Published online Apr 30, 2019. doi: 10.13105/wjma.v7.i4.162
Peer-review started: March 13, 2019
First decision: March 27, 2019
Revised: April 3, 2019
Accepted: April 18, 2019
Article in press: April 18, 2019
Published online: April 30, 2019
Processing time: 49 Days and 19 Hours
Endoscopic sphincterotomy (EST) is widely regarded as the first choice in the management of common bile duct (CBD) stones. However, for some patients, this treatment is not possible. The percutaneous transhepatic balloon dilation (PTBD) technique has been suggested as an alternative but has yet to gain wide acceptance.
To review cases of PTBD for removing CBD stones and explore the safety and efficacy of this treatment.
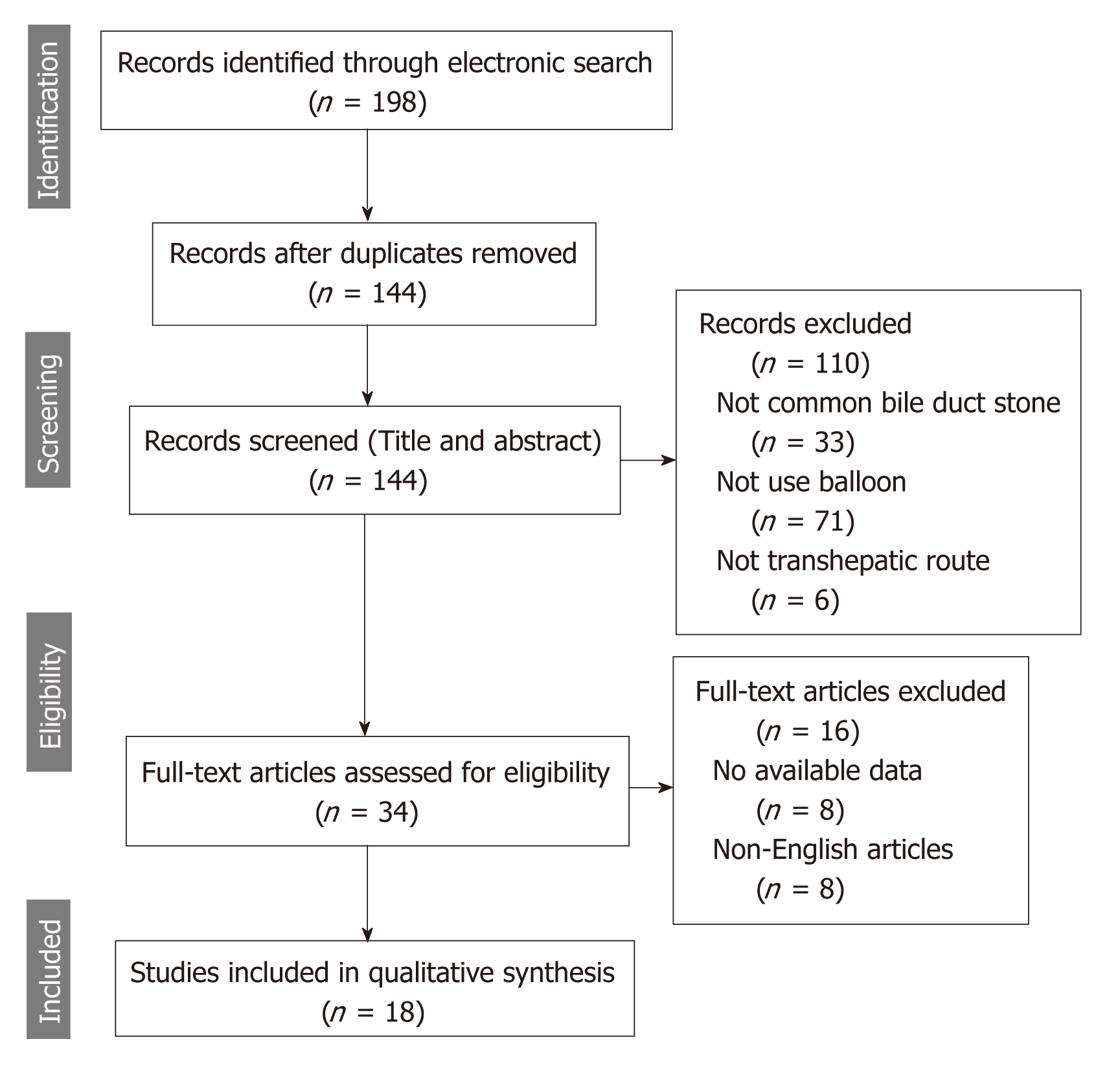
We conducted a systematic review using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. We searched EMBASE, PubMed, and Web of Science for cases of PTBD that underwent CBD stone removal from 1981 to January 2019. We analyzed all relevant articles available in full text. We extracted data on patient’s age, gender, overall technique success rate, reasons for technique failure, and the presence and type of major and minor complications. We analyzed the data and reported the results in a table and text. Altogether, we retrieved 12 case series and 6 case reports, for a total of 1347 patients. Thirty cases were excluded due to a lack of patient data.
The overall technique success rate for removing a CBD stone was 98.5% (1327/1347) and 98.1% (109/111) for removing concurrent CBD and gallbladder stones. Based on available data (n = 1312), mean age of all patients (687 males and 625 females) was 68.9 years. The total number of procedures in the remaining 1317 patients (after exclusion) was 3237 (average 2.4 procedures per patient). The total number of failures for eliminating a CBD stone was 20, and the reasons for failure included: Stone impaction (n = 10), intrahepatic bile duct stricture (n = 5), large stone (n = 2), severe CBD dilation (n = 1), multiple stones (n = 1), and duodenal perforation (n = 1). Various major complications related to the procedure were reported, but the incidence rate was low (1.4%). No pancreatitis or procedure related mortality was reported. Minor complications including transient hyperamylasemia, nausea, vomiting, abdominal pain, fever, and mild hemobilia were reported. For 218 patients (88 patients with unsuccessful endoscopic removal due to anatomical change and large or impacted stone and 130 cases who refused endoscopic procedure due to poor general condition or other additional disease), the CBD stones were successfully pushed into the duodenum by performing the PTBD procedure.
PTBD is a safe and effective approach in the nonoperative management of CBD stones. PTBD provides an alternative treatment when endoscopic procedures fail or are unsuitable for the patient.
Core tip: Endoscopic treatment for common bile duct (CBD) stones has been widely accepted. However, for specific patients, such as those with gastrointestinal anatomical changes, duodenal diverticulum, esophageal varices, or other conditions, endoscopic treatment is unsuitable and difficult to perform. Under these circumstances, it has been shown that percutaneous transhepatic balloon dilation (PTBD) can remove CBD stones via a percutaneous transhepatic route after papilla dilation. However, no review on this technique has been published. Therefore, we performed a systematic review to confirm the safety and efficacy of PTBD in removing CBD stones in terms of the key outcomes, success rate, reasons for failure, and procedure-related complications.
- Citation: Li YL, Li D, Liu B, Wang WJ, Wang W, Wang YZ. Safety and efficacy of percutaneous transhepatic balloon dilation in removing common bile duct stones: A systematic review. World J Meta-Anal 2019; 7(4): 162-169
- URL: https://www.wjgnet.com/2308-3840/full/v7/i4/162.htm
- DOI: https://dx.doi.org/10.13105/wjma.v7.i4.162
Since 1974 when Kawai first described endoscopic sphincterotomy (EST), this treatment has been widely accepted and regarded as the first choice in the management of common bile duct (CBD) stones[1]. Indeed, endoscopic therapies have initiated a great revolution in the treatment of choledocholithiasis[2-4]. However, for specific patients, such as those with gastrointestinal anatomical changes, duodenal diverticulum, esophageal varices, or poor general condition, endoscopic treatment can be difficult to perform, and it has been deemed unsuitable in these particular cases[5-7].
In cases that preclude EST, percutaneous transhepatic stone removal through the papilla into the duodenum without balloon dilation was first reported as an alternative in 1979 by Dotter et al[8] and Perez et al[9]. Further, in 1981 Centola et al[10] first introduced transpapillary elimination of a stone by dilating the papilla with a 6-mm balloon, and since then, this technique has been implemented as a standard percutaneous stone removal procedure. This technique has increased efficacy, with a high success rate and low incidence of complications. Despite these reports, the percutaneous transhepatic balloon dilation (PTBD) technique has still not gained wide acceptance. This is mainly due to a lack of awareness and evaluation of the safety, efficacy, and risk of complications associated with this procedure.
Individual studies alone may not provide strong and sufficient evidence to help PTBD gain greater acceptance, and to the best of our knowledge, no review on the use of PTBD in removing CBD stones has previously been published. In the current review, we aim to objectively evaluate the potential role of PTBD in the management of CBD stones, as an alternative to EST. We performed a systematic review of the currently available literature for success rate, reasons for failure, and procedure-related complications associated with the implementation of the PTBD procedure. This review was conducted in an effort to clarify the safety and efficacy of the procedure.
This systematic review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines[11]. We searched Embase, PubMed, and Web of Science for relevant studies involving the use of PTBD for removal of CBD stones. Our search covered studies conducted during the period from 1981 to January 2019. We used the following Medical Subject Headings (MeSH): “gallstone” and “dilation” and “percutaneous” and “transhepatic” and “balloon”. The complete terms used for the PubMed search were: (dilation [Title/Abstract]) OR dilations [Title/Abstract] OR dilatations [Title/Abstract] OR dilatation [Title/Abstract]) AND (transhepatic [Title/Abstract] OR interventional radiography [Title/Abstract]) AND (percutaneous [Title/Abstract] OR radiography, interventional [Title/Abstract]) AND (balloon [Title/Abstract]) AND (gallstones [Mesh] OR gallstone [Title/Abstract] OR gall Stones [Title/Abstract] OR biliary calculi [Title/Abstract] OR calculi, biliary [Title/Abstract] OR gall Stone [Title/Abstract] OR common bile duct calculi [Title/Abstract] OR gallstones, common bile duct [Title/Abstract] OR common bile duct gallstones [Title/Abstract] OR gall Stones, common bile duct [Title/Abstract] OR biliary calculi, common bile duct [Title/Abstract] OR common bile duct gall stones [Title/Abstract]).
We regarded studies as available for inclusion if they applied a percutaneous transhepatic route, applied a balloon dilation technique, and involved treatment of CBD stones or concurrent CBD stones in addition to gallbladder stones. Case reports and case series were both included. We excluded non-English published studies and studies for which the full text article was unavailable. The studies were reviewed by two individual researchers (DL and BL) and data analysis and extraction were done by the same two researchers (DL and BL). After screening the full text, we extracted the following data from each study for inclusion in our review: Age, gender, number of procedures, overall technique success rate, reasons for failure, and various major and minor complications. Using descriptive statistical analysis, the variables were described as number, proportion, and mean (Table 1).
| Characteristic | Value |
| No. of patients | 1347 |
| Gender | 1312 |
| Female | 625 (47.64) |
| Male | 687 (52.36) |
| Average age | 66.89 |
| Overall technique success rate | 98.51 |
| Average number of procedure | 2.46 |
| Reasons of failure | |
| Severe CBD dilation | 1 (0.07) |
| Multiple stones | 1 (0.07) |
| Large stone | 2 (0.15) |
| Stone impaction | 10 (0.74) |
| Intrahepatic bile duct stricture | 5 (0.37) |
| Duodenal perforation | 1 (0.07) |
| Major complications | |
| Cholangitis | 11 (0.82) |
| Bile duct hemorrhage | 1 (0.07) |
| Subcapsular biloma | 1 (0.07) |
| Subcapsular hematoma | 1 (0.07) |
| Subcapsular abscess | 1 (0.07) |
| Bile peritonitis | 1 (0.07) |
| Duodenal perforation | 1 (0.07) |
| CBD perforation | 1 (0.07) |
| Gastroduodenal artery pseudoaneurysm | 1 (0.07) |
| Right hepatic artery transection | 1 (0.07) |
The search results and flow diagram are shown in Figure 1. We retrieved 12 case series and 6 case reports, for a total of 1347 cases treated by percutaneous transhepatic papilla balloon dilation[10,12-28].
According to our findings, 7 studies were published before the year 2000 and 11 studies were published after the year 2000. Centola et al[10] from England was the first to report a case in which a balloon was used to dilate the papilla and remove a stone in the duodenum in 1981. Among those case series which applied PPBD, the largest included 916 cases and was reported by Shin et al[14] in South Korea in 2017. In our review, 1050 cases were published from Asia, with 297 cases published from Europe and North America.
As for the patient characteristics, not all the studies reported age and sex (n = 35)[16,20,27]. Based on the available data (n = 1312), the average age of patients was 66.89 years and there were 687 males and 625 females. All patients were treated by PTBD for CBD stone removal, and 111 patients who had CBD stones and gallbladder stones concurrently were treated by the combination of PTBD and an additional procedure. Indications cited in these studies for the use of the PTBD procedure to remove stones were: unsuitable for endoscopic procedure due to the poor condition or other additional disease (n = 130), which included coronary artery disease, emphysema, pulmonary insufficiency, cardiac insufficiency, multiple sclerosis, and other diseases, unsuccessful endoscopic removal due to the anatomical change and large or impacted stone (n = 88), and unsuccessful basket extraction (n = 2). Determination of the number of patients treated by an unsuccessful endoscopic procedure or who were unsuitable for an endoscopic proce-dure was low (16.1%), as the largest case series (n = 916) did not mention the other forms of treatment or the patients’ additional diseases.
The overall PTBD technique success rate for removing a CBD stone was 98.5% (1327/1347), and 98.1% (109/111) for removing concurrent CBD and gallbladder stones. The largest diameter of CBD stone was 25 mm reported by Chang et al[13] in 2018, and the CBD stone was successfully removed through dilated papilla by using a 24 mm balloon. Before stone removal, percutaneous transhepatic biliary drainage was conducted on 1024 patients, which is performed to relieve clinical symptoms and build the approach for the stone removal procedure that follows. Based on the available data, the total number of procedures in 1317 patients was 3237, with an average of 2.4 procedures per patient (30 cases did not have this information). The total number of failures in eliminating a CBD stone was 20, and there were multiple reasons for failure, including severe CBD dilation (n = 1), large stone (n = 2), multiple stones (n = 1), stone impaction (n = 10), bile duct stricture (n = 5), and duodenal perforation (n = 1).
Major complications related to the procedure were reported, but the incidence rate for these complications was low (1.4%). Among the included studies, the incidence rate of major complications varied from 0%-6.8%. Major complications included cholangitis (n = 11), bile duct hemorrhage (n = 1), subcapsular biloma (n = 1), subcapsular hematoma (n = 1), subcapsular abscess (n = 1), bile peritonitis (n = 1), duodenal perforation (n = 1), CBD perforation (n = 1), gastroduodenal artery pseudoaneurysm (n = 1), and right hepatic artery transection (n = 1). No pancreatitis or procedure related mortality was reported. Minor complications, such as hyperamylasemia, nausea, vomiting, abdominal pain, fever, and mild hemobilia, were reported. The complete data for these complications were not provided in many case series as most of the minor complications had transient adverse effects and did not require any treatment.
The results of this review show that the use of the PTBD technique in removing CBD stones can yield a high success rate and a low incidence of complications. Furthermore, our findings suggest that PTBD offers a safe and effective choice for removing CBD stones in those patients with a prior failed endoscopic treatment or who are unsuitable for an endoscopic procedure. These data demonstrate and support the PTBD technique as an effective and safe therapeutic management tool, which can be implemented as an alternative, and supplement, to endoscopic therapies.
The overall technique success rate for removing a CBD stone by performing PTBD was 98.5%. The success rate of endoscopic treatment of CBD stones is compromised by several limitations, including gastrointestinal anatomical changes (e.g., Billroth II surgery and duodenal diverticulum) and a limited application in those with a poor general condition. Under these circumstances, endoscopic treatment is unsuitable and difficult to perform. In the current study, the results show that among 218 patients, 88 had unsuccessful endoscopic removal and 130 were unfit for an endoscopic pro-cedure, and the CBD stone was successfully pushed into the duodenum by performing the PTBD procedure. Compared to endoscopic procedures, PTBD uses percutaneous transhepatic and transpapillary routes which could avoid the effects of anatomical changes and is easier to complete the procedure through the papilla. The overall technique success rate for removing concurrent CBD and gallbladder stones was 98.1% (109/111) when performing a combination of the PTBD procedure and another treatment such as laparoscopic choledochotomy (LC) and percutaneous transcystic procedure. Interestingly, in the studies included in our review, there is data suggesting that PTBD + LC is more effective and safe in patients with both CBD and gallbladder stones when compared to the endoscopic papillary balloon dilatation + LC technique. Based on these findings, we postulate that PTBD is an alternative technique that can potentially mitigate the limitations of endoscopic treatment.
Although the success rate of PTBD was quite high, there were a few failed cases. Our results show that the reasons some cases failed were related to the presence of a large stone and duodenal perforation. The large stone is difficult to push through the papilla, which needs use of stone basket or other lithotripsy. And a larger balloon may be used to dilate the papilla, which could cause more abdominal pain and overexpansion of the papilla. For patients with a history of gastrointestinal surgery, it should be performed gently when the guide wire pass through the papilla and the stones were pushed into the duodenum with a balloon. In our systematic review, we conclude several procedure details or key points, which could help surgeons improve their performance with this technique. We suggest the following: (1) In the supine position, puncturing the bile duct in the right anterior lobe under the guidance of B-type ultrasound to make the angle between the bile duct and the CBD as large as possible; (2) After passing through the Oddi sphincter, the stiff guide wire is introduced for greater support; (3) When dilating the Oddi sphincter, the balloon catheter should be accurately positioned and fully dilated. The preferred diameter of the balloon is 8 mm. If the expansion is unsatisfactory, it can be increased by 2 mm successively, with a maximum of 20 mm; (4) Intermittent expansion should be used to avoid tearing of sphincter fibers. We found that the duodenal papilla can be expanded at multiple angles for a duration of 15 s; (5) When the diameter of the stone is > 10 mm, transpapillary stone removal can be achieved by performing lithotripsy first, and then pushing the stone into the duodenum with a balloon; (6) Multiple stones should be rolled out one by one to avoid pancreatitis caused by stone debris reflux to the pancreatic duct. Alternatively, the clinician can leave an external drainage tube for the second stage of stone removal; and (7) Routine placement of internal and external biliary drainage tubes can effectively reduce the incidence of pancreatitis by reducing the intrabiliary pressure. We believe that these suggestions will result in increased efficacy and a further reduction in complications due to the PTBD procedure.
For the 1347 cases we retrieved in this study, major complications related to the PTBD procedure were reported, but the incidence rate was low (1.4%). The most common major complication was cholangitis, at a rate of less than 1% of all cases included in our review. The incidence of other major complications was even lower. Further, we found no reported procedure related mortality. Importantly, the minor complications noted in the results from the included studies were easily controlled by conservative treatment. Several case series (n = 4, 26 patients) reported transient hyperamylasemia after the procedure; however, the level of amylase was decreased to normal after a few days of recovery. These data suggest that PTBD is a safe procedure with a low incidence of complications.
To the best of our knowledge, no review on the effectiveness of the PTBD pro-cedure in removing CBD stones has previously been published. Therefore, we performed this systematic review to confirm the safety and efficacy of PTBD procedure in removing CBD stones by analyzing key outcomes such as success rate, reasons for failure, and procedure-related complications. However, our study had several limitations. First, there are no randomized clinical trials currently published that compare endoscopic treatment and the PTBD procedure. These trials would provide stronger evidence in proving the safety and efficacy of the PTBD procedure as an alternative to endoscopic treatment. However, even given this lack of data, we believe our review fills in some of the blanks that currently exist pertaining to the safety and efficacy of PTBD. Second, long-term effectiveness of this procedure is unknown. There are no long-term follow-up studies published currently, and as such there is no data on any long-term complications, such as stone recurrence and reflux cholangitis. Moreover, there remain no high quality, rigorous manuscripts published on the PTBD procedure. This has resulted in a lack of patient characteristics and incomplete procedure details, which may cause bias. Although further research is required to investigate better application of this treatment, our limited evidence clearly demonstrates that PTBD is a safe and effective approach in the nonoperative management of the CBD stones. This technique provides an alternative treatment when endoscopic procedures fail or are unsuitable for specific patients.
Endoscopic sphincterotomy (EST) is widely regarded as the first choice in the management of common bile duct (CBD) stones. However, for some patients, this treatment is not possible.
The percutaneous transhepatic balloon dilation (PTBD) technique has been suggested as an alternative but has yet to gain wide acceptance.
This review was conducted in an effort to clarify the safety and efficacy of the procedure via reviewing cases of PTBD for removing CBD stones. We conducted a systematic review using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.
We searched EMBASE, PubMed, and Web of Science for cases of PTBD that underwent CBD stone removal from 1981 to January 2019. We analyzed all relevant articles available in full text. We extracted data on patient’s age, gender, overall technique success rate, reasons for technique failure, and the presence and type of major and minor complications.
The overall technique success rate for removing a CBD stone was 98.5% (1327/1347) and 98.1% (109/111) for removing concurrent CBD and gallbladder stones. The total number of failures for eliminating a CBD stone was 20, and the reasons for failure included: Stone impaction (n = 10), intrahepatic bile duct stricture (n = 5), large stone (n = 2), severe CBD dilation (n = 1), multiple stones (n = 1), and duodenal perforation (n = 1).
Various major complications related to the procedure were reported, but the incidence rate was low (1.4%). No pancreatitis or procedure related mortality was reported. Minor complications including transient hyperamylasemia, nausea, vomiting, abdominal pain, fever, and mild hemobilia were reported. For 218 patients (88 patients with unsuccessful endoscopic removal due to anatomical change and large or impacted stone and 130 cases who refused endoscopic procedure due to poor general condition or other additional disease), the CBD stones were successfully pushed into the duodenum by performing the PTBD procedure.
PTBD is a safe and effective approach in the nonoperative management of CBD stones. PTBD provides an alternative treatment when endoscopic procedures fail or are unsuitable for the patient.
We thank Yuan Zhang for her dedicated assistance in statistical analysis of the data.
| 1. | Kawai K, Akasaka Y, Murakami K, Tada M, Koli Y. Endoscopic sphincterotomy of the ampulla of Vater. Gastrointest Endosc. 1974;20:148-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 514] [Cited by in RCA: 460] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 2. | Williams E, Beckingham I, El Sayed G, Gurusamy K, Sturgess R, Webster G, Young T. Updated guideline on the management of common bile duct stones (CBDS). Gut. 2017;66:765-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 280] [Article Influence: 31.1] [Reference Citation Analysis (1)] |
| 3. | Trikudanathan G, Arain MA, Attam R, Freeman ML. Advances in the endoscopic management of common bile duct stones. Nat Rev Gastroenterol Hepatol. 2014;11:535-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Teoh AY, Cheung FK, Hu B, Pan YM, Lai LH, Chiu PW, Wong SK, Chan FK, Lau JY. Randomized trial of endoscopic sphincterotomy with balloon dilation versus endoscopic sphincterotomy alone for removal of bile duct stones. Gastroenterology. 2013;144:341-345.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 97] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 5. | Köksal AŞ, Eminler AT, Parlak E. Biliary endoscopic sphincterotomy: Techniques and complications. World J Clin Cases. 2018;6:1073-1086. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 21] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (6)] |
| 6. | Duan F, Cui L, Bai Y, Li X, Yan J, Liu X. Comparison of efficacy and complications of endoscopic and percutaneous biliary drainage in malignant obstructive jaundice: a systematic review and meta-analysis. Cancer Imaging. 2017;17:27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 80] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 7. | Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ, Lande JD, Pheley AM. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1716] [Cited by in RCA: 1703] [Article Influence: 56.8] [Reference Citation Analysis (2)] |
| 8. | Dotter CT, Bilbao MK, Katon RM. Percutaneous transhepatic gallstone removal by needle tract. Radiology. 1979;133:242-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Perez MR, Oleaga JA, Freiman DB, McLean GL, Ring EJ. Removal of a distal common bile duct stone through percutaneous transhepatic catheterization. Arch Surg. 1979;114:107-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Centola CA, Jander HP, Stauffer A, Russinovich NA. Balloon dilatation of the papilla of Vater to allow biliary stone passage. AJR Am J Roentgenol. 1981;136:613-614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 36] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Preferred Reporting Items for Systematic Reviews and Meta-Analyses. PRISMA statement. Accessed on Sep 10, 2013. Available from: http://www.prisma-statement.org/. |
| 12. | Liu B, Wu DS, Cao PK, Wang YZ, Wang WJ, Wang W, Chang HY, Li D, Li X, Hertzanu Y, Li YL. Percutaneous transhepatic extraction and balloon dilation for simultaneous gallbladder stones and common bile duct stones: A novel technique. World J Gastroenterol. 2018;24:3799-3805. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Chang HY, Wang CJ, Liu B, Wang YZ, Wang WJ, Wang W, Li D, Li YL. Ursodeoxycholic acid combined with percutaneous transhepatic balloon dilation for management of gallstones after elimination of common bile duct stones. World J Gastroenterol. 2018;24:4489-4498. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Shin JS, Shim HJ, Kwak BK, Yoon HK. Biliary stone removal through the percutaneous transhepatic biliary drainage route, focusing on the balloon sphincteroplasty flushing technique: a single center study with 916 patients. Jpn J Radiol. 2017;35:440-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Li D, Li YL, Wang WJ, Liu B, Chang HY, Wang W, Wang YZ, Li Z. Percutaneous transhepatic papilla balloon dilatation combined with a percutaneous transcystic approach for removing concurrent gallbladder stone and common bile duct stone in a patient with billroth II gastrectomy and acute cholecystitis: A case report. Medicine (Baltimore). 2017;96:e7964. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Li S, Li Y, Geng J, Liu B, Gao R, Zhou Z, Hu S. Concurrent Percutaneous Transhepatic Papillary Balloon Dilatation Combined with Laparoscopic Cholecystectomy for the Treatment of Gallstones with Common Bile Duct Stones. J Laparoendosc Adv Surg Tech A. 2015;25:886-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Ozcan N, Kahriman G, Mavili E. Percutaneous transhepatic removal of bile duct stones: results of 261 patients. Cardiovasc Intervent Radiol. 2012;35:621-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 18. | Oguzkurt L, Ozkan U, Gumus B. Percutaneous transhepatic cutting balloon papillotomy for removal of common bile duct stones. Cardiovasc Intervent Radiol. 2009;32:1117-1119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Park YS, Kim JH, Choi YW, Lee TH, Hwang CM, Cho YJ, Kim KW. Percutaneous treatment of extrahepatic bile duct stones assisted by balloon sphincteroplasty and occlusion balloon. Korean J Radiol. 2005;6:235-240. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Nagashima I, Takada T, Shiratori M, Inaba T, Okinaga K. Percutaneous transhepatic papillary balloon dilation as a therapeutic option for choledocholithiasis. J Hepatobiliary Pancreat Surg. 2004;11:252-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 31] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Chikamori F, Kuniyoshi N, Shibuya S, Takase Y. Simultaneous laparoscopic cholecystectomy and percutaneous papillary balloon dilatation for cholecystocholedocholithiasis. Dig Surg. 2003;20:12-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Shirai N, Hanai H, Kajimura M, Kataoka H, Yoshida K, Nakagawara M, Nemoto M, Nagasawa M, Kaneko E. Successful treatment of percutaneous transhepatic papillary dilation in patients with obstructive jaundice due to common bile duct stones after Billroth II gastrectomy: report of two emergent cases. J Clin Gastroenterol. 2000;30:91-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Chikamori F, Nishio S, LeMaster JC. Percutaneous papillary balloon dilatation as a therapeutic option for cholecystocholedocholithiasis in the era of laparoscopic cholecystectomy. Surg Today. 1999;29:856-861. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Graziani L, Fabrizzi G, Manfrini E, Galeazzi R, Freddara U. Percutaneous transhepatic Oddi-sphincter dilatation for bile duct stone removal. AJR Am J Roentgenol. 1989;152:73-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | Berkman WA, Bishop AF, Palagallo GL, Cashman MD. Transhepatic balloon dilation of the distal common bile duct and ampulla of Vater for removal of calculi. Radiology. 1988;167:453-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Saeed M, Newman GE, Dunnick NR. Use of angioplasty balloons in the percutaneous management of biliary calculi: tandem-balloon method. AJR Am J Roentgenol. 1987;148:745-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 27. | Meranze SG, Stein EJ, Burke DR, Hartz WH, McLean GK. Removal of retained common bile duct stones with angiographic occlusion balloons. AJR Am J Roentgenol. 1986;146:383-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 28. | Fataar S, Bassiony H, Abou-Neema T. The percutaneous "stretch and push" technique for removing retained biliary calculi. Br J Radiol. 1982;55:456-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
PRISMA 2009 statement: Guidelines of the PRISMA 2009 Statement have been adopted
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Bramhall S, Espinel J, Kanno Y, Mercado MA, Pan SM S-Editor: Ji FF L-Editor: Wang TQ E-Editor: Wu YXJ