity of literature on the topic of interest have resulted in the inclusion of only three papers. However, according to Valentine et al[58], 2010, the minimum number of studies needed to conduct a meta-analysis is two. On top of that, we did sensitivity analysis and funnel plot to show the publication bias. Nevertheless, due care is necessary when interpreting the results as at least 5 studies or more are needed to reasonably and consistently achieve powers from the random-effects meta-analyses that are greater than the studies that contribute to them[59]. Second, the pooled sample size is not large enough to reflect the anxiety prevalence in clinical setting, therefore limiting the generalizability of our study findings.
In conclusion, our study provides an estimation of the prevalence of anxiety among patients with GDM. Our study showed that the pooled prevalence was high at 29.5%. We recommend that more epidemiological studies on anxiety during pregnancy to be conducted in this particular population. In addition, it is important to identify factors associated with anxiety during pregnancy so that early detection and intervention can be implemented to improve various obstetric and mental health outcomes.
There is lack of systematic review and meta-analysis on prevalence of anxiety among GDM women.
The systematic review and meta-analysis reporting the pooled prevalence of anxiety among GDM patients is high (29.5%).
Authors aimed to pool data from existing literature to determine the pool estimates for the prevalence of anxiety among women diagnosed with GDM.
Multiple databases including MEDLINE, Cinahl, PubMed and Scopus were searched to identify studies published up to 31 October 2019 with data on the prevalence of anxiety among women diagnosed with GDM.
Total 19 abstracts, retrieved 10 articles and included three studies incorporating 12744 GDM women from three countries were reviewed. The pooled prevalence of anxiety was 29.5% among GDM women.
The results suggest that epidemiological studies on anxiety should be conducted urgently as it merits clinical attention. In addition, it is important to identify factors associated with anxiety among women diagnosed with GDM.
We would like to thank the Director General of Health Malaysia for his permission to publish this article.
| 1. | Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet. 2009;373:1773-1779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2141] [Cited by in RCA: 2400] [Article Influence: 141.2] [Reference Citation Analysis (1)] |
| 2. | Rayanagoudar G, Hashi AA, Zamora J, Khan KS, Hitman GA, Thangaratinam S. Quantification of the type 2 diabetes risk in women with gestational diabetes: a systematic review and meta-analysis of 95,750 women. Diabetologia. 2016;59:1403-1411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 150] [Cited by in RCA: 206] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 3. | Bener A, Saleh NM, Al-Hamaq A. Prevalence of gestational diabetes and associated maternal and neonatal complications in a fast-developing community: global comparisons. Int J Womens Health. 2011;3:367-373. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 119] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 4. | Veeraswamy S, Vijayam B, Gupta VK, Kapur A. Gestational diabetes: the public health relevance and approach. Diabetes Res Clin Pract. 2012;97:350-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 5. | Farrar D, Simmonds M, Bryant M, Sheldon TA, Tuffnell D, Golder S, Dunne F, Lawlor DA. Hyperglycaemia and risk of adverse perinatal outcomes: systematic review and meta-analysis. BMJ. 2016;354:i4694. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 280] [Cited by in RCA: 271] [Article Influence: 27.1] [Reference Citation Analysis (0)] |
| 6. | Li Z, Cheng Y, Wang D, Chen H, Chen H, Ming WK, Wang Z. Incidence Rate of Type 2 Diabetes Mellitus after Gestational Diabetes Mellitus: A Systematic Review and Meta-Analysis of 170,139 Women. J Diabetes Res. 2020;2020:3076463. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 128] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 7. | Mak JKL, Lee AH, Pham NM, Pan XF, Tang L, Binns CW, Sun X. Gestational diabetes incidence and delivery outcomes in Western China: A prospective cohort study. Birth. 2019;46:166-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 8. | Thevarajah A, Simmons D. Risk factors and outcomes for neonatal hypoglycaemia and neonatal hyperbilirubinaemia in pregnancies complicated by gestational diabetes mellitus: a single centre retrospective 3-year review. Diabet Med. 2019;36:1109-1117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Somohano-Mendiola N, Champion JD, Vatcheva K. Assessment of Gestational Diabetes Mellitus Outcomes for Hispanic Women Living in the Rio Grande Valley. Hisp Health Care Int. 2019;17:111-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Chazotte C, Freda MC, Elovitz M, Youchah J. Maternal depressive symptoms and maternal-fetal attachment in gestational diabetes. J Womens Health. 1995;4:375-380. [RCA] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 11. | Natasha K, Hussain A, Khan AK. Prevalence of depression among subjects with and without gestational diabetes mellitus in Bangladesh: a hospital based study. J Diabetes Metab Disord. 2015;14:64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 12. | Egan AM, Dunne FP, Lydon K, Conneely S, Sarma K, McGuire BE. Diabetes in pregnancy: worse medical outcomes in type 1 diabetes but worse psychological outcomes in gestational diabetes. QJM. 2017;110:721-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (1)] |
| 13. | Beka Q, Bowker S, Savu A, Kingston D, Johnson JA, Kaul P. Development of Perinatal Mental Illness in Women With Gestational Diabetes Mellitus: A Population-Based Cohort Study. Can J Diabetes. 2018;42:350-355.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 14. | Major B, Cozzarelli C, Horowitz MJ. Encyclopedia of psychology: 8 Volume set. New York and Washington: Oxford University Press and the American Psychological Association, 2000. |
| 15. | Sowers KM, Dulmus CN, Linn BK. Mental Illness: Worldwide. In: Encyclopedia of Social Work. National Association of Social Workers Press and Oxford University Press, 2019. [DOI] [Full Text] |
| 16. | Soto-Balbuena C, Rodríguez MF, Escudero Gomis AI, Ferrer Barriendos FJ, Le HN, Pmb-Huca G. Incidence, prevalence and risk factors related to anxiety symptoms during pregnancy. Psicothema. 2018;30:257-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 21] [Reference Citation Analysis (0)] |
| 17. | Grigoriadis S, Graves L, Peer M, Mamisashvili L, Tomlinson G, Vigod SN, Dennis CL, Steiner M, Brown C, Cheung A, Dawson H, Rector NA, Guenette M, Richter M. A systematic review and meta-analysis of the effects of antenatal anxiety on postpartum outcomes. Arch Womens Ment Health. 2019;22:543-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 110] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 18. | Netsi E, Pearson RM, Murray L, Cooper P, Craske MG, Stein A. Association of Persistent and Severe Postnatal Depression With Child Outcomes. JAMA Psychiatry. 2018;75:247-253. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 342] [Cited by in RCA: 439] [Article Influence: 54.9] [Reference Citation Analysis (0)] |
| 19. | Podvornik N, Globevnik Velikonja V, Praper P. Depression and Anxiety in Women During Pregnancy in Slovenia. Zdr Varst. 2015;54:45-50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Abrar A, Fairbrother N, Smith AP, Skoll A, Albert AYK. Anxiety among women experiencing medically complicated pregnancy: A systematic review and meta-analysis. Birth. 2020;47:13-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 21. | Biaggi A, Conroy S, Pawlby S, Pariante CM. Identifying the women at risk of antenatal anxiety and depression: A systematic review. J Affect Disord. 2016;191:62-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1118] [Cited by in RCA: 1041] [Article Influence: 104.1] [Reference Citation Analysis (0)] |
| 22. | Marchetti D, Carrozzino D, Fraticelli F, Fulcheri M, Vitacolonna E. Quality of Life in Women with Gestational Diabetes Mellitus: A Systematic Review. J Diabetes Res. 2017;2017:7058082. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 64] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 23. | Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15040] [Cited by in RCA: 16694] [Article Influence: 1517.6] [Reference Citation Analysis (1)] |
| 24. | Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M; STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology. 2007;18:805-835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1209] [Cited by in RCA: 2030] [Article Influence: 106.8] [Reference Citation Analysis (0)] |
| 25. | Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539-1558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21630] [Cited by in RCA: 27034] [Article Influence: 1126.4] [Reference Citation Analysis (0)] |
| 26. | Wallace BC, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH. Closing the gap between methodologists and end-users: R as a computational back-end. J Stat Softw. 2012;49:1-15. [RCA] [DOI] [Full Text] [Cited by in Crossref: 503] [Cited by in RCA: 511] [Article Influence: 36.5] [Reference Citation Analysis (1)] |
| 27. | Jamovi. The jamovi project (2020). Jamovi (Version 1.2). Available from: https://www.jamovi.org. |
| 28. | Lee KW, Ching SM, Hoo FK, Ramachandran V, Chong SC, Tusimin M, Mohd Nordin N. Prevalence and factors associated with depressive, anxiety and stress symptoms among women with gestational diabetes mellitus in tertiary care centres in Malaysia: a cross-sectional study. BMC Pregnancy Childbirth. 2019;19:367. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 29. | Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33:335-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6494] [Cited by in RCA: 7999] [Article Influence: 258.0] [Reference Citation Analysis (0)] |
| 30. | Musa R, Fadzil MA, Zain Z. Translation, validation and psychometric properties of Bahasa Malaysia version of the Depression Anxiety and Stress Scales (DASS). ASEAN J Psychiatr. 2007;8:82-89. |
| 31. | Guo X, Zheng L, Zhang X, Zou L, Li J, Sun Z, Hu J, Sun Y. The prevalence and heterogeneity of prehypertension: a meta-analysis and meta-regression of published literature worldwide. Cardiovasc J Afr. 2012;23:44-50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 32. | Arya R, Antonisamy B, Kumar S. Sample size estimation in prevalence studies. Indian J Pediatr. 2012;79:1482-1488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 195] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 33. | Faisal-Cury A, Rossi Menezes P. Prevalence of anxiety and depression during pregnancy in a private setting sample. Arch Womens Ment Health. 2007;10:25-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 182] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 34. | Lee AM, Lam SK, Sze Mun Lau SM, Chong CS, Chui HW, Fong DY. Prevalence, course, and risk factors for antenatal anxiety and depression. Obstet Gynecol. 2007;110:1102-1112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 427] [Cited by in RCA: 459] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 35. | Ding XX, Wu YL, Xu SJ, Zhu RP, Jia XM, Zhang SF, Huang K, Zhu P, Hao JH, Tao FB. Maternal anxiety during pregnancy and adverse birth outcomes: a systematic review and meta-analysis of prospective cohort studies. J Affect Disord. 2014;159:103-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 433] [Cited by in RCA: 383] [Article Influence: 31.9] [Reference Citation Analysis (0)] |
| 36. | Lee KW, Ching SM, Ramachandran V, Yee A, Hoo FK, Chia YC, Wan Sulaiman WA, Suppiah S, Mohamed MH, Veettil SK. Prevalence and risk factors of gestational diabetes mellitus in Asia: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2018;18:494. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 239] [Cited by in RCA: 314] [Article Influence: 39.3] [Reference Citation Analysis (0)] |
| 37. | Antenatal N. Postnatal mental health: Clinical management and service guidance (CG192). London: National Institute for Health and Care Excellence, 2014. |
| 38. | Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782-786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8260] [Cited by in RCA: 9922] [Article Influence: 254.4] [Reference Citation Analysis (0)] |
| 39. | Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28548] [Cited by in RCA: 32845] [Article Influence: 763.8] [Reference Citation Analysis (0)] |
| 40. | Spielberger CD, Gorsuch RL, Lushene RE. Lushene RE. State-Trait Anxiety Inventory (STAI). Test Manual for Form X: Consulting Psychologists Press, 1968. |
| 41. | Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092-1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11947] [Cited by in RCA: 20791] [Article Influence: 1039.6] [Reference Citation Analysis (0)] |
| 42. | Gladstone GL, Parker GB, Mitchell PB, Malhi GS, Wilhelm KA, Austin MP. A Brief Measure of Worry Severity (BMWS): personality and clinical correlates of severe worriers. J Anxiety Disord. 2005;19:877-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 59] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 43. | Green JM, Kafetsios K, Statham HE, Snowdon CM. Factor structure, validity and reliability of the Cambridge Worry Scale in a pregnant population. J Health Psychol. 2003;8:753-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 167] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 44. | Wijma K, Wijma B, Zar M. Psychometric aspects of the W-DEQ; a new questionnaire for the measurement of fear of childbirth. J Psychosom Obstet Gynaecol. 1998;19:84-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 446] [Cited by in RCA: 548] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 45. | Oates M. Perinatal psychiatric disorders: a leading cause of maternal morbidity and mortality. Br Med Bull. 2003;67:219-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 195] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 46. | Jablensky AV, Morgan V, Zubrick SR, Bower C, Yellachich LA. Pregnancy, delivery, and neonatal complications in a population cohort of women with schizophrenia and major affective disorders. Am J Psychiatry. 2005;162:79-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 375] [Cited by in RCA: 315] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 47. | Ban L, Gibson JE, West J, Fiaschi L, Oates MR, Tata LJ. Impact of socioeconomic deprivation on maternal perinatal mental illnesses presenting to UK general practice. Br J Gen Pract. 2012;62:e671-e678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 60] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 48. | The National Institute for Health and Care Excellence. Antenatal and postnatal mental health: the NICE guideline on clinical management and service guidance. British Psychological Society, 2007. |
| 49. | Feldman R, Granat A, Pariente C, Kanety H, Kuint J, Gilboa-Schechtman E. Maternal depression and anxiety across the postpartum year and infant social engagement, fear regulation, and stress reactivity. J Am Acad Child Adolesc Psychiatry. 2009;48:919-927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 465] [Cited by in RCA: 525] [Article Influence: 30.9] [Reference Citation Analysis (0)] |
| 50. | Reck C, Struben K, Backenstrass M, Stefenelli U, Reinig K, Fuchs T, Sohn C, Mundt C. Prevalence, onset and comorbidity of postpartum anxiety and depressive disorders. Acta Psychiatr Scand. 2008;118:459-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 198] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 51. | Miller RL, Pallant JF, Negri LM. Anxiety and stress in the postpartum: is there more to postnatal distress than depression? BMC Psychiatry. 2006;6:12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 154] [Cited by in RCA: 166] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 52. | Matthey S, Barnett B, Howie P, Kavanagh DJ. Diagnosing postpartum depression in mothers and fathers: whatever happened to anxiety? J Affect Disord. 2003;74:139-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 345] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 53. | Wenzel A, Haugen EN, Jackson LC, Brendle JR. Anxiety symptoms and disorders at eight weeks postpartum. J Anxiety Disord. 2005;19:295-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 237] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 54. | Ross LE, McLean LM. Anxiety disorders during pregnancy and the postpartum period: A systematic review. J Clin Psychiatry. 2006;67:1285-1298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 412] [Cited by in RCA: 401] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 55. | Nager A, Johansson LM, Sundquist K. Are sociodemographic factors and year of delivery associated with hospital admission for postpartum psychosis? A study of 500,000 first-time mothers. Acta Psychiatr Scand. 2005;112:47-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 56. | Rich-Edwards JW, Kleinman K, Abrams A, Harlow BL, McLaughlin TJ, Joffe H, Gillman MW. Sociodemographic predictors of antenatal and postpartum depressive symptoms among women in a medical group practice. J Epidemiol Community Health. 2006;60:221-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 401] [Cited by in RCA: 424] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 57. | Wall-Wieler E, Carmichael SL, Urquia ML, Liu C, Hjern A. Severe maternal morbidity and postpartum mental health-related outcomes in Sweden: a population-based matched-cohort study. Arch Womens Ment Health. 2019;22:519-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 58. | Valentine JC, Pigott TD, Rothstein HR. How many studies do you need? A primer on statistical power for meta-analysis. J Educ Behav Stat. 2010;35:215-247. [DOI] [Full Text] |
| 59. | Jackson D, Turner R. Power analysis for random-effects meta-analysis. Res Synth Methods. 2017;8:290-302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 342] [Cited by in RCA: 414] [Article Influence: 46.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Malaysia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Byeon H S-Editor: Wang JL L-Editor: A E-Editor: Li X