Published online May 31, 2019. doi: 10.13105/wjma.v7.i5.249
Peer-review started: March 4, 2019
First decision: March 27, 2019
Revised: May 7, 2019
Accepted: May 11, 2019
Article in press: May 11, 2019
Published online: May 31, 2019
Processing time: 34 Days and 15.8 Hours
Endoscopic retrograde cholangiopancreatography (ERCP) plays a major role in the investigation and treatment of pancreaticobiliary diseases. However, post-ERCP pancreatitis (PEP) is a severe adverse effect. Prior meta-analyses have shown that prophylactic PS was useful for preventing PEP. However, abstract reports and patients who underwent endoscopic ampullectomy were included in the previous analyses. In addition, two meta-analyses involved non-randomized controlled trials (RCTs). The efficacy of PS for preventing severe PEP was different in each meta-analysis. Therefore, we performed the current meta-analysis, which included only full-text articles, and added new findings.
To reveal the efficacy of prophylactic pancreatic stent (PS) placement for preventing PEP.
We searched the MEDLINE, Cochrane Library and PubMed databases for related RCTs. Among the reports retrieved, 11 studies were included in this meta-analysis. All full-text articles were published between 1993 and 2016. A total of 1475 patients were enrolled in the included studies; of these patients, 734 had a PS inserted, and 741 did not have a PS inserted. PEP and severe PEP occurrence were evaluated in this meta-analysis.
PEP was observed in all studies and occurred in 39 (5.3%) patients who received a PS. On the other hand, PEP occurred in 141 (19%) patients who did not receive a PS. The occurrence of PEP was significantly lower in the patients who underwent PS placement than in the patients who did not receive a PS (OR = 0.32; 95%CI: 0.23-0.45; P < 0.001). In addition, the occurrence of severe PEP was evaluated. Notably, the occurrence of severe PEP was not observed in the stent group; however, the occurrence of severe PEP was observed in 8 (1.3%) patients who did not have a PS inserted. Severe PEP occurred significantly less often in the stent group than in the no stent group (OR = 0.24; 95%CI: 0.06-0.94; P = 0.04).
In conclusion, prophylactic PS placement is useful for preventing PEP and severe PEP.
Core tip: Endoscopic retrograde cholangiopancreatography (ERCP) plays a major role in the investigation and treatment of pancreaticobiliary diseases. However, post-ERCP pancreatitis (PEP) is a severe adverse effect. To prevent PEP, prophylactic pancreatic stent (PS) placement was recommended in some randomized controlled trials (RCTs). We performed this meta-analysis that included only RCTs with full-text articles to evaluate the efficacy of prophylactic PS for preventing PEP. As a result, the rates of PEP and severe PEP occurrence were statistically lower in the stent group than in the no stent group. Prophylactic PS was efficient in preventing PEP.
- Citation: Sugimoto M, Takagi T, Suzuki R, Konno N, Asama H, Sato Y, Irie H, Watanabe K, Nakamura J, Kikuchi H, Takasumi M, Hashimoto M, Hikichi T, Ohira H. Pancreatic stents to prevent post-endoscopic retrograde cholangiopancreatography pancreatitis: A meta-analysis. World J Meta-Anal 2019; 7(5): 249-258
- URL: https://www.wjgnet.com/2308-3840/full/v7/i5/249.htm
- DOI: https://dx.doi.org/10.13105/wjma.v7.i5.249
Endoscopic retrograde cholangiopancreatography (ERCP) occupies an important place in the endoscopic treatment and investigation of pancreatic and biliary diseases. However, post-ERCP pancreatitis (PEP) is a severe adverse event. Several past studies have reported that the occurrence of PEP was observed in 0.4%–5.6% of patients[1-8]. Additionally, the fatality rate of PEP was 0%–0.1%[4,6-8].
The risk factors shown to influence PEP occurrence in past reports were previous history of pancreatitis or PEP, two or more pancreatography procedures, sphincter of Oddi dysfunction (SOD), age younger than fifty years, female sex, difficulty of biliary cannulation, biliary sphincter balloon dilation, and precut sphincterotomy[7-15]. However, the usefulness of pancreatic stent (PS) placement for PEP has been reported in these high-risk patients[16-55]. Several prospective randomized controlled trials (RCTs) were discussed in these reports. Some RCTs showed the efficacy of PS placement in preventing PEP[19,20,22,26,27,30,45,51-53,55]. In addition, six meta-analyses were performed on this topic. The insertion of a PS was recommended in all of the meta-analyses[35,38,56-59]. However, the RCTs involved in these meta-analyses were varied. In addition, two meta-analyses involved non-RCTs[38,59]. In a study included in the two meta-analyses, the no stent group was not randomized[31]. Therefore, we performed a meta-analysis limited to full-text articles and excluding any RCTs of special cases (for example, ampullectomy cases, only abstracts, etc.,). In addition, we included new RCTs in this meta-analysis.
We conducted a meta-analysis data search according to PRISMA statement guidelines[60]. MS and TT performed literature retrieval using the MEDLINE, PubMed, Cochrane Library databases. The retrieval was limited to reports written in English. The following keywords were used for the search: “pancreatic stent” and “post-ERCP pancreatitis”.
The studies that met the following criteria were selected: (1) RCTs comparing patients who received a PS for the prevention PEP and patients who did not receive a PS during ERCP; (2) Full-length articles; and (3) Articles written in English. We excluded studies that met the following criteria: (1) Case reports; (2) Case series; (3) Retrospective case control studies; and (4) Studies on endoscopic ampullectomy, because the procedure considerably changes the form of the Vater papilla. Moreover, we performed a manual search of reports cited in the extracted articles to discover any additional reports.
The data extracted were as follows (Tables 1 and 2): (1) Study data (first author, year of publication, country); (2) Patient characteristics (age, sex, number of patients who received a PS, number of patients who did not receive a PS); and (3) Factors related to ERCP procedures (type of PS, success rate of PS insertion, occurrence of PEP, severity of PEP, severity criteria of PEP).
| Ref. | Country | Sample number | Mean age | Sex (male / female) | Patients | |||
| Stent | No stent | Stent | No stent | Stent | No stent | |||
| Smithline et al[55], 1993 | United States | 43 | 50 | 46 | 47 | 19/81 | 22/78 | SOD, CBD < 10 mm |
| Tarnasky et al[51], 1998 | United States | 41 | 39 | 45.7 | 46.4 | NA | NA | SOD |
| Fazel et al[52], 2003 | United States | 38 | 36 | 45.8 | 43.6 | 4/32 | 6/32 | SOD, difficult cannulation |
| Sofuni et al[19], 2007 | Japan | 98 | 103 | 67.0 | 66.0 | 60/38 | 64/38 | NA |
| Tsuchiya et al[20], 2007 | Japan | 32 | 32 | 65.0 | 69.0 | 19/13 | 22/10 | NA |
| Ito et al[22], 2010 | Japan | 35 | 35 | 68 | 70 | 19/16 | 20/15 | Difficult cannulation |
| Sofuni et al[27], 2011 | Japan | 213 | 213 | NA | NA | NA | NA | Risk factors, such as SOD, history of pancreatitis |
| Pan et al[26], 2011 | China | 20 | 20 | 61.0 | 57.0 | 9/11 | 10/10 | High-risk patients |
| Kawaguchi et al[30], 2012 | Japan | 60 | 60 | 66.0 | 68.0 | 27/33 | 25/35 | SOD, previous PEP |
| Lee et al[53], 2012 | South Korea | 50 | 51 | 57.3 | 57.9 | 17/33 | 21/30 | Difficult cannulation |
| Yin et al[45], 2016 | China | 104 | 102 | 57.2 | 57.4 | 59/45 | 55/47 | High-risk patients |
| Ref. | ERCP procedure | Pancreatic stent | Success rate (%) | PEP n (%) stent/ no stent | Criteria of PEP severity |
| Smithline et al[55], 1993 | Precut EST | Double-barbed 5 or 7fr, 2 or 2.5 cm | 90 | Total 6 (14)/9 (18) Mild 5 (12)/5 (10) Moderate 1 (2)/2 (4) Severe 1 (2)/2 (4) | Cotton |
| Tarnasky et al[51], 1998 | EST | 5 or 7Fr, 2 or 2.5 cm | NA | Total 1 (2)/10 (26) Mild 0 (0)/5 (13) Moderate 0 (0)/5 (13) Severe 0 (0)/ 0 (0) | Cotton |
| Fazel et al[52], 2003 | EST | 5fr nasopancreatic catheter or Double-barbed 5fr, 2 cm | 95 | Total 2 (5.3)/10 (28) Mild 2 (5.3)/5 (14) Moderate 0 (0)/2(6) Severe 0 (0)/3 (8) | Cotton |
| Sofuni et al[19], 2007 | EST, EPBD, IDUS, biopsy, sphincter of Oddi manometry, POCS | 5Fr, 3 cm with 2 flanges on the duodenal side | 97 | Total 3 (3)/14 (13.6) Mild 2 (2)/8 (7.8) Moderate 1 (1)/6 (4.6) Severe 0 (0)/0(0) | Cotton |
| Tsuchiya et al[20], 2007 | EST, IDUS, EPBD, sphincter of Oddi manometry | 5fr, 3 or 4 cm duodenal pig tail stent without inner flange | 100 | Total 1 (3.1)/4 (12.5) Mild 1 (3.1)/2 (6.3) Moderate 0 (0)/1 (3.1) Severe 0 (0)/1 (3.1) | Cotton |
| Ito et al[22], 2010 | EST, IDUS, EPBD, biopsy | 5fr, 4 cm with a single duodenal pig tail | 97 | Total 1 (2.9)/8 (23) Mild 1 (2.9)/8 (23) Moderate and severe 0 | Cotton |
| Sofuni et al[27], 2011 | EST, EPBD, ENBD, IDUS, biopsy | 5Fr, 3 cm with 2 flanges on the duodenal side | 88 | Total 20 (9.4)/31 (15.2) Mild 16 (7.5)/22 (14.6) Moderate 4 (1.9)/8 (3.8) Severe 0 (0)/1 (0.5) | Cotton |
| Pan et al[26], 2011 | ERCP | 5fr single pig tail | NA | Total 4 (20)/14 (70) Mild, moderate, severe NA | Cotton |
| Kawaguchi et al[30], 2012 | Precut EST, pancreatic sphincterotomy, biopsy, IDUS | 5fr, 3 cm with two flanges on the duodenal side | 100 | Total 1 (1.7)/8 (13.3) Mild 1 (1.7)/8 (13.3) | Modified Cotton |
| Lee et al[53], 2012 | EST, precut EST, IDUS, biopsy | Unflanged 3fr, 4, 6, or 8 cm duodenal pig tail stent | 96 | Total 6 (12)/15 (29.4) Mild 5 (10)/12 (23.5) Moderate 1 (2)/2 (3.9) Severe 0 (0)/1 (2) | Cotton |
| Yin et al[45], 2016 | EST, EPBD | 5Fr, 5, 7, or 9 cm | NA | Total 8 (7.7)/18 (17.7) Mild, Moderate, severe NA | NA |
The publication bias for the obtained data was assessed using funnel plots.
The meta-analysis was performed using The EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan)[61]. The homogeneity of each study was judged by determining the I2 value. An I2 value ≤ 25% was considered to have no statistical heterogeneity. An I2 value of 25%-50% was treated as low statistical heterogeneity, and an I2 value of 50%-75% was treated as moderate statistical heterogeneity. An I2 value > 75% was considered to have high statistical heterogeneity. A fixed-effects model was used if extracted studies had low heterogeneity. A random-effects model was used if the extracted studies were heterogeneous. A P value < 0.05 indicated a significant difference.
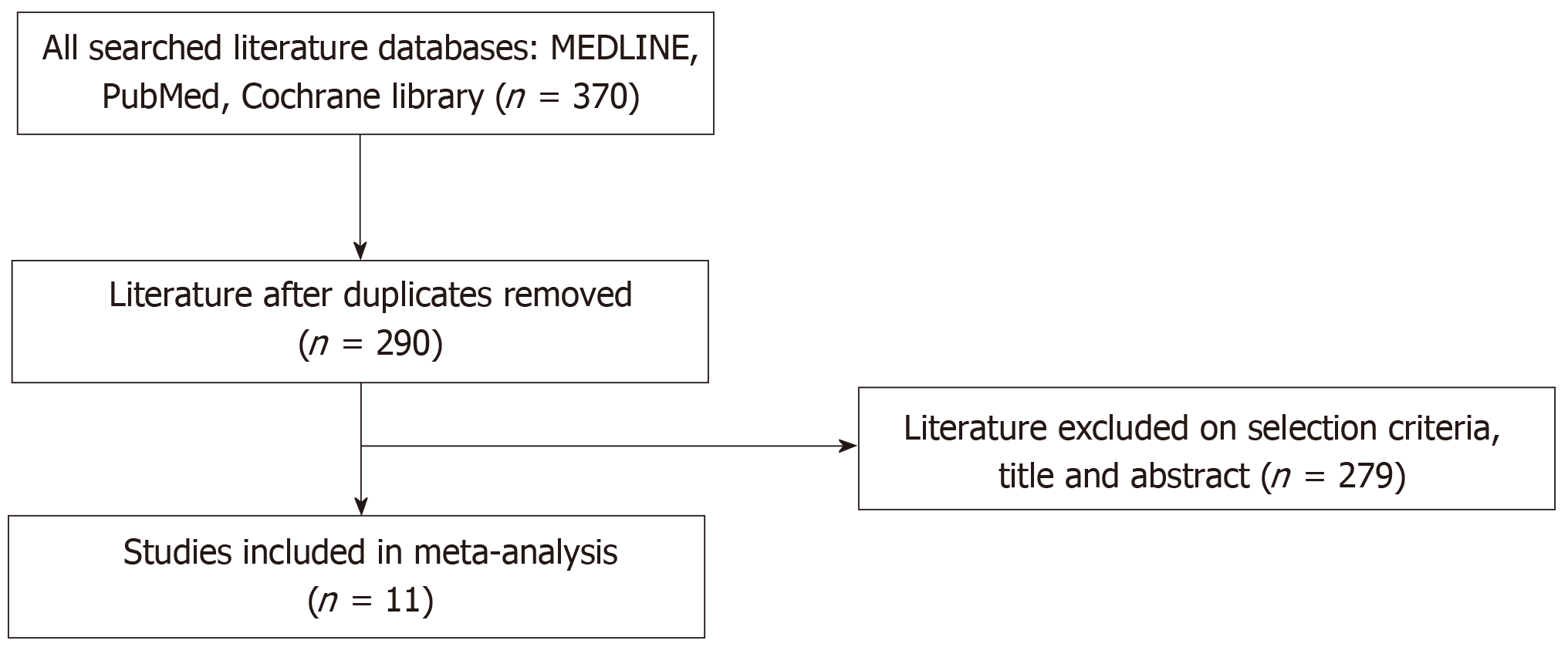
A total of 369 articles were identified by searching MEDLINE, Cochrane Library and PubMed. Of these reports, 80 studies were excluded because of duplication. In addition, 279 studies were excluded according to the selection criteria described above, as determined from the title and abstract. Finally, 11 studies were included in this meta-analysis (Figure 1).
All of these studies were RCTs published between 1993 and 2016. A total of 1475 patients were included in the studies, and of whom, 734 patients underwent insertion of PS, and 741 patients did not have a PS inserted. In some studies, proteinase inhibitors or antibiotics were administered as other prophylaxis; however, rectal indomethacin was not used in any study. All patient characteristics are shown in Table 1, and ERCP-related procedures are shown in Table 2.
In the RCTs, with the exception of two studies by Smithline et al[55] and Fazel et al[52], PEP was defined according to Cotton’s criteria[62]. In these RCTs, new abdominal pain after ERCP with elevated serum amylase no less than three times the normal upper limit in 24 h was diagnosed as PEP. In the study by Smithline et al[55], abdominal pain with elevated serum lipase or amylase no less than two times the normal upper limit was diagnosed as PEP. In the study by Fazel et al[52], epigastric and umbilical pain with elevated serum amylase no less than two times the normal upper limit was diagnosed as PEP.
The severity of PEP was classified according to Cotton’s criteria in almost all RCTs[62] (Table 2). In the criteria, mild pancreatitis was defined as an extension of planned hospitalization of two to three days. Moderate pancreatitis was defined as an extension of planned hospitalization of four to ten days. Severe pancreatitis was defined as an extension of planned hospitalization of more than ten days with or without bleeding or a pseudocyst requiring intervention.
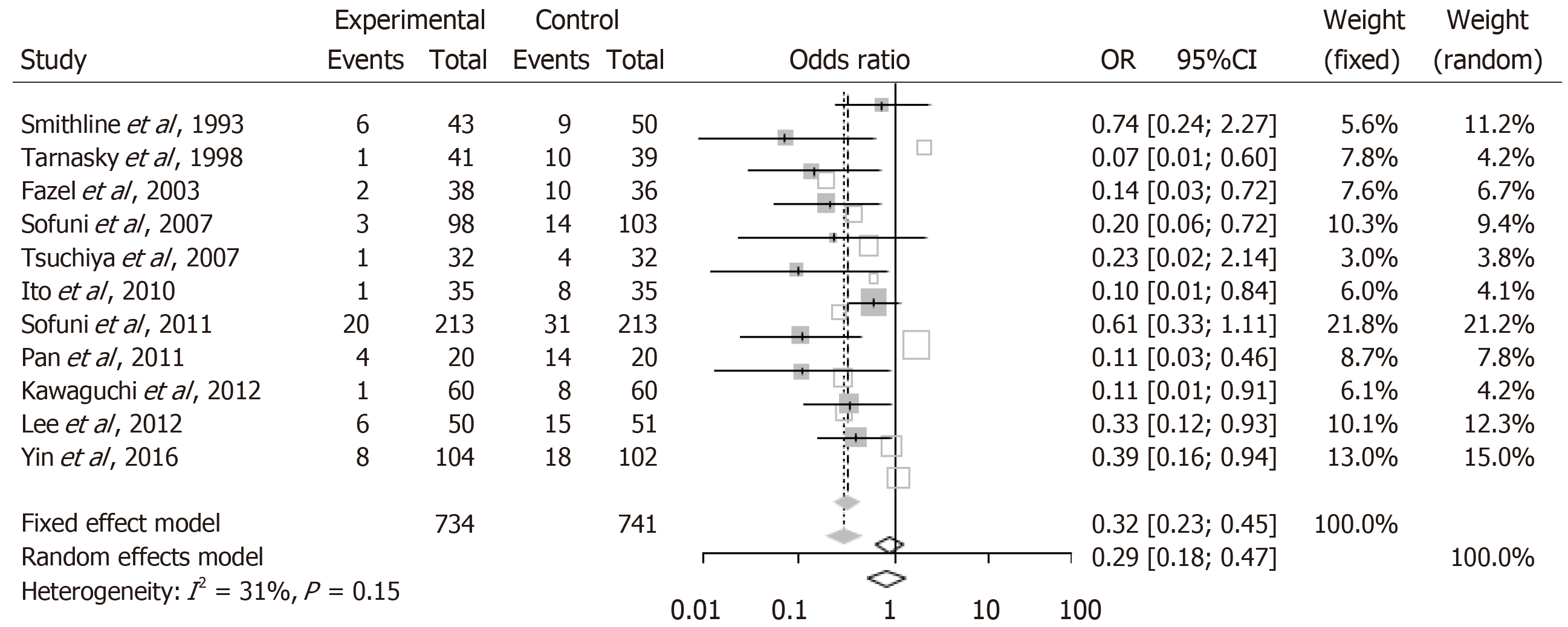
PEP was observed in all studies; it occurred in 39 (5.3%) patients who underwent PS insertion, and on the other hand, it occurred in 141 (19%) patients who did not have a PS inserted. The heterogeneity among the included studies was low (I2 = 31%, P = 0.15); therefore, we selected a fixed-effects model. The occurrence of PEP was significantly lower in patients who received a PS than in the patients who did not receive a PS (OR = 0.32; 95%CI: 0.23-0.45; P < 0.001; Figure 2).
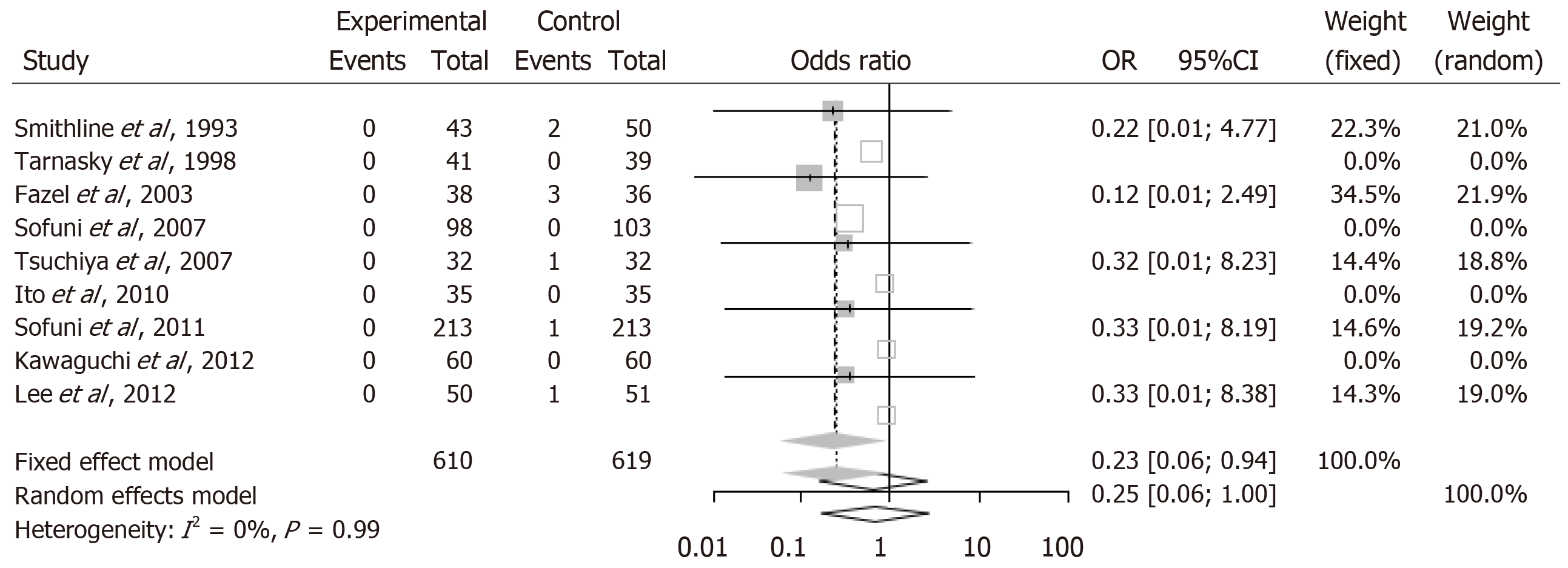
We also evaluated severe PEP between the stent group and the no stent group. The occurrence of severe PEP was not observed in the stent group; however, the occurrence of severe PEP was observed in 8 (1.3%) patients who did not undergo PS insertion. Statistical heterogeneity was not seen in the included studies (I2 = 0%, P = 0.99); therefore, a fixed-effects model was chosen. The occurrence of severe PEP was significantly lower in the stent group than in the no stent group (OR = 0.24; 95%CI: 0.06-0.94; P = 0.04; Figure 3).
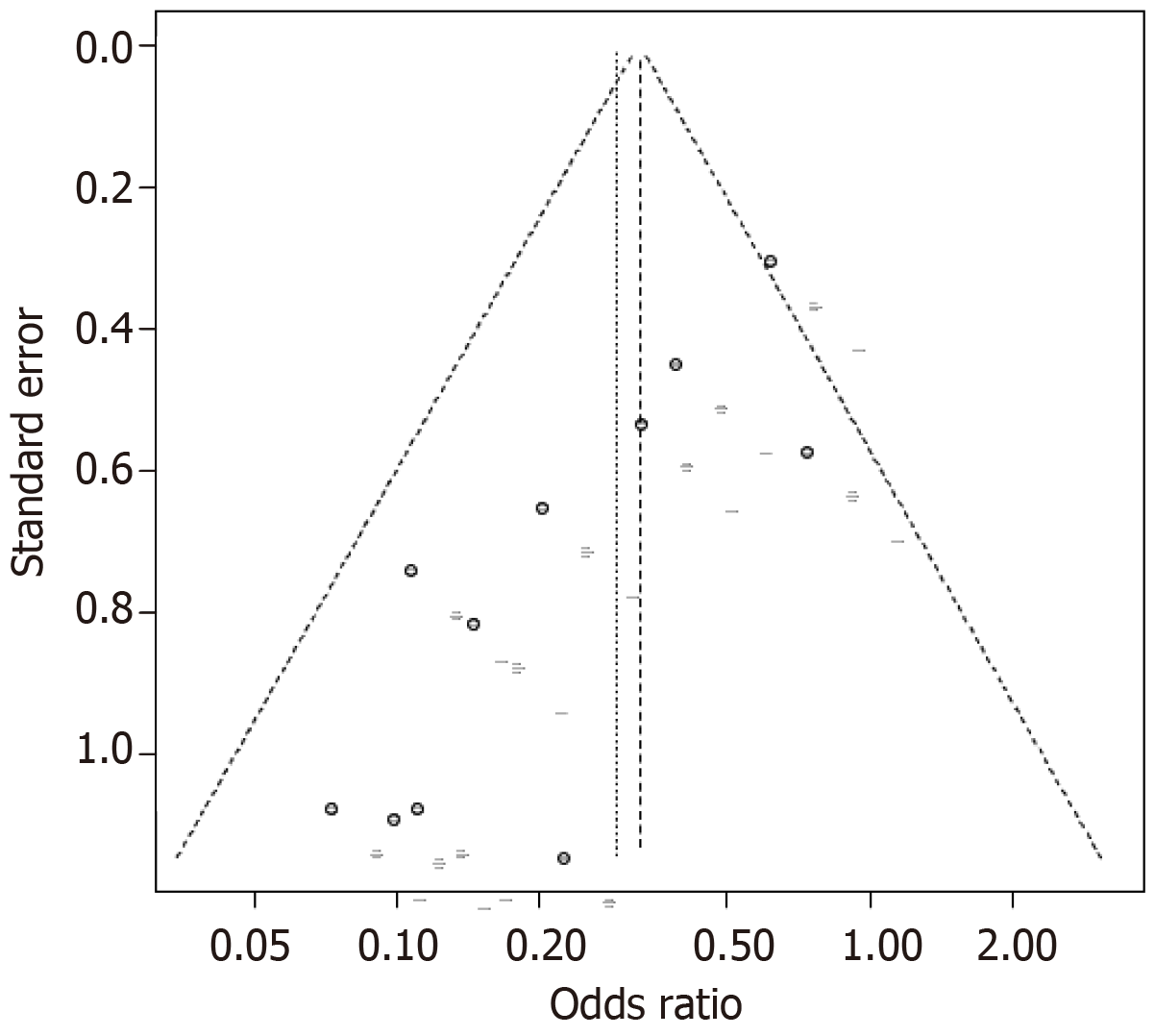
Egger’s test of funnel plot asymmetry showed publication bias (P = 0.009; Figure 4). The funnel plot was asymmetric, and we found that negative studies with a smaller number of subjects were missing.
In this meta-analysis, prophylactic PS placement was efficient for preventing PEP. This result is the same as that in each previous RCT that was included in this meta-analysis. In addition, this meta-analysis proved that prophylactic PS placement prevented the occurrence of severe PEP.
In the eleven RCTs in this meta-analysis, ten RCTs indicated that prophylactic PS placement decreased the occurrence of PEP[19,20,22,26,27,30,45,51-53]. However, Smithline et al[55] reported that prophylactic main pancreatic duct stenting is not recommended for the prevention of PEP[55]. The different results among the RCTs was influenced by the small sample size. In addition, there were far fewer patients with severe PEP. Therefore, the occurrence of severe PEP was not significantly different between the stent group and the no stent group in any of the included studies. On the other hand, severe PEP was not observed in the stent group in the included RCTs. These results indicated that prophylactic PS might prevent not only total PEP but also severe PEP.
The efficacy of prophylactic PS for preventing severe PEP was not statistically proven in any RCT. However, six meta-analyses were previously performed on prophylactic PS to prevent PEP. Additionally, two of the six meta-analyses also reported that prophylactic PS did not significantly prevent severe PEP[56,58]. As more cases about prophylactic PS were reported, two meta-analyses performed by Mazaki et al[57,59] proved that prophylactic PS was efficient for preventing severe PEP. The second recent meta-analysis was carried out by Shi et al[35] and involved only full-text articles and excluded reports with only abstracts. However, the efficacy of prophylactic PS for preventing severe PEP was not shown in the meta-analysis. In the current meta-analysis, we included only full-text articles. As a result, PS was found to be efficient for preventing severe PEP. The addition of new RCTs and exclusion of RCTs on special cases such as ampullectomy[63] may have contributed to the definitive results of this meta-analysis.
This study has some limitations. First, all RCTs involved in this meta-analysis were written in English. Second, the type of PS was different in each RCT. Third, publication bias existed in this study. In the future, we hope that the accumulation of a greater number of relevant RCTs will overcome this bias.
In conclusion, prophylactic PS was useful for preventing not only PEP but also severe PEP.
Endoscopic retrograde cholangiopancreatography (ERCP) occupies an important place in the endoscopic treatment and investigation of pancreatic and biliary diseases. However, post-ERCP pancreatitis (PEP) is a severe adverse effect. To prevent PEP, prophylactic pancreatic stent (PS) placement has been recommended based on the results of several randomized controlled trials (RCTs).
Prior meta-analyses have shown that prophylactic PS was useful for preventing PEP. However, abstract reports and patients who underwent endoscopic ampullectomy were included in the previous analyses. The efficacy of PS for preventing severe PEP was different in each meta-analysis. Therefore, we performed the current meta-analysis, which included only full-text articles, and added new findings.
In this meta-analysis, we evaluated the efficacy of prophylactic PS for the prevention of PEP.
We identified the included RCTs by searching MEDLINE, Cochrane Library and PubMed. Among the retrieved reports, 11 studies were included in this meta-analysis. The occurrence of PEP and severe PEP was evaluated.
The rates of PEP and severe PEP occurrence were significantly lower in patients who received a PS than in patients who did not receive a PS.
Prophylactic PS was useful not only for preventing PEP but also for preventing severe PEP.
This meta-analysis proved that prophylactic PS prevented severe PEP. This result will contribute to a reduction in PEP and severe PEP in patients undergoing ERCP.
| 1. | Reiertsen O, Skjøtø J, Jacobsen CD, Rosseland AR. Complications of fiberoptic gastrointestinal endoscopy--five years' experience in a central hospital. Endoscopy. 1987;19:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 91] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Sherman S, Hawes RH, Rathgaber SW, Uzer MF, Smith MT, Khusro QE, Silverman WB, Earle DT, Lehman GA. Post-ERCP pancreatitis: randomized, prospective study comparing a low- and high-osmolality contrast agent. Gastrointest Endosc. 1994;40:422-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 57] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Johnson GK, Geenen JE, Bedford RA, Johanson J, Cass O, Sherman S, Hogan WJ, Ryan M, Silverman W, Edmundowicz S. A comparison of nonionic versus ionic contrast media: results of a prospective, multicenter study. Midwest Pancreaticobiliary Study Group. Gastrointest Endosc. 1995;42:312-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 60] [Article Influence: 1.9] [Reference Citation Analysis (1)] |
| 4. | Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ, Lande JD, Pheley AM. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1716] [Cited by in RCA: 1703] [Article Influence: 56.8] [Reference Citation Analysis (2)] |
| 5. | Loperfido S, Angelini G, Benedetti G, Chilovi F, Costan F, De Berardinis F, De Bernardin M, Ederle A, Fina P, Fratton A. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc. 1998;48:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 801] [Cited by in RCA: 782] [Article Influence: 27.9] [Reference Citation Analysis (1)] |
| 6. | Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, Spirito F, Pilotto A, Forlano R. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007;102:1781-1788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 669] [Cited by in RCA: 799] [Article Influence: 42.1] [Reference Citation Analysis (0)] |
| 7. | Glomsaker T, Hoff G, Kvaløy JT, Søreide K, Aabakken L, Søreide JA; Norwegian Gastronet ERCP Group. Patterns and predictive factors of complications after endoscopic retrograde cholangiopancreatography. Br J Surg. 2013;100:373-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 102] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 8. | Katsinelos P, Lazaraki G, Chatzimavroudis G, Gkagkalis S, Vasiliadis I, Papaeuthimiou A, Terzoudis S, Pilpilidis I, Zavos C, Kountouras J. Risk factors for therapeutic ERCP-related complications: an analysis of 2,715 cases performed by a single endoscopist. Ann Gastroenterol. 2014;27:65-72. [PubMed] |
| 9. | Chen JJ, Wang XM, Liu XQ, Li W, Dong M, Suo ZW, Ding P, Li Y. Risk factors for post-ERCP pancreatitis: a systematic review of clinical trials with a large sample size in the past 10 years. Eur J Med Res. 2014;19:26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 99] [Cited by in RCA: 92] [Article Influence: 7.7] [Reference Citation Analysis (1)] |
| 10. | Cotton PB, Garrow DA, Gallagher J, Romagnuolo J. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc. 2009;70:80-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 449] [Cited by in RCA: 485] [Article Influence: 28.5] [Reference Citation Analysis (0)] |
| 11. | Leghari A, Ghazanfar S, Qureshi S, Taj MA, Niaz SK, Quraishy MS. Frequency and risk factors in the post-ERCP pancreatitis in a tertiary care centre. J Coll Physicians Surg Pak. 2013;23:620-624. [PubMed] |
| 12. | Liu Y, Su P, Lin S, Xiao K, Chen P, An S, Zhi F, Bai Y. Endoscopic papillary balloon dilatation versus endoscopic sphincterotomy in the treatment for choledocholithiasis: a meta-analysis. J Gastroenterol Hepatol. 2012;27:464-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 49] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 13. | Masci E, Mariani A, Curioni S, Testoni PA. Risk factors for pancreatitis following endoscopic retrograde cholangiopancreatography: a meta-analysis. Endoscopy. 2003;35:830-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 275] [Cited by in RCA: 287] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 14. | Weinberg BM, Shindy W, Lo S. Endoscopic balloon sphincter dilation (sphincteroplasty) versus sphincterotomy for common bile duct stones. Cochrane Database Syst Rev. 2006;CD004890. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 87] [Article Influence: 4.4] [Reference Citation Analysis (1)] |
| 15. | Zhao HC, He L, Zhou DC, Geng XP, Pan FM. Meta-analysis comparison of endoscopic papillary balloon dilatation and endoscopic sphincteropapillotomy. World J Gastroenterol. 2013;19:3883-3891. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 50] [Cited by in RCA: 62] [Article Influence: 4.8] [Reference Citation Analysis (1)] |
| 16. | Kingsnorth A. Role of cytokines and their inhibitors in acute pancreatitis. Gut. 1997;40:1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 119] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 17. | Freeman ML. Pancreatic stents for prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis. Clin Gastroenterol Hepatol. 2007;5:1354-1365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 132] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 18. | Lawrence C, Cotton PB, Romagnuolo J, Payne KM, Rawls E, Hawes RH. Small prophylactic pancreatic duct stents: an assessment of spontaneous passage and stent-induced ductal abnormalities. Endoscopy. 2007;39:1082-1085. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Sofuni A, Maguchi H, Itoi T, Katanuma A, Hisai H, Niido T, Toyota M, Fujii T, Harada Y, Takada T. Prophylaxis of post-endoscopic retrograde cholangiopancreatography pancreatitis by an endoscopic pancreatic spontaneous dislodgement stent. Clin Gastroenterol Hepatol. 2007;5:1339-1346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 113] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 20. | Tsuchiya T, Itoi T, Sofuni A, Itokawa F, Kurihara T, Ishii K, Tsuji S, Kawai T, Moriyasu F. Temporary pancreatic stent to prevent post endoscopic retrograde cholangiopancreatography pancreatitis: a preliminary, single-center, randomized controlled trial. J Hepatobiliary Pancreat Surg. 2007;14:302-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 67] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 21. | Chahal P, Tarnasky PR, Petersen BT, Topazian MD, Levy MJ, Gostout CJ, Baron TH. Short 5Fr vs long 3Fr pancreatic stents in patients at risk for post-endoscopic retrograde cholangiopancreatography pancreatitis. Clin Gastroenterol Hepatol. 2009;7:834-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 63] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 22. | Ito K, Fujita N, Noda Y, Kobayashi G, Obana T, Horaguchi J, Takasawa O, Koshita S, Kanno Y, Ogawa T. Can pancreatic duct stenting prevent post-ERCP pancreatitis in patients who undergo pancreatic duct guidewire placement for achieving selective biliary cannulation? A prospective randomized controlled trial. J Gastroenterol. 2010;45:1183-1191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 110] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 23. | Rao AS, Baron TH. Pancreatic stent placement for prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis: do we need further evidence? No, the defense rests. Endoscopy. 2010;42:870-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Gong B, Sun B, Hao LX, Bie L. Usefulness of an algorithm for endoscopic retrieval of proximally migrated 5Fr and 7Fr pancreatic stents. Hepatobiliary Pancreat Dis Int. 2011;10:196-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Pahk A, Rigaux J, Poreddy V, Smith J, Al-Kawas F. Prophylactic pancreatic stents: does size matter? A comparison of 4-Fr and 5-Fr stents in reference to post-ERCP pancreatitis and migration rate. Dig Dis Sci. 2011;56:3058-3064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Pan XP, Dang T, Meng XM, Xue KC, Chang ZH, Zhang YP. Clinical study on the prevention of post-ERCP pancreatitis by pancreatic duct stenting. Cell Biochem Biophys. 2011;61:473-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 27. | Sofuni A, Maguchi H, Mukai T, Kawakami H, Irisawa A, Kubota K, Okaniwa S, Kikuyama M, Kutsumi H, Hanada K, Ueki T, Itoi T. Endoscopic pancreatic duct stents reduce the incidence of post-endoscopic retrograde cholangiopancreatography pancreatitis in high-risk patients. Clin Gastroenterol Hepatol. 2011;9:851-858; quiz e110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 118] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 28. | Zolotarevsky E, Fehmi SM, Anderson MA, Schoenfeld PS, Elmunzer BJ, Kwon RS, Piraka CR, Wamsteker EJ, Scheiman JM, Korsnes SJ, Normolle DP, Kim HM, Elta GH. Prophylactic 5-Fr pancreatic duct stents are superior to 3-Fr stents: a randomized controlled trial. Endoscopy. 2011;43:325-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 56] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 29. | Enestvedt BK, Ahmad NA. Pancreatic duct stents for the prevention of post ERCP pancreatitis: for all or some? Gastroenterology. 2012;143:493-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 30. | Kawaguchi Y, Ogawa M, Omata F, Ito H, Shimosegawa T, Mine T. Randomized controlled trial of pancreatic stenting to prevent pancreatitis after endoscopic retrograde cholangiopancreatography. World J Gastroenterol. 2012;18:1635-1641. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 39] [Cited by in RCA: 49] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 31. | Cha SW, Leung WD, Lehman GA, Watkins JL, McHenry L, Fogel EL, Sherman S. Does leaving a main pancreatic duct stent in place reduce the incidence of precut biliary sphincterotomy-associated pancreatitis? A randomized, prospective study. Gastrointest Endosc. 2013;77:209-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 32. | Afghani E, Akshintala VS, Khashab MA, Law JK, Hutfless SM, Kim KJ, Lennon AM, Kalloo AN, Singh VK. 5-Fr vs. 3-Fr pancreatic stents for the prevention of post-ERCP pancreatitis in high-risk patients: a systematic review and network meta-analysis. Endoscopy. 2014;46:573-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 33. | Freeman ML. Pancreatic stents for prevention of post-ERCP pancreatitis: the evidence is irrefutable. J Gastroenterol. 2014;49:369-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 34. | Nakahara K, Okuse C, Suetani K, Michikawa Y, Kobayashi S, Otsubo T, Itoh F. Need for pancreatic stenting after sphincterotomy in patients with difficult cannulation. World J Gastroenterol. 2014;20:8617-8623. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 35. | Shi QQ, Ning XY, Zhan LL, Tang GD, Lv XP. Placement of prophylactic pancreatic stents to prevent post-endoscopic retrograde cholangiopancreatography pancreatitis in high-risk patients: a meta-analysis. World J Gastroenterol. 2014;20:7040-7048. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 30] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 36. | Takenaka M, Fujita T, Sugiyama D, Masuda A, Shiomi H, Sugimoto M, Sanuki T, Hayakumo T, Azuma T, Kutsumi H. What is the most adapted indication of prophylactic pancreatic duct stent within the high-risk group of post-endoscopic retrograde cholangiopancreatography pancreatitis? Using the propensity score analysis. J Hepatobiliary Pancreat Sci. 2014;21:275-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 37. | Arain MA, Freeman ML. Pancreatic stent placement remains a cornerstone of prevention of post-ERCP pancreatitis, but it requires specialized techniques. Gastrointest Endosc. 2015;81:156-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 38. | Fan JH, Qian JB, Wang YM, Shi RH, Zhao CJ. Updated meta-analysis of pancreatic stent placement in preventing post-endoscopic retrograde cholangiopancreatography pancreatitis. World J Gastroenterol. 2015;21:7577-7583. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 45] [Cited by in RCA: 46] [Article Influence: 4.2] [Reference Citation Analysis (1)] |
| 39. | Freeman ML. Use of Prophylactic Pancreatic Stents for the Prevention of Post-ERCP Pancreatitis. Gastroenterol Hepatol (N Y). 2015;11:420-422. [PubMed] |
| 40. | Troendle DM, Abraham O, Huang R, Barth BA. Factors associated with post-ERCP pancreatitis and the effect of pancreatic duct stenting in a pediatric population. Gastrointest Endosc. 2015;81:1408-1416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 58] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 41. | Elmunzer BJ, Serrano J, Chak A, Edmundowicz SA, Papachristou GI, Scheiman JM, Singh VK, Varadurajulu S, Vargo JJ, Willingham FF, Baron TH, Coté GA, Romagnuolo J, Wood-Williams A, Depue EK, Spitzer RL, Spino C, Foster LD, Durkalski V; SVI study group and the United States Cooperative for Outcomes Research in Endoscopy (USCORE). Rectal indomethacin alone versus indomethacin and prophylactic pancreatic stent placement for preventing pancreatitis after ERCP: study protocol for a randomized controlled trial. Trials. 2016;17:120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 60] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 42. | Fujisawa T, Kagawa K, Ochiai K, Hisatomi K, Kubota K, Sato H, Nakajima A, Matsuhashi N. Prophylactic Efficacy of 3- or 5-cm Pancreatic Stents for Preventing Post-ERCP Pancreatitis: A Prospective, Randomized Trial. J Clin Gastroenterol. 2016;50:e30-e34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (1)] |
| 43. | Li GD, Jia XY, Dong HY, Pang QP, Zhai HL, Zhang XJ, Guo R, Dong YC, Qin CY. Pancreatic Stent or Rectal Indomethacin-Which Better Prevents Post-ERCP Pancreatitis?: A Propensity Score Matching Analysis. Medicine (Baltimore). 2016;95:e2994. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 44. | Tse F, Yuan Y, Bukhari M, Leontiadis GI, Moayyedi P, Barkun A. Pancreatic duct guidewire placement for biliary cannulation for the prevention of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis. Cochrane Database Syst Rev. 2016;CD010571. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 45. | Yin HK, Wu HE, Li QX, Wang W, Ou WL, Xia HH. Pancreatic Stenting Reduces Post-ERCP Pancreatitis and Biliary Sepsis in High-Risk Patients: A Randomized, Controlled Study. Gastroenterol Res Pract. 2016;2016:9687052. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 46. | Zagalsky D, Guidi MA, Curvale C, Lasa J, de Maria J, Ianniccillo H, Hwang HJ, Matano R. Early precut is as efficient as pancreatic stent in preventing post-ERCP pancreatitis in high-risk subjects - A randomized study. Rev Esp Enferm Dig. 2016;108:258-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 47. | Hwang HJ, Guidi MA, Curvale C, Lasa J, Matano R. Post-ERCP pancreatitis: early precut or pancreatic duct stent? A multicenter, randomized-controlled trial and cost-effectiveness analysis. Rev Esp Enferm Dig. 2017;109:174-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 48. | Olsson G, Lübbe J, Arnelo U, Jonas E, Törnqvist B, Lundell L, Enochsson L. The impact of prophylactic pancreatic stenting on post-ERCP pancreatitis: A nationwide, register-based study. United European Gastroenterol J. 2017;5:111-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 49. | Zhang C, Yang YL, Ma YF, Zhang HW, Li JY, Lin MJ, Shi LJ, Qi CC. The modified pancreatic stent system for prevention of post-ERCP pancreatitis: a case-control study. BMC Gastroenterol. 2017;17:108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 50. | Sugimoto M, Takagi T, Suzuki R, Konno N, Asama H, Sato Y, Irie H, Watanabe K, Nakamura J, Kikuchi H, Waragai Y, Takasumi M, Hikichi T, Ohira H. Pancreatic stents for the prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis should be inserted up to the pancreatic body or tail. World J Gastroenterol. 2018;24:2392-2399. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 51. | Tarnasky PR, Palesch YY, Cunningham JT, Mauldin PD, Cotton PB, Hawes RH. Pancreatic stenting prevents pancreatitis after biliary sphincterotomy in patients with sphincter of Oddi dysfunction. Gastroenterology. 1998;115:1518-1524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 52. | Fazel A, Quadri A, Catalano MF, Meyerson SM, Geenen JE. Does a pancreatic duct stent prevent post-ERCP pancreatitis? A prospective randomized study. Gastrointest Endosc. 2003;57:291-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 211] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 53. | Lee TH, Moon JH, Choi HJ, Han SH, Cheon YK, Cho YD, Park SH, Kim SJ. Prophylactic temporary 3F pancreatic duct stent to prevent post-ERCP pancreatitis in patients with a difficult biliary cannulation: a multicenter, prospective, randomized study. Gastrointest Endosc. 2012;76:578-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 57] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 54. | Sahar N, Ross A, Lakhtakia S, Coté GA, Neuhaus H, Bruno MJ, Haluszka O, Kozarek R, Ramchandani M, Beyna T, Poley JW, Maranki J, Freeman M, Kedia P, Tarnasky P; Pancreatic Stenting Registry Group. Reducing the risk of post-endoscopic retrograde cholangiopancreatography pancreatitis using 4-Fr pancreatic plastic stents placed with common-type guidewires: Results from a prospective multinational registry. Dig Endosc. 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 55. | Smithline A, Silverman W, Rogers D, Nisi R, Wiersema M, Jamidar P, Hawes R, Lehman G. Effect of prophylactic main pancreatic duct stenting on the incidence of biliary endoscopic sphincterotomy-induced pancreatitis in high-risk patients. Gastrointest Endosc. 1993;39:652-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 133] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 56. | Singh P, Das A, Isenberg G, Wong RC, Sivak MV, Agrawal D, Chak A. Does prophylactic pancreatic stent placement reduce the risk of post-ERCP acute pancreatitis? A meta-analysis of controlled trials. Gastrointest Endosc. 2004;60:544-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 210] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 57. | Mazaki T, Masuda H, Takayama T. Prophylactic pancreatic stent placement and post-ERCP pancreatitis: a systematic review and meta-analysis. Endoscopy. 2010;42:842-853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 133] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 58. | Choudhary A, Bechtold ML, Arif M, Szary NM, Puli SR, Othman MO, Pais WP, Antillon MR, Roy PK. Pancreatic stents for prophylaxis against post-ERCP pancreatitis: a meta-analysis and systematic review. Gastrointest Endosc. 2011;73:275-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 191] [Article Influence: 12.7] [Reference Citation Analysis (1)] |
| 59. | Mazaki T, Mado K, Masuda H, Shiono M. Prophylactic pancreatic stent placement and post-ERCP pancreatitis: an updated meta-analysis. J Gastroenterol. 2014;49:343-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 150] [Article Influence: 12.5] [Reference Citation Analysis (1)] |
| 60. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11206] [Cited by in RCA: 11310] [Article Influence: 665.3] [Reference Citation Analysis (0)] |
| 61. | Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant. 2013;48:452-458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9275] [Cited by in RCA: 14478] [Article Influence: 1113.7] [Reference Citation Analysis (0)] |
| 62. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1890] [Cited by in RCA: 2085] [Article Influence: 59.6] [Reference Citation Analysis (2)] |
| 63. | Harewood GC, Pochron NL, Gostout CJ. Prospective, randomized, controlled trial of prophylactic pancreatic stent placement for endoscopic snare excision of the duodenal ampulla. Gastrointest Endosc. 2005;62:367-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 200] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): E
P-Reviewer: Chawla S, Ljubicic N, Lv XP, Sperti C S-Editor: Ji FF L-Editor: A E-Editor: Wu YXJ